WASHINGTON STATE BOARD of PHARMACY Review Form PHARMACY TECHNICIAN TRAINING PROGRAMS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -

Innovation in Pain Management
INNOVATION IN PAIN MANAGEMENT The transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, London, on 12 December 2002 Edited by L A Reynolds and E M Tansey Volume 21 2004 ©The Trustee of the Wellcome Trust, London, 2004 First published by the Wellcome Trust Centre for the History of Medicine at UCL, 2004 The Wellcome Trust Centre for the History of Medicine at University College London is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 0 85484 097 7 Histmed logo images courtesy Wellcome Library, London. Design and production: Julie Wood at Shift Key Design 020 7241 3704 All volumes are freely available online at: www.history.qmul.ac.uk/research/modbiomed/wellcome_witnesses/ Please cite as: Reynolds L A, Tansey E M. (eds) (2004) Innovation in Pain Management. Wellcome Witnesses to Twentieth Century Medicine, vol. 21. London: Wellcome Trust Centre for the History of Medicine at UCL. CONTENTS Illustrations and credits v Witness Seminars: Meetings and publications;Acknowledgements vii E M Tansey and L A Reynolds Introduction Christina Faull xix Transcript Edited by L A Reynolds and E M Tansey 1 Appendix 1 73 Extract from an annotated Physiological Society interview with Patrick Wall (1925–2001) by Martin Rosenberg and Steve McMahon (5 February 1999) Appendix 2 83 Morphine: Optimal potential for benefit with a minimum risk of adverse events and burden by Jan Stjernswärd (12 April 2004) References 85 Biographical notes 103 Index 115 Key to cover photographs ILLUSTRATIONS AND CREDITS Figure 1 Dr Cicely Saunders and two patients at St Joseph’s on their golden wedding anniversary, 1960. -

Updates in Pediatric Dermatology
Peds Derm Updates ELIZABETH ( LISA) SWANSON , M D ADVANCED DERMATOLOGY COLORADO ROCKY MOUNTAIN HOSPITAL FOR CHILDREN [email protected] Disclosures Speaker Sanofi Regeneron Amgen Almirall Pfizer Advisory Board Janssen Powerpoints are the peacocks of the business world; all show, no meat. — Dwight Schrute, The Office What’s New In Atopic Dermatitis? Impact of Atopic Dermatitis Eczema causes stress, sleeplessness, discomfort and worry for the entire family Treating one patient with eczema is an example of “trickle down” healthcare Patients with eczema have increased risk of: ADHD Anxiety and Depression Suicidal Ideation Parental depression Osteoporosis and osteopenia (due to steroids, decreased exercise, and chronic inflammation) Impact of Atopic Dermatitis Sleep disturbances are a really big deal Parents of kids with atopic dermatitis lose an average of 1-1.5 hours of sleep a night Even when they sleep, kids with atopic dermatitis don’t get good sleep Don’t enter REM as much or as long Growth hormone is secreted in REM (JAAD Feb 2018) Atopic Dermatitis and Food Allergies Growing evidence that food allergies might actually be caused by atopic dermatitis Impaired barrier allows food proteins to abnormally enter the body and stimulate allergy Avoiding foods can be harmful Proper nutrition is important Avoidance now linked to increased risk for allergy and anaphylaxis Refer severe eczema patients to Allergist before 4-6 mos of age to talk about food introduction Pathogenesis of Atopic Dermatitis Skin barrier -

Is Oral Morphine Still the First Choice Opioid for Moderate to Severe
Review Palliative Medicine 25(5) 402–409 ! The Author(s) 2010 Is oral morphine still the first choice Reprints and permissions: sagepub.co.uk/journalsPermissions.nav opioid for moderate to severe cancer DOI: 10.1177/0269216310392102 pain? A systematic review within the pmj.sagepub.com European Palliative Care Research Collaborative guidelines project Augusto Caraceni Palliative Care, Pain Therapy and Rehabilitation Unit, Fondazione IRCCS Istituto Nazionale Tumori, Italy Alessandra Pigni Palliative Care, Pain Therapy and Rehabilitation Unit, Fondazione IRCCS Istituto Nazionale Tumori, Italy Cinzia Brunelli Palliative Care, Pain Therapy and Rehabilitation Unit, Fondazione IRCCS Istituto Nazionale Tumori, Italy Abstract The aim of this systematic review was to evaluate the evidence that oral morphine can be recommended as the first choice opioid in the treatment of moderate to severe cancer pain in updating the European Association for Palliative Care opioid recommendations. A systematic literature review was performed to update the 2007 Cochrane review ‘Oral morphine for cancer pain’. The literature search was conducted on MedLine, EMBASE and Cochrane Central Register of Controlled Trials databases. The search strategy, limited in time (from 1 July 2006 to 31 October 2009), was aimed to be as extensive as possible using both text words and MeSH/EMTREE terms; a hand search of the reference lists of identified papers was also performed. Randomized clinical trials, containing data on efficacy and/or side effects of morphine, were identified. Among the papers retrieved from the cited databases and the Cochrane review, 17 eligible studies, for a total of 2053 patients, and a meta-analysis were selected. These studies do not add significant information to the previous Cochrane review confirming the limitation of efficacy and tolerability data on opioid-naı¨ve and non-selected populations of cancer patients treated with morphine and suggesting that oral morphine, oxycodone and hydromorphone have similar efficacy and toxicity in this patient population. -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -

Pimecrolimus for the Treatment of Adults with Atopic Dermatitis, Seborrheic Dermatitis, Or Psoriasis: a Review of Clinical and Cost- Effectiveness
CADTH RAPID RESPONSE REPORT: SUMMARY WITH CRITICAL APPRAISAL Pimecrolimus for the Treatment of Adults with Atopic Dermatitis, Seborrheic Dermatitis, or Psoriasis: A Review of Clinical and Cost- Effectiveness Service Line: Rapid Response Service Version: 1.0 Publication Date: September 25, 2017 Report Length: 19 Pages Authors: Raywat Deonandan, Melissa Severn Cite As: Pimecrolimus for the treatment of adults with atopic dermatitis, seborrheic dermatitis, or psoriasis: a review of clinical and cost- effectiveness. Ottawa: CADTH; 2017 Sep. (CADTH rapid response report: summary with critical appraisal). Acknowledgments: ISSN: 1922-8147 (online) Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. -
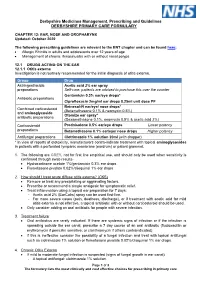
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Acetate, Administration Of, in Parenteral Nutrition Support, 102
327 INDEX Acetate, administration of, in parenteral 50-52 nutrition support, 102 diagnostic tests for, 52-53 Acetominophen, 211, 213 prevention of, 55-58 Acidosis, correction of, with parenteral Aminoglycosides, nephro- and ototoxicity of, nutrition support, 102 11 Actinomycin D, 89 Amekacin, nephrotoxicity of, 11 Acylampicillins, toxic effects of, 10-11 Amphotericin B, chemical structure of, 16 Adenine diphosphate, effect of aspirin on, 212 combined with 5-flucytosine, for crypto- Adolescence, cancer statistics for, 291, 292 coccosis, 30 concept of body image during, 284-85 for aspergillosis, 27 coping strategies for disease during, 289-90 for candidiasis, 23, 24 current approach to cancer care during, for coccidioidomycosis, 31 281-82 for histoplasmosis, 32 emotional and physical development during, for mucormycosis, 28 282-86 for trichosporon infection, 31 general principles for management of cancer interaction of, with granulocyte trans- during, fusions, 73 activities, 298-99 pharmacokinetics of, 17 bereavement follow-up, 305 toxic effects of, 19 birth control, 300 Analgesic(s). See also names of specific drugs diagnosis, 293 classifications of, 206, 207 discussion of diagnosis, 293-98 controversial,231-33 financial expenses, 301-02 equianalgesic comparison of, 222-25 home care, 302-03 guidelines for selection and use of, 208 school program, 299-300 mechanisms of action by, 208-11 sibling care, 300-01 narcotic, supportive care, 298 cardiovascular effects of, 221 psychological impact of illness and hospital chemical classifications of, 216, 218 ization during, 287-89 effects of, on central nervous system, Adriamycin, emesis caused by, 89 219 hematopoietic effects of, 179 effects of, on endocrine system, 221 Aged. -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

Opioid Managementtm a Medical Journal for Proper and Adequate Use
JOURNAL OF OPIOID MANAGEMENT OPIOID OF JOURNAL Journal of Opioid ManagementTM A medical journal for proper and adequate use Volume 3, Number 1 JANUARY/FEBRUARY 2007 ISSN 1551-7489 Official Journal of Opioid Management Society CONTENTS n GUEST EDITORIAL Patterns of illicit drug use and retention in a Can we continue to do business as usual? . 5 methadone program: A longitudinal study. 27 B. Eliot Cole, MD, MPA Ingrid Davstad, MA Marlene Stenbacka, PhD n OPIOID NEWS AND EVENTS Anders Leifman, MSE Calendar . 8 Olof Beck, PhD News briefs . 9 Seher Korkmaz, MD, PhD Anders Romelsjö, MD, PhD n PHARMACY PERSPECTIVE A randomized, open-label, multicenter trial Opioid administration for acute abdominal comparing once-a-day AVINZA® (morphine JANUARY/FEBRUARY 2007 pain in the pediatric emergency department . 11 sulfate extended-release capsules) versus twice- Adi Klein-Kremer, MD a-day OxyContin® (oxycodone hydrochloride Ran D. Goldman, MD controlled-release tablets) for the treatment of chronic, moderate to severe low back pain: n LEGAL PERSPECTIVE Improved physical functioning in the ACTION trial . 35 Medicolegal rounds: Medicolegal issues and alleged breaches of standards of medical care Richard L. Rauck, MD in a patient motor vehicle accident allegedly Stephen A. Bookbinder, MD related to chronic opioid analgesic therapy . 16 Timothy R. Bunker, MD Christopher D. Alftine, MD David A. Fishbain, MD, FAPA Steven Gershon, MD John E. Lewis, PhD Egbert de Jong, MD Brandly Cole, PsyD Andres Negro-Vilar, MD, PhD Renné Steele Rosomoff, BSN, MBA Richard Ghalie, MD Hubert L. Rosomoff, MD, DMedSc, FAAPM n LITERATURE REVIEWS n ORIGINAL ARTICLES Buprenorphine: A unique opioid with broad Morphine prescription in end-of-life care and clinical applications . -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS,