Updates in Pediatric Dermatology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

This Fact Sheet Provides Information to Patients with Eczema and Their Carers. About Topical Corticosteroids How to Apply Topic
This fact sheet provides information to patients with eczema and their carers. About topical corticosteroids You or your child’s doctor has prescribed a topical corticosteroid for the treatment of eczema. For treating eczema, corticosteroids are usually prepared in a cream or ointment and are applied topically (directly onto the skin). Topical corticosteroids work by reducing inflammation and helping to control an over-reactive response of the immune system at the site of eczema. They also tighten blood vessels, making less blood flow to the surface of the skin. Together, these effects help to manage the symptoms of eczema. There is a range of steroids that can be used to treat eczema, each with different strengths (potencies). On the next page, the potencies of some common steroids are shown, as well as the concentration that they are usually used in cream or ointment preparations. Using a moisturiser along with a steroid cream does not reduce the effect of the steroid. There are many misconceptions about the side effects of topical corticosteroids. However these treatments are very safe and patients are encouraged to follow the treatment regimen as advised by their doctor. How to apply topical corticosteroids How often should I apply? How much should I apply? Apply 1–2 times each day to the affected area Enough cream should be used so that the of skin according to your doctor’s instructions. entire affected area is covered. The cream can then be rubbed or massaged into the Once the steroid cream has been applied, inflamed skin. moisturisers can be used straight away if needed. -

Betamethasone Valerate Foam: a Look at the Clinical Data
Review: Clinical Trial Outcomes Betamethasone valerate foam: a look at the clinical data Clin. Invest. (2014) 4(3), 259–267 Topical corticosteroids and especially betamethasone valerate (BMV) have Avner Shemer1, Nicole Sakka1 & been used topically to relieve many inflammatory skin conditions such as Dov Tamarkin*2 psoriasis and atopic dermatitis. The vehicle used to deliver topical drugs 1Department of Dermatology, the Chaim Sheba Medical Center, Affiliated with the can influence the performance of these topical applications. BMV has Tel-Aviv University, Sackler School of Medicine, traditionally been available in creams, ointments, lotions and sprays. In Tel Hashomer, Israel the early 2000s, a topical hydroethanolic BMV foam became commercially 2Foamix Ltd., 2 Holzman Street, Weizmann available. Subsequently, alcohol-free emulsion- and petrolatum-based Science Park, Rehovot 76704, Israel foam formulations were also developed. This manuscript reviews the *Author for correspondence: Tel.: +972 52 457 5677 properties of BMV foams and clinical studies that have been conducted Fax: +972 8 853 1102 to assess their efficacy and safety as treatments for scalp and non-scalp [email protected] psoriasis, as well as other dermatological inflammatory conditions. Keywords: betamethasone valerate • foam • psoriasis • topical corticosteroids Topical corticosteroids have been ranked in four groups consisting of seven classes ranging from ultra-high potency preparations (class 1) to low-potency prepara- tions (class 7). Betamethasone valerate (BMV) is a mid-potency corticosteroid (class 3–5, depending on the dosage form), used topically to relieve inflammatory skin conditions. It is used as a treatment for psoriasis, atopic dermatitis and other corticosteroid-responsive dermatoses. The vehicle used to deliver topical drugs can influence the performance of these drugs. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

4. Antibacterial/Steroid Combination Therapy in Infected Eczema
Acta Derm Venereol 2008; Suppl 216: 28–34 4. Antibacterial/steroid combination therapy in infected eczema Anthony C. CHU Infection with Staphylococcus aureus is common in all present, the use of anti-staphylococcal agents with top- forms of eczema. Production of superantigens by S. aureus ical corticosteroids has been shown to produce greater increases skin inflammation in eczema; antibacterial clinical improvement than topical corticosteroids alone treatment is thus pivotal. Poor patient compliance is a (6, 7). These findings are in keeping with the demon- major cause of treatment failure; combination prepara- stration that S. aureus can be isolated from more than tions that contain an antibacterial and a topical steroid 90% of atopic eczema skin lesions (8); in one study, it and that work quickly can improve compliance and thus was isolated from 100% of lesional skin and 79% of treatment outcome. Fusidic acid has advantages over normal skin in patients with atopic eczema (9). other available topical antibacterial agents – neomycin, We observed similar rates of infection in a prospective gentamicin, clioquinol, chlortetracycline, and the anti- audit at the Hammersmith Hospital, in which all new fungal agent miconazole. The clinical efficacy, antibac- patients referred with atopic eczema were evaluated. In terial activity and cosmetic acceptability of fusidic acid/ a 2-month period, 30 patients were referred (22 children corticosteroid combinations are similar to or better than and 8 adults). The reason given by the primary health those of comparator combinations. Fusidic acid/steroid physician for referral in 29 was failure to respond to combinations work quickly with observable improvement prescribed treatment, and one patient was referred be- within the first week. -

