Download Our Summer 2010 Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

California Proposition 65 Toxicity List
STATE OF CALIFORNIA ENVIRONMENTAL PROTECTION AGENCY OFFICE OF ENVIRONMENTAL HEALTH HAZARD ASSESSMENT SAFE DRINKING WATER AND TOXIC ENFORCEMENT ACT OF 1986 CHEMICALS KNOWN TO THE STATE TO CAUSE CANCER OR REPRODUCTIVE TOXICITY 4-Mar-05 The Safe Drinking Water and Toxic Enforcement Act of 1986 requires that the Governor revise and Chemical Type of Toxicity CAS No. Date Listed A-alpha-C (2-Amino-9H-pyrido[2,3-b]indole) cancer 26148685 1-Jan-90 Acetaldehyde cancer 75070 1-Apr-88 Acetamide cancer 60355 1-Jan-90 Acetazolamide developmental 59665 20-Aug-99 Acetochlor cancer 34256821 1-Jan-89 Acetohydroxamic acid developmental 546883 1-Apr-90 2-Acetylaminofluorene cancer 53963 1-Jul-87 Acifluorfen cancer 62476599 1-Jan-90 Acrylamide cancer 79061 1-Jan-90 Acrylonitrile cancer 107131 1-Jul-87 Actinomycin D cancer 50760 1-Oct-89 Actinomycin D developmental 50760 1-Oct-92 Adriamycin (Doxorubicin hydrochloride) cancer 23214928 1-Jul-87 AF-2;[2-(2-furyl)-3-(5-nitro-2-furyl)]acrylamide cancer 3688537 1-Jul-87 Aflatoxins cancer --- 1-Jan-88 Alachlor cancer 15972608 1-Jan-89 Alcoholic beverages, when associated with alcohol abuse cancer --- 1-Jul-88 Aldrin cancer 309002 1-Jul-88 All-trans retinoic acid developmental 302794 1-Jan-89 Allyl chloride Delisted October 29, 1999 cancer 107051 1-Jan-90 Alprazolam developmental 28981977 1-Jul-90 Altretamine developmental, male 645056 20-Aug-99 Amantadine hydrochloride developmental 665667 27-Feb-01 Amikacin sulfate developmental 39831555 1-Jul-90 2-Aminoanthraquinone cancer 117793 1-Oct-89 p -Aminoazobenzene cancer -
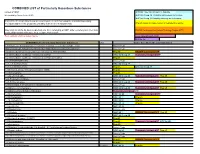
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -
WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

WO 2018/190970 Al 18 October 2018 (18.10.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/190970 Al 18 October 2018 (18.10.2018) W !P O PCT (51) International Patent Classification: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, CI2Q 1/32 (2006.01) UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (21) International Application Number: EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, PCT/US2018/021 109 MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, (22) International Filing Date: TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, 06 March 2018 (06.03.2018) KM, ML, MR, NE, SN, TD, TG). (25) Filing Language: English Declarations under Rule 4.17: (26) Publication Langi English — as to applicant's entitlement to apply for and be granted a patent (Rule 4.1 7(H)) (30) Priority Data: — as to the applicant's entitlement to claim the priority of the 62/484,141 11 April 2017 ( 11.04.2017) US earlier application (Rule 4.17(Hi)) (71) Applicant: REGENERON PHARMACEUTICALS, Published: INC. [US/US]; 777 Old Saw Mill River Road, Tarrytown, — with international search report (Art. 21(3)) New York 10591-6707 (US). — with sequence listing part of description (Rule 5.2(a)) (72) Inventors: STEVIS, Panayiotis; 777 Old Saw Mill Riv er Road, Tarrytown, New York 10591-6707 (US). -

Chemical Muscle Enhancement (The BDR) by Author L
Chemical Muscle Enhancement (The BDR) By Author L. Rea TABLE OF CONTENTS 1. AAS INTRODUCTION ..PG’S 1-12 WARNING: READ FIRST OVER 20 YEARS AGO... WHY STEROIDS AND WHAT IS POSSIBLE? WHAT ARE STEROIDS? FEMALE HORMONE SYNTHESIS MALE HORMONE SYNTHESIS TESTOSTERONE... WHAT DOES IT DO? STEROIDS INCREASE PC SYNTHESIS STEROIDS EFFECT BLOOD VOLUME WHAT HAPPENS AFTER TESTOSTERONE MOLECULES LEAVE RECEPTORS? STEROIDS...GROWTH ON THE CELULAR LEVEL 2. DRUG REFERENCES AND DESCRIPTIONS..PG 12 ORAL ANABOLIC / ANDROGENIC STEROIDS..PG’S 13-30 INJECTABLE ANABOLIC / ANDROGENIC STEROIDS..PG’S 31-45 TESTOSTERONE AND ITS ESTERS..PG’S 45-61 NORTESTOSTERONE (NANDROLONE) AND ITS ESTER..PG’S 62-70 TRENBOLONE AND DERIVATIVES..PG’S 71-78 ESTROGEN CONTROL AND HPTA REGENERATION DRUGS..PG’S 79-94 DIURETICS..PG’S 95-102 THYROID HORMONES ..PG’S 103-116 NON-AAS GROWTH FACTORS AND RELATED SUBSTANCES..PG’S 117-141 OTHER SUBSTANCES..PG’S 142-152 3. REPORTED CYCLES AND EFFECTS.. (Introduction) PG’S 153-159 REPORTED CYCLES AND EFFECTS EXAMPLES (MALE)...PG’S 160-169 REPORTED CYCLES AND EFFECTS EXAMPLES (FEMALE)...PG’S 170-174 REPORTED ADVANCED CYCLES AND EFFECTS-BLITZ CYCLES..PG’S 175-200 (More Reported Cycles and Effects) 4. NUTRITION..PG’S..201-211 5. SUPPLEMENTAL CREATINE..PG’S 212-216 6. REFERENCES AND AVAILABLE LITERATURE..PG’S 217-223 All Rights Reserved CHEMICAL MUSCLE ENHANCEMENT (The Report) and BODYBUILDERS DESK REFERENCE COPYRIGHT ©2002 by AUTHOR L. REA No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical including photocopy, recording, or by any information storage and retrieval system, without the permission in writing of the author and publisher. -

Order in Council 1243/1995
PROVINCE OF BRITISH COLUMBIA ORDER OF THE LIEUTENANT GOVERNOR IN COUNCIL Order in Council No. 12 4 3 , Approved and Ordered OCT 121995 Lieutenant Governor Executive Council Chambers, Victoria On the recommendation of the undersigned, the Lieutenant Governor, by and with the advice and consent of the Executive Council, orders that Order in Council 1039 made August 17, 1995, is rescinded. 2. The Drug Schedules made by regulation of the Council of the College of Pharmacists of British Columbia, as set out in the attached resolution dated September 6, 1995, are hereby approved. (----, c" g/J1"----c- 4- Minister of Heal fandand Minister Responsible for Seniors Presidin Member of the Executive Council (This pan is for adnwustratlye purposes only and is not part of the Order) Authority under which Order Is made: Act and section:- Pharmacists, Pharmacy Operations and Drug Scheduling Act, section 59(2)(1), 62 Other (specify): - Uppodukoic1enact N6145; Resolution of the Council of the College of Pharmacists of British Columbia ("the Council"), made by teleconference at Vancouver, British Columbia, the 6th day of September 1995. RESOLVED THAT: In accordance with the authority established in Section 62 of the Pharmacists, Pharmacy Operations and Drug Scheduling Act of British Columbia, S.B.C. Chapter 62, the Council makes the Drug Schedules by regulation as set out in the attached schedule, subject to the approval of the Lieutenant Governor in Council. Certified a true copy Linda J. Lytle, Phr.) Registrar DRUG SCHEDULES to the Pharmacists, Pharmacy Operations and Drug Scheduling Act of British Columbia The Drug Schedules have been printed in an alphabetical format to simplify the process of locating each individual drug entry and determining its status in British Columbia. -

Ep 2446888 A2
(19) & (11) EP 2 446 888 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 02.05.2012 Bulletin 2012/18 A61K 31/569 (2006.01) (21) Application number: 11010272.0 (22) Date of filing: 12.07.2006 (84) Designated Contracting States: (71) Applicant: DMI Biosciences, Inc. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Englewood, CO 80110-3948 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI SK TR (72) Inventor: Bar-Or, David Designated Extension States: Englewood, Colorado 80110 (US) AL BA HR MK RS (74) Representative: Schaeberle, Steffen (30) Priority: 12.07.2005 US 69872305 P Hoefer & Partner 24.08.2005 US 71115705 P Patentanwälte 24.08.2005 US 71115805 P Pilgersheimer Strasse 20 81543 München (DE) (62) Document number(s) of the earlier application(s) in accordance with Art. 76 EPC: Remarks: 06787393.5 / 1 919 290 This application was filed on 29-12-2011 as a divisional application to the application mentioned under INID code 62. (54) Use of danazol for the treatment of uveitis (57) The present invention relates to the treatment of an inflammatory disease or condition of the eye such as uveitis with danazof or a pharmacologically-acceptable salt or ester thereof. EP 2 446 888 A2 Printed by Jouve, 75001 PARIS (FR) EP 2 446 888 A2 Description FIELD OF THE INVENTION 5 [0001] The present invention relates to the treatment of diseases and conditions with an effective amount of a steroid having those formulas given below, or a pharmacologically-acceptable salt or ester thereof. -

VETORYL® CAPSULES (Trilostane) Monitoring Form
VETORYL® CAPSULES (trilostane) Monitoring Form Date:___________________________________________________________ Client Name:____________________________________________________ Patient Name:___________________________________________________ Phone Number: _________________________________________________ Your dog is coming in to assess the effectiveness of treatment with VETORYL® CAPSULES (trilostane). Date medication was last given: _____________________________________________________ Time medication was last given: _____________________________________________________ Was the medication given with food: YES NO Has your pet experienced any of the following (Please circle if Yes): Vomiting Diarrhea Lethargy Decreased Appetite Other___________________________________________ Have the clinical signs of Cushing’s Syndrome your dog was experiencing improved? YES NO Signature:______________________________________________________ Available in 5, 10, 30, 60, and 120 mg VETORYL is a trademark of Dechra LTD. ©2015, Dechra Ltd. NADA 141-291, Approved by FDA As with all drugs, side effects may occur. In field studies and post-approval experience, the most common side effects reported were: anorexia, lethargy/ depression, vomiting, diarrhea, elevated liver enzymes, elevated potassium with or without decreased sodium, elevated BUN, decreased Na/K ratio, hypoadrenocorticism, weakness, elevated creatinine, shaking, and renal insufficiency. In some cases, death has been reported as an outcome of these adverse events. VETORYL Capsules are not for -

< MOH Approved Drugs List >
Ministry Of Health Directorate General of Medical Supplies Rep_Id : App_Drugs_List_Who.rdf < MOH Approved Drugs List > DATE : 12/08/2009 Page : 1 of 108 VED Flag <S.No> < Item Code > < I T E M D E S C ROF I P- T I O N > < U N I T > DATE : ABC Flag H/C Flag Category : DRUGS 1 Ph. System : GASTRO-INTESTINAL SYSTEM 1 Main Group : ANTACIDS 1 Sub Group : ALUMINIUM COMPOUNDS 1 03000000105 ALUMINIUM HYDROXIDE GEL, DRIED 475 MG. CAPSULE Desirable Cat_C Not H/C Item 2 Sub Group : ANTACID COMPOUND PREPARATIONS 2 02000000079 ANTACID SUSPENSION (ALUMINIUM HYDROXIDE + BOTTLE Desirable MAGNESIUM HYDROXIDE OR TRISILICATE) 100 - 200 Cat_A ML. B0TTLE. H/C Item 3 03000000173 ANTACID TABLET (ALUMINIUM HYDROXIDE + TABLET/CAP Desirable MAGNESIUM HYDROXIDE OR TRISILICATE). Cat_A H/C Item 2 Main Group : ANTISPASMODICS 1 Sub Group : ANTIMUSCARINICS 4 01000000304 HYOSCINE N BUTYLBROMIDE 20MG/ML. 1ML. AMPOULE Essantial Cat_A H/C Item 5 03000000640 HYOSCINE N BUTYL BROMIDE 10MG. TABLET/CAP Essantial Cat_A H/C Item 6 020D0000063 ANTISPASMODIC DROPS 15ML-25ML. BOTTLE Desirable Cat_C Not H/C Item 2 Sub Group : OTHER ANTISPASMODIC AND MOTILITY STIMULANT 7 03000001245 MEBEVERINE HYDROCHLORIDE 100 MG - 135 MG. TABLET/CAP Essantial Cat_B Not H/C Item Ministry Of Health Directorate General of Medical Supplies Rep_Id : App_Drugs_List_Who.rdf < MOH Approved Drugs List > DATE : 12/08/2009 Page : 2 of 108 VED Flag <S.No> < Item Code > < I T E M D E S C ROF I P- T I O N > < U N I T > DATE : ABC Flag H/C Flag Category : DRUGS 1 Ph. -
Canine Cushing's Case Files: the Ins and Outs of Detection And
Canine Cushing’s Case Files: THE INS AND OUTS OF DETECTION AND TREATMENT 01CS-VET0001-0615 SPON SORED BY DECHRA VETERINARY PRODUCTS Canine Cushing’s Case Files: THE INS AND OUTS OF DETECTION AND TREATMENT CLINICAL ARTICLES PRACTICE-RELATED ARTICLES 6 Case file: DALI 26 Your veterinary team’s role in identifying by Audrey K. Cook, BVM&S, MRCVS, DACVIM, DECVIM dogs with hyperadrenocorticism 8 Case file: PRINCESS 28 Your veterinary team’s role in by Lori Thompson, DVM, DACVD treating and monitoring dogs with hyperadrenocorticism 10 Case file: MITCH by David Bruyette, DVM, DACVIM 30 The economics of managing hyperadrenocorticism in dogs 12 Case file: HOLLY by Fritz Wood, CPA, CFP by Christopher G. Byers, DVM, DACVECC, DACVIM 32 Avoiding practitioner pitfalls 14 Case file: LIBBY with canine Cushing’s cases by Todd M. Archer, DVM, MS, DACVIM by Andy Roark, DVM, MS 16 Case file: BOCA by Cynthia Nichols, DVM DECHRA VETERINARY PRODUCTS 18 Case file: HOWIE SUppLEMENTAL RESOURCES by Christopher G. Byers, DVM, DACVECC, DACVIM 34 Diagnosis, Treatment and Monitoring 20 Case file: CALLIE of Hyperadrenocorticism by Orla Mahony, MVB, DACVIM, DECVIM 37 Technical Brochure for VETORYL® 22 Dogs with recurring pyoderma Capsules (trilostane) by Thomas Lewis, DVM, DACVD 24 5 questions veterinarians ask the Dechra Veterinary Products Technical Services Team hen you know the ins and outs of something, it Dechra Veterinary Products, the manufacturer of VETORYL® Wmeans you know the intricate details, fine points, Capsules (trilostane), understands how challenging the diag- peculiarities, or technicalities of a certain subject. The nosis and management of canine hyperadrenocorticism, or phrase the ins and outs also has a second meaning — the Cushing’s syndrome, can be. -

Network-Based Characterization of Drug-Protein Interaction Signatures
Tabei et al. BMC Systems Biology 2019, 13(Suppl 2):39 https://doi.org/10.1186/s12918-019-0691-1 RESEARCH Open Access Network-based characterization of drug-protein interaction signatures with a space-efficient approach Yasuo Tabei1*, Masaaki Kotera2, Ryusuke Sawada3 and Yoshihiro Yamanishi3,4 From The 17th Asia Pacific Bioinformatics Conference (APBC 2019) Wuhan, China. 14–16 January 2019 Abstract Background: Characterization of drug-protein interaction networks with biological features has recently become challenging in recent pharmaceutical science toward a better understanding of polypharmacology. Results: We present a novel method for systematic analyses of the underlying features characteristic of drug-protein interaction networks, which we call “drug-protein interaction signatures” from the integration of large-scale heterogeneous data of drugs and proteins. We develop a new efficient algorithm for extracting informative drug- protein interaction signatures from the integration of large-scale heterogeneous data of drugs and proteins, which is made possible by space-efficient representations for fingerprints of drug-protein pairs and sparsity-induced classifiers. Conclusions: Our method infers a set of drug-protein interaction signatures consisting of the associations between drug chemical substructures, adverse drug reactions, protein domains, biological pathways, and pathway modules. We argue the these signatures are biologically meaningful and useful for predicting unknown drug-protein interactions and are expected to contribute to rational drug design. Keywords: Drug-protein interaction prediction, Drug discovery, Large-scale prediction Background similar drugs are expected to interact with similar pro- Target proteins of drug molecules are classified into a pri- teins, with which the similarity of drugs and proteins are mary target and off-targets. -

Particularly Hazardous Substances (Phs)
PARTICULARLY HAZARDOUS SUBSTANCES (PHS) This list contains examples of chemicals that may be used at the University of Nebraska Medical Center (UNMC). The list is not all-inclusive. This lists contains examples of Particularly Hazardous Substances (PHS) which are a special subset of OSHA Hazardous Chemicals. PHS include chemicals that are known or suspect carcinogens, reproductive toxins, and/or highly toxic materials. Before working with any PHS, please determine if you have any of these and evaluate if additional protective work practices are needed. You should utilize the PHS Assessment Form to help in this evaluation. Abbreviations Used in List Headings CARC NTP National Toxicology Program listed carcinogen - National Toxicology Program K = known carcinogen S = suspect carcinogen CARC IARC International Association for Research on Cancer listed carcinogen - IARC 1= known human carcinogen 2A = probable human carcinogen 2B = possible human carcinogen CARC OSHA OSHA regulated carcinogen - OSHA-regulated carcinogens X = regulated carcinogen REPRO SHEP Included in Catalog of Teratogenic Agents, T.H. Shepard, 6th Edition, Johns Hopkins Press, 1989 X = listed teratogen REPRO CALIF Listed by the State of California ‘Safe Drinking Water Act, 1986’ http://www.oehha.ca.gov/prop65/prop65_list/Newlist.html F = female reproductive hazard M = male reproductive hazard HTX Highly toxic, included in EPA’s list ‘Acutely Toxic Hazardous Waste’, P-listed waste 40 CFR 261.33, or Included in OSHA’s list of highly hazardous chemicals with a threshold £200