Update on Managing Canine Hyperadrenocorticism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

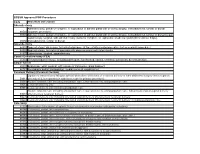
California Proposition 65 Toxicity List
STATE OF CALIFORNIA ENVIRONMENTAL PROTECTION AGENCY OFFICE OF ENVIRONMENTAL HEALTH HAZARD ASSESSMENT SAFE DRINKING WATER AND TOXIC ENFORCEMENT ACT OF 1986 CHEMICALS KNOWN TO THE STATE TO CAUSE CANCER OR REPRODUCTIVE TOXICITY 4-Mar-05 The Safe Drinking Water and Toxic Enforcement Act of 1986 requires that the Governor revise and Chemical Type of Toxicity CAS No. Date Listed A-alpha-C (2-Amino-9H-pyrido[2,3-b]indole) cancer 26148685 1-Jan-90 Acetaldehyde cancer 75070 1-Apr-88 Acetamide cancer 60355 1-Jan-90 Acetazolamide developmental 59665 20-Aug-99 Acetochlor cancer 34256821 1-Jan-89 Acetohydroxamic acid developmental 546883 1-Apr-90 2-Acetylaminofluorene cancer 53963 1-Jul-87 Acifluorfen cancer 62476599 1-Jan-90 Acrylamide cancer 79061 1-Jan-90 Acrylonitrile cancer 107131 1-Jul-87 Actinomycin D cancer 50760 1-Oct-89 Actinomycin D developmental 50760 1-Oct-92 Adriamycin (Doxorubicin hydrochloride) cancer 23214928 1-Jul-87 AF-2;[2-(2-furyl)-3-(5-nitro-2-furyl)]acrylamide cancer 3688537 1-Jul-87 Aflatoxins cancer --- 1-Jan-88 Alachlor cancer 15972608 1-Jan-89 Alcoholic beverages, when associated with alcohol abuse cancer --- 1-Jul-88 Aldrin cancer 309002 1-Jul-88 All-trans retinoic acid developmental 302794 1-Jan-89 Allyl chloride Delisted October 29, 1999 cancer 107051 1-Jan-90 Alprazolam developmental 28981977 1-Jul-90 Altretamine developmental, male 645056 20-Aug-99 Amantadine hydrochloride developmental 665667 27-Feb-01 Amikacin sulfate developmental 39831555 1-Jul-90 2-Aminoanthraquinone cancer 117793 1-Oct-89 p -Aminoazobenzene cancer -

CARE PLAN Electrolyte and Fluid Imbalance
CARE PLAN Electrolyte and Fluid Imbalance . Related to: Check all that apply Endocrine dysfunction Treatment/Drug side effects Urinary difficulties Nutritional deficiency Tissue trauma Renal dysfunction Post-op complications Trauma Other _____________ Status: Achieved/ Progressing/Not Date/Select Outcome Select Interventions Met (comment for negative variances) Serum electrolytes, Perform initial/routine BUN, blood gases will assessments, assess be within desired limits for neurological manifestations indicating electrolyte imbalance. Report findings to clinician (MD, PA, NP) promptly. Implement therapeutic actions (i.e., appropriate diet, administer replacement electrolytes—sodium bicarb, mag sulfate, etc., as ordered) Assess/monitor serum levels of electrolytes; report finding to MD promptly Monitor for associated complications Absence of cardiac Assess/monitor cardiac dysrhythmias rhythm Published by Cinahl Information Systems, a division of EBSCO Information Services. Copyright©2016, Cinahl Information Systems. All rights reserved. No part of this may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the publisher. Cinahl Information Systems accepts no liability for advice or information given herein or errors/omissions in the text. It is merely intended as a general informational overview of the subject for the healthcare professional. Cinahl Information Systems, 1509 Wilson Terrace, -
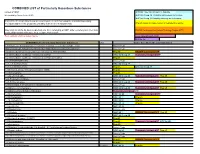
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -

Electrolyte Imbalance in Children with Severe Acute Malnutrition at a Tertiary Care Hospital in Pakistan: a Cross-Sectional Study
Open Access Original Article DOI: 10.7759/cureus.10541 Electrolyte Imbalance in Children With Severe Acute Malnutrition at a Tertiary Care Hospital in Pakistan: A Cross-Sectional Study Mohammad Raza 1, 2 , Sohail Kumar 3 , Muzamil Ejaz 2 , Dua Azim 3 , Saad Azizullah 2 , Azhar Hussain 4, 5 1. Pediatrics, The Indus Hospital, Karachi, PAK 2. Pediatrics, Dow Medical College, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, PAK 3. Internal Medicine, Dow Medical College, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, PAK 4. Healthcare Administration, Franklin University, Columbus, USA 5. Medicine, Xavier University School of Medicine, Oranjestad, ABW Corresponding author: Mohammad Raza, [email protected] Abstract Background Malnutrition is a significant public health concern and a leading contributor to the global burden of children’s diseases, affecting 50 to 150 million children under the age of five years worldwide. Globally, undernutrition accounts for approximately 33% of the deaths among under-fives. South Asia alone contributes to 50% and 38.8% of the world’s population of wasted and stunted children, respectively. In Pakistan, malnutrition is the leading cause of childhood mortality, accounting for nearly 35% of all deaths under five years of age. Severe acute malnutrition (SAM), the most severe form of malnutrition, is often associated with electrolyte imbalances. This study aimed to determine the frequency of electrolyte imbalance in children with SAM admitted at a tertiary care hospital. Methods This cross-sectional study includes 184 patients with SAM aged between 6 and 60 months, who were admitted at the inpatient Department of Pediatrics, Dr. Ruth K. -

ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis
ORIGINAL ARTICLE ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis Naykky Singh Ospina,* Alaa Al Nofal,* Irina Bancos, Asma Javed, Khalid Benkhadra, Ekta Kapoor, Aida N. Lteif, Neena Natt, and M. Hassan Murad Evidence-Based Practice Research Program (N.S.O., A.A.N., K.B., M.H.M.), Mayo Clinic, Rochester, Downloaded from https://academic.oup.com/jcem/article/101/2/427/2810551 by guest on 29 September 2021 Minnesota; Knowledge and Evaluation Research Unit (N.S.O., K.B., M.H.M.), Mayo Clinic, Rochester, Minnesota; Division of Endocrinology, Diabetes, Metabolism, and Nutrition (N.S.O., N.N., I.B.), Mayo Clinic, Rochester, Minnesota; Division of Pediatric Endocrinology and Metabolism (A.A.N., A.J., A.N.L.), Mayo Clinic, Rochester, Minnesota; Division of General Internal Medicine (E.K.), Mayo Clinic, Rochester, Minnesota 55905 Context: The diagnosis of adrenal insufficiency is clinically challenging and often requires ACTH stimulation tests. Objective: To determine the diagnostic accuracy of the high- (250 mcg) and low- (1 mcg) dose ACTH stimulation tests in the diagnosis of adrenal insufficiency. Methods: We searched six databases through February 2014. Pairs of independent reviewers se- lected studies and appraised the risk of bias. Diagnostic association measures were pooled across studies using a bivariate model. Data Synthesis: For secondary adrenal insufficiency, we included 30 studies enrolling 1209 adults and 228 children. High- and low-dose ACTH stimulation tests had similar diagnostic accuracy in adults and children using different peak serum cortisol cutoffs. In general, both tests had low sensitivity and high specificity resulting in reasonable likelihood ratios for a positive test (adults: high dose, 9.1; low dose, 5.9; children: high dose, 43.5; low dose, 7.7), but a fairly suboptimal likelihood ratio for a negative test (adults: high dose, 0.39; low dose, 0.19; children: high dose, 0.65; low dose, 0.34). -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