Experience with Molluscum Contagiosum and Associated Inflammatory Reactions in a Pediatric Dermatology Practice the Bump That Rashes
STUDY ONLINE FIRST Experience With Molluscum Contagiosum and Associated Inflammatory Reactions in a Pediatric Dermatology Practice The Bump That Rashes Emily M. Berger, MD; Seth J. Orlow, MD, PhD; Rishi R. Patel, MD; Julie V. Schaffer, MD Objective: To investigate the frequency, epidemiol- (50.6% vs 31.8%; PϽ.001). In patients with molluscum ogy, clinical features, and prognostic significance of in- dermatitis, numbers of MC lesions increased during the flamed molluscum contagiosum (MC) lesions, mollus- next 3 months in 23.4% of those treated with a topical cum dermatitis, reactive papular eruptions resembling corticosteroid and 33.3% of those not treated with a topi- Gianotti-Crosti syndrome, and atopic dermatitis in pa- cal corticosteroid, compared with 16.8% of patients with- tients with MC. out dermatitis. Patients with inflamed MC lesions were less likely to have an increased number of MC lesions Design: Retrospective medical chart review. over the next 3 months than patients without inflamed MC lesions or dermatitis (5.2% vs 18.4%; PϽ.03). The Setting: University-based pediatric dermatology practice. GCLRs were associated with inflamed MC lesion (PϽ.001), favored the elbows and knees, tended to be Patients: A total of 696 patients (mean age, 5.5 years) pruritic, and often heralded resolution of MC. Two pa- with molluscum. tients developed unilateral laterothoracic exanthem– like eruptions. Main Outcome Measures: Frequencies, characteris- tics, and associated features of inflammatory reactions Conclusions: Inflammatory reactions to MC, including to MC in patients with and without atopic dermatitis. the previously underrecognized GCLR, are common. Treat- ment of molluscum dermatitis can reduce spread of MC Results: Molluscum dermatitis, inflamed MC lesions, and via autoinoculation from scratching, whereas inflamed MC Gianotti-Crosti syndrome–like reactions (GCLRs) oc- lesions and GCLRs reflect cell-mediated immune re- curred in 270 (38.8%), 155 (22.3%), and 34 (4.9%) of sponses that may lead to viral clearance. -

Bluecross Blueshield of Western New York Formulary 1 Please Bring This Guide with You the Next Time You Visit Your Doctor
BlueCross BlueShield of Western New York Formulary 1 Please bring this guide with you the next time you visit your doctor. If you have questions about your prescription drug benefit, visit the Pharmacy Services section of the BlueCross BlueShield web site at www.bcbswny.com. CRP2107_009678.1 MG009678A (Revise Date 07/01/2021) A Division of HealthNow New York Inc. An independent licensee of the BlueCross BlueShield Association. The Cross and Shield are registered trademarks of the BlueCross BlueShield Association. Inside front cover TABLE OF CONTENTS INTRODUCTION . iii UNDERSTANDING THE SYMBOLS USED THROUGHOUT THIS BOOK . iii USING THIS FORMULARY BOOK TO HELP CONTAIN COSTS . iv Save Money on Your Prescription Drugs . iv Finding Medications in the Guide . v SECTION 1 — THERAPEUTIC DRUG CATEGORIES . 1 SECTION II — INDEX . 8 ii The BlueCross BlueShield of Western New York Formulary 1 is a list of drugs to help guide physicians and pharmacists to select the medication that provides the appropriate treatment for the best price. INTRODUCTION BlueCross Blue Shield of Western New York has established an independent committee of practicing physicians and a pharmacist to help ensure that our formularies are medically sound and that they support your patients’ health. This committee—called the Pharmacy and Therapeutics Committee—reviews and evaluates medications on the formulary based on safety and efficacy to help maintain clinical integrity in all therapeutic categories. UNDERSTANDING THE SYMBOLS USED THROUGHOUT THIS BOOK Throughout this book, you will see certain symbols that indicate a management program is in place for selected medications. The symbols are as follows: Key P = A step edit applies to this drug. -

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

St John's Institute of Dermatology
St John’s Institute of Dermatology Topical steroids This leaflet explains more about topical steroids and how they are used to treat a variety of skin conditions. If you have any questions or concerns, please speak to a doctor or nurse caring for you. What are topical corticosteroids and how do they work? Topical corticosteroids are steroids that are applied onto the skin and are used to treat a variety of skin conditions. The type of steroid found in these medicines is similar to those produced naturally in the body and they work by reducing inflammation within the skin, making it less red and itchy. What are the different strengths of topical corticosteroids? Topical steroids come in a number of different strengths. It is therefore very important that you follow the advice of your doctor or specialist nurse and apply the correct strength of steroid to a given area of the body. The strengths of the most commonly prescribed topical steroids in the UK are listed in the table below. Table 1 - strengths of commonly prescribed topical steroids Strength Chemical name Common trade names Mild Hydrocortisone 0.5%, 1.0%, 2.5% Hydrocortisone Dioderm®, Efcortelan®, Mildison® Moderate Betamethasone valerate 0.025% Betnovate-RD® Clobetasone butyrate 0.05% Eumovate®, Clobavate® Fluocinolone acetonide 0.001% Synalar 1 in 4 dilution® Fluocortolone 0.25% Ultralanum Plain® Fludroxycortide 0.0125% Haelan® Tape Strong Betamethasone valerate 0.1% Betnovate® Diflucortolone valerate 0.1% Nerisone® Fluocinolone acetonide 0.025% Synalar® Fluticasone propionate 0.05% Cutivate® Hydrocortisone butyrate 0.1% Locoid® Mometasone furoate 0.1% Elocon® Very strong Clobetasol propionate 0.1% Dermovate®, Clarelux® Diflucortolone valerate 0.3% Nerisone Forte® 1 of 5 In adults, stronger steroids are generally used on the body and mild or moderate steroids are used on the face and skin folds (armpits, breast folds, groin and genitals). -

Pimecrolimus for the Treatment of Adults with Atopic Dermatitis, Seborrheic Dermatitis, Or Psoriasis: a Review of Clinical and Cost- Effectiveness
CADTH RAPID RESPONSE REPORT: SUMMARY WITH CRITICAL APPRAISAL Pimecrolimus for the Treatment of Adults with Atopic Dermatitis, Seborrheic Dermatitis, or Psoriasis: A Review of Clinical and Cost- Effectiveness Service Line: Rapid Response Service Version: 1.0 Publication Date: September 25, 2017 Report Length: 19 Pages Authors: Raywat Deonandan, Melissa Severn Cite As: Pimecrolimus for the treatment of adults with atopic dermatitis, seborrheic dermatitis, or psoriasis: a review of clinical and cost- effectiveness. Ottawa: CADTH; 2017 Sep. (CADTH rapid response report: summary with critical appraisal). Acknowledgments: ISSN: 1922-8147 (online) Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. -
EAR, NOSE and OROPHARYNX Updated: October 2020
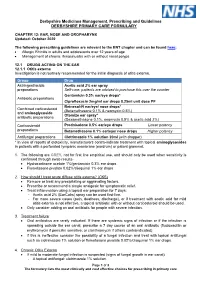
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -
Mupirocin Cream USP, 2%
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: ANDA 201587 Name: Mupirocin Cream USP, 2% Sponsor: Glenmark Generics Inc., USA Approval Date: January 24, 2013 CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: ANDA 201587 CONTENTS Reviews / Information Included in this Review Approval Letter X Other Action Letters Labeling X Labeling Review(s) X Medical Review(s) Chemistry Review(s) X Pharm/Tox Review(s) Statistical Review(s) X Microbiology Review(s) Bioequivalence Review(s) X Other Review(s) X Administrative & Correspondence Documents X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: ANDA 201587 APPROVAL LETTER DEPARTMENT OF HEALTH & HUMAN SERVICES Food and Drug Administration Rockville, MD 20857 ANDA 201587 Glenmark Generics Inc., USA U.S. Agent for: Glenmark Generics Ltd. Attention: William R. McIntyre, Ph.D. Executive Vice President, Regulatory Affairs 750 Corporate Drive Mahwah, NJ 07430 Dear Sir: This is in reference to your abbreviated new drug application (ANDA) dated February 22, 2010, submitted pursuant to section 505(j) of the Federal Food, Drug, and Cosmetic Act (the Act), for Mupirocin Cream USP, 2%. Reference is also made to your amendments dated June 1, 2010; August 16, 2011; and January 19, January 27, April 27, July 18, and July 20, 2012. We also acknowledge receipt of your correspondence dated November 2, 2012, addressing patent issues associated with this ANDA. We have completed the review of this ANDA and have concluded that adequate information has been presented to demonstrate that the drug is safe and effective for use as recommended in the submitted labeling. Accordingly the ANDA is approved, effective on the date of this letter.