SNAP Cortisol Testing Guide
SNAP® Cortisol Testing Guide Diagnosing and Treating Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease IMPORTANT: Review history of any administration of corticosteroids as these may influence the reported results. Diagnose ACTH Stimulation Test Diagnostic Protocol for Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism or Addison’s disease Draw baseline cortisol sample. Perform an ACTH stimulation test with Cortrosyn® 5 µg/kg IV or ACTH gel 2.2 U/kg IM. Draw 1-hour cortisol (Cortrosyn®) or 1 and 2-hour cortisol (ACTH gel). Pre-ACTH: 2–6 µg/dL Pre- and Post-ACTH Post-ACTH Post-ACTH Post-ACTH 2 6 µg/dL >22 µg/dL <2 µg/dL – Post-ACTH: 6–18 µg/dL 18–22 µg/dL If both results are <2 µg/dL, results are Equivocal, Consistent Inconclusive consistent with Normal Cushing’s possible with Cushing’s hypoadrenocorticism Perform high-dose dexamethasone* Begin treatment with suppression to mineralocorticoid discriminate between and/or glucocorticoid PDH and ATH, as appropriate. ACTH level and/or abdominal ultrasound. * Do not exceed 0.1 mg/kg of dexamethasone. Diagnose Low-Dose Dexamethasone Suppression Protocol For Cases of Suspected Canine Hyperadrenocorticism History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism Draw baseline cortisol sample. Perform a low-dose dexamethasone suppression test with 0.01 mg/kg of dexamethasone IV. Draw 4-hour -

WO 2018/190970 Al 18 October 2018 (18.10.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/190970 Al 18 October 2018 (18.10.2018) W !P O PCT (51) International Patent Classification: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, CI2Q 1/32 (2006.01) UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (21) International Application Number: EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, PCT/US2018/021 109 MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, (22) International Filing Date: TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, 06 March 2018 (06.03.2018) KM, ML, MR, NE, SN, TD, TG). (25) Filing Language: English Declarations under Rule 4.17: (26) Publication Langi English — as to applicant's entitlement to apply for and be granted a patent (Rule 4.1 7(H)) (30) Priority Data: — as to the applicant's entitlement to claim the priority of the 62/484,141 11 April 2017 ( 11.04.2017) US earlier application (Rule 4.17(Hi)) (71) Applicant: REGENERON PHARMACEUTICALS, Published: INC. [US/US]; 777 Old Saw Mill River Road, Tarrytown, — with international search report (Art. 21(3)) New York 10591-6707 (US). — with sequence listing part of description (Rule 5.2(a)) (72) Inventors: STEVIS, Panayiotis; 777 Old Saw Mill Riv er Road, Tarrytown, New York 10591-6707 (US). -

Download Our Summer 2010 Newsletter
A n e w s l e t t e r f o r r e f e r r i n g veterinarians JOIN US IN 2011 AS WE CELEBRATE METROPOLITAN VETERINARY ASSOCIATES 25 P roviding emergency care & specialized veterinary services YEARS INSID E: p2-3 WELCOME TO Trilostane for the Treatment of Canine the fourth edition of our newsletter Hyperadrenocorticism – The Answer to Our Problems? Established in 1986, Metropolitan Veterinary Associates & Emergency Services p4 is a veterinary group that provides referral veterinary services. We concentrate Pet Loss Support Group & Monthly Lecture Series on specialty and emergency cases, allowing us to dedicate high-level care to the following disciplines: behavior, cardiology, dentistry, dermatology, I NSERT: emergency, internal medicine, neurology, ophthalmology, radiology front (including CT and MRI) and surgery. Meet our internal medicine team In order to maintain a high level of patient care, MVA moved into a newly back renovated 18,000 square foot facility with state-of-the-art diagnostic and Join us for CE therapeutic equipment in 2006. If you haven’t been able to visit our practice, we hope you can join us at one of the upcoming hospital lectures mentioned on page 4. Please enjoy this newsletter and let us know of any topics of interest you’d like to see explored in future editions. We’ve made it easier to contact us. Catch us 24 HOURS A DAY at 610/666/1050! (our primary phone number) DID YOU KNOW? TRILOSTANE FOR THE TREATMENT OF ! CANINE HYPERADRENOCORTICISM – THE ANSWER TO OUR PROBLEMS? By: Damon B. -
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative