Genetics of Movement Disorders in the Next-Generation Sequencing Era
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phosphorylation of Synaptojanin Differentially Regulates Endocytosis of Functionally Distinct Synaptic Vesicle Pools
8882 • The Journal of Neuroscience, August 24, 2016 • 36(34):8882–8894 Cellular/Molecular Phosphorylation of Synaptojanin Differentially Regulates Endocytosis of Functionally Distinct Synaptic Vesicle Pools X Junhua Geng,1* Liping Wang,1,2* Joo Yeun Lee,1,4 XChun-Kan Chen,1 and Karen T. Chang1,3,4 1Zilkha Neurogenetic Institute, 2Department of Biochemistry and Molecular Biology, and 3Department of Cell and Neurobiology, Keck School of Medicine, University of Southern California, Los Angeles, California 90089, and 4Neuroscience Graduate Program, University of Southern California, Los Angeles, California 90089 The rapid replenishment of synaptic vesicles through endocytosis is crucial for sustaining synaptic transmission during intense neuronal activity. Synaptojanin (Synj), a phosphoinositide phosphatase, is known to play an important role in vesicle recycling by promoting the uncoating of clathrin following synaptic vesicle uptake. Synj has been shown to be a substrate of the minibrain (Mnb) kinase, a fly homolog of the dual-specificity tyrosine phosphorylation-regulated kinase 1A (DYRK1A); however, the functional impacts of Synj phosphorylation by Mnb are not well understood. Here we identify that Mnb phosphorylates Synj at S1029 in Drosophila. We find that phosphorylation of Synj at S1029 enhances Synj phosphatase activity, alters interaction between Synj and endophilin, and promotes efficient endocytosis of the active cycling vesicle pool (also referred to as exo-endo cycling pool) at the expense of reserve pool vesicle endocytosis. Dephosphorylated Synj, on the other hand, is deficient in the endocytosis of the active recycling pool vesicles but maintains reserve pool vesicle endocytosis to restore total vesicle pool size and sustain synaptic transmission. Together, our findings reveal a novel role for Synj in modulating reserve pool vesicle endocytosis and further indicate that dynamic phosphorylation and dephosphorylation of Synj differentially maintain endocytosis of distinct functional synaptic vesicle pools. -

Large-Scale Analysis of Genome and Transcriptome Alterations in Multiple Tumors Unveils Novel Cancer-Relevant Splicing Networks
Downloaded from genome.cshlp.org on September 28, 2021 - Published by Cold Spring Harbor Laboratory Press Research Large-scale analysis of genome and transcriptome alterations in multiple tumors unveils novel cancer-relevant splicing networks Endre Sebestyén,1,5 Babita Singh,1,5 Belén Miñana,1,2 Amadís Pagès,1 Francesca Mateo,3 Miguel Angel Pujana,3 Juan Valcárcel,1,2,4 and Eduardo Eyras1,4 1Universitat Pompeu Fabra, E08003 Barcelona, Spain; 2Centre for Genomic Regulation, E08003 Barcelona, Spain; 3Program Against Cancer Therapeutic Resistance (ProCURE), Catalan Institute of Oncology (ICO), Bellvitge Institute for Biomedical Research (IDIBELL), E08908 L’Hospitalet del Llobregat, Spain; 4Catalan Institution for Research and Advanced Studies, E08010 Barcelona, Spain Alternative splicing is regulated by multiple RNA-binding proteins and influences the expression of most eukaryotic genes. However, the role of this process in human disease, and particularly in cancer, is only starting to be unveiled. We system- atically analyzed mutation, copy number, and gene expression patterns of 1348 RNA-binding protein (RBP) genes in 11 solid tumor types, together with alternative splicing changes in these tumors and the enrichment of binding motifs in the alter- natively spliced sequences. Our comprehensive study reveals widespread alterations in the expression of RBP genes, as well as novel mutations and copy number variations in association with multiple alternative splicing changes in cancer drivers and oncogenic pathways. Remarkably, the altered splicing patterns in several tumor types recapitulate those of undifferen- tiated cells. These patterns are predicted to be mainly controlled by MBNL1 and involve multiple cancer drivers, including the mitotic gene NUMA1. We show that NUMA1 alternative splicing induces enhanced cell proliferation and centrosome am- plification in nontumorigenic mammary epithelial cells. -

RBM11 Sirna (H): Sc-91387
SANTA CRUZ BIOTECHNOLOGY, INC. RBM11 siRNA (h): sc-91387 BACKGROUND PRODUCT Proteins containing RNA recognition motifs, including various hnRNP proteins, RBM11 siRNA (h) is a pool of 3 target-specific 19-25 nt siRNAs designed are implicated in the regulation of alternative splicing and protein components to knock down gene expression. Each vial contains 3.3 nmol of lyophilized of snRNPs. The RBM (RNA-binding motif) gene family encodes proteins with siRNA, sufficient for a 10 µM solution once resuspended using protocol an RNA binding motif that have been suggested to play a role in the modu- below. Suitable for 50-100 transfections. Also see RBM11 shRNA Plasmid (h): lation of apoptosis. RBM11 (RNA-binding protein 11) is a 281 amino acid sc-91387-SH and RBM11 shRNA (h) Lentiviral Particles: sc-91387-V as alter- nuclear protein that contains one RNA recognition motif. RBM11 exists as nate gene silencing products. two isoforms produced by alternative splicing and is expressed in testis, kid- For independent verification of RBM11 (h) gene silencing results, we also ney, spleen, brain, spinal cord and mammary gland. The gene that encodes provide the individual siRNA duplex components. Each is available as 3.3 nmol RBM11 maps to chromosome 21, the smallest of the human chromosomes. of lyophilized siRNA. These include: sc-91387A, sc-91387B and sc-91387C. Down syndrome, also known as trisomy 21, is the disease most commonly associated with chromosome 21. Alzheimer’s disease, Jervell and Lange- STORAGE AND RESUSPENSION Nielsen syndrome and amyotrophic lateral sclerosis are also associated with chromosome 21. Store lyophilized siRNA duplex at -20° C with desiccant. -

Ever 2018 Eupo 2018
European Association for Vision and Eye Research European University Professors of Ophthalmology EVER 2018 Annual Congress October 4-6, 2018 EUPO 2018 Course on Retina, Intraocular Inflammation & Uveitis October 3-4, 2018 Programme book Nice, France www.ever.be www.eupo.eu European Association for Vision and Eye Research EVER 20October 17-1919 in Nice, France www.ever.be 1 Table of contents Word from the president ....................................................................................................................................2 About EVER ..........................................................................................................................................................3 EVER Membership ...............................................................................................................................................4 Speakers’ affiliation to scientific sections .........................................................................................................5 Composition of the board 2018 .........................................................................................................................8 Venue ................................................................................................................................................................... 10 Congress information ....................................................................................................................................... 11 Programme information ....................................................................................................................................15 -

Mutations in Pi(3,5)P2 Signaling and Neurodegeneration in Mouse and Human
MUTATIONS IN PI(3,5)P2 SIGNALING AND NEURODEGENERATION IN MOUSE AND HUMAN by Clement Y. Chow A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Human Genetics) in The University of Michigan 2008 Doctoral Committee: Professor Miriam H. Meisler, Chair Professor Sally A. Camper Professor David Ginsburg Associate Professor David C. Kohrman Assistant Professor Geoffrey G. Murphy Clement Y. Chow 2008 To my wife, Candace For all her love and support ii ACKNOWLEDGEMENTS I would first like to thank my mentor, Miriam Meisler. She is the consummate scientist. Miriam is inquisitive and interested in a wide range of topics. This trait has taught me to always ask the right questions and be skeptical of conclusions that are not supported by data. Miriam’s unending desire to make each oral presentation perfect drove me to improve my own skills. I came to this lab without any public presentation skills, but I am now greatly improved in my presentation abilities, a skill crucial for a successful scientific career. Miriam is a perfectionist when it comes to writing and always encouraged me to do the same. I will continue to strive to perfect my writing abilities. I came to the lab wanting to positionally clone a mouse mutant. I told Miriam that I would stay in the lab if she allowed me to do so. She was supportive and excited from the beginning, allowing me to pursue a project with an unknown future. This allowed me to learn, first hand, many aspects of genetics that such a project provides. -

Short-Term Rapamycin Persistently Improves Cardiac Function After Cessation of Treatment in Aged Male and Female Mice
Short-term rapamycin persistently improves cardiac function after cessation of treatment in aged male and female mice. Ellen Quarles A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2017 Reading Committee: Peter Rabinovitch, Chair Michael MacCoss David Marcinek Program Authorized to Offer Degree: Pathology © Copyright 2017 Ellen Quarles University of Washington Abstract Short-term rapamycin persistently improves cardiac function after cessation of treatment in aged male and female mice. Ellen Quarles Chair of the Supervisory Committee: Peter Rabinovitch, Professor and Vice Chair of Research Department of Pathology Cardiac aging is an intrinsic process that results in impaired cardiac function and dysregulation of cellular and molecular quality control mechanisms. These effects are evident in the decline of diastolic function, increase in left ventricular hypertrophy, metabolic substrate shifts, and alterations to the cardiac proteome. This thesis covers the quality control mechanisms that are associated with cardiac aging, results from an anti-aging intervention in aged mice, and a review of mitochondrial dysfunction in the heart. Chapter one is a review of the quality control mechanisms in aging myocardium. Chapter two consists of the results of several mouse experiments that compare the cardiac function, proteomes, and metabolomes of aged and young controls, along with rapamycin treated aged mice. The novelty of this study comes from the inclusion of a group of animals treated only transiently with the drug, then followed for eight weeks post-drug-removal. This persistence cohort may hold clues to deriving long-lasting benefits of rapamycin with only transient treatment. -

REPORT Genome-Wide Linkage Analysis of a Parkinsonian-Pyramidal Syndrome Pedigree by 500 K SNP Arrays
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector REPORT Genome-wide Linkage Analysis of a Parkinsonian-Pyramidal Syndrome Pedigree by 500 K SNP Arrays Seyedmehdi Shojaee,1 Farzad Sina,4 Setareh Sadat Banihosseini,5 Mohammad Hossein Kazemi,5 Reza Kalhor,6 Gholam-Ali Shahidi,4 Hossein Fakhrai-Rad,7 Mostafa Ronaghi,7 and Elahe Elahi2,3,* Robust SNP genotyping technologies and data analysis programs have encouraged researchers in recent years to use SNPs for linkage studies. Platforms used to date have been 10 K chip arrays, but the possible value of interrogating SNPs at higher densities has been con- sidered. Here, we present a genome-wide linkage analysis by means of a 500 K SNP platform. The analysis was done on a large pedigree affected with Parkinsonian-pyramidal syndrome (PPS), and the results showed linkage to chromosome 22. Sequencing of candidate genes revealed a disease-associated homozygous variation (R378G) in FBXO7. FBXO7 codes for a member of the F-box family of proteins, all of which may have a role in the ubiquitin-proteosome protein-degradation pathway. This pathway has been implicated in various neurodegenerative diseases, and identification of FBXO7 as the causative gene of PPS is expected to shed new light on its role. The per- formance of the array was assessed and systematic analysis of effects of SNP density reduction was performed with the real experimental data. Our results suggest that linkage in our pedigree may have been missed had we used chips containing less than 100,000 SNPs across the genome. -
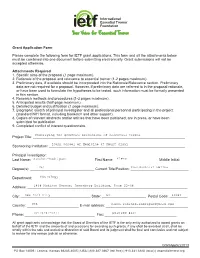
Grant Application Form Please Complete the Following Form for IETF
©2007 IETF Grant Application Form Please complete the following form for IETF grant applications. This form and all the attachments below must be combined into one document before submitting electronically. Grant submissions will not be accepted otherwise. Attachments Required 1. Specific aims of the proposal (1 page maximum). 2. Rationale of the proposal and relevance to essential tremor (1-2 pages maximum). 3. Preliminary data, if available should be incorporated into the Rationale/Relevance section. Preliminary data are not required for a proposal. However, if preliminary data are referred to in the proposal rationale, or have been used to formulate the hypotheses to be tested, such information must be formally presented in this section. 4. Research methods and procedures (1-2 pages maximum). 5. Anticipated results (half-page maximum). 6. Detailed budget and justification (1 page maximum). 7. Biographic sketch of principal investigator and all professional personnel participating in the project (standard NIH format, including biosketch and other support). 8. Copies of relevant abstracts and/or articles that have been published, are in press, or have been submitted for publication. 9. Completed conflict of interest questionnaire. Project Title: ____________________________________________________________________________ Sponsoring Institution: ____________________________________________________________________ Principal Investigator: Last Name: _______________________________ First Name: ______________________ Middle Initial: __ Degree(s): -

Viewed and Published Immediately Upon Acceptance Cited in Pubmed and Archived on Pubmed Central Yours — You Keep the Copyright
BMC Genomics BioMed Central Research article Open Access Differential gene expression in ADAM10 and mutant ADAM10 transgenic mice Claudia Prinzen1, Dietrich Trümbach2, Wolfgang Wurst2, Kristina Endres1, Rolf Postina1 and Falk Fahrenholz*1 Address: 1Johannes Gutenberg-University, Institute of Biochemistry, Mainz, Johann-Joachim-Becherweg 30, 55128 Mainz, Germany and 2Helmholtz Zentrum München – German Research Center for Environmental Health, Institute for Developmental Genetics, Ingolstädter Landstraße 1, 85764 Neuherberg, Germany Email: Claudia Prinzen - [email protected]; Dietrich Trümbach - [email protected]; Wolfgang Wurst - [email protected]; Kristina Endres - [email protected]; Rolf Postina - [email protected]; Falk Fahrenholz* - [email protected] * Corresponding author Published: 5 February 2009 Received: 19 June 2008 Accepted: 5 February 2009 BMC Genomics 2009, 10:66 doi:10.1186/1471-2164-10-66 This article is available from: http://www.biomedcentral.com/1471-2164/10/66 © 2009 Prinzen et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: In a transgenic mouse model of Alzheimer disease (AD), cleavage of the amyloid precursor protein (APP) by the α-secretase ADAM10 prevented amyloid plaque formation, and alleviated cognitive deficits. Furthermore, ADAM10 overexpression increased the cortical synaptogenesis. These results suggest that upregulation of ADAM10 in the brain has beneficial effects on AD pathology. Results: To assess the influence of ADAM10 on the gene expression profile in the brain, we performed a microarray analysis using RNA isolated from brains of five months old mice overexpressing either the α-secretase ADAM10, or a dominant-negative mutant (dn) of this enzyme. -

The Expression of Cold-Inducible RNA-Binding Protein Mrna in Sow Genital Tract Is Modulated by Natural Mating, but Not by Seminal Plasma
International Journal of Molecular Sciences Article The Expression of Cold-Inducible RNA-Binding Protein mRNA in Sow Genital Tract Is Modulated by Natural Mating, but not by Seminal Plasma Jaume Gardela 1,2 , Mateo Ruiz-Conca 1,2 , Cristina A. Martinez 1 , Dominic Wright 3, Manel López-Béjar 2,4, Heriberto Rodriguez-Martinez 1 and Manuel Alvarez-Rodriguez 1,2,* 1 Department of Biomedical and Clinical Sciences (BKV), Division of Children’s and Women Health (BKH), Obstetrics and Gynaecology, Linköping University, 58185 Linköping, Sweden; [email protected] (J.G.); [email protected] (M.R.-C.); [email protected] (C.A.M.); [email protected] (H.R.-M.) 2 Department of Animal Health and Anatomy, Veterinary Faculty, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] or [email protected] 3 Department of Physics, Chemistry and Biology, Faculty of Science and Engineering, Linköping University, 58185 Linköping, Sweden; [email protected] 4 College of Veterinary Medicine, Western University of Health Sciences, Pomona, CA 91766, USA * Correspondence: [email protected]; Tel.: +46-(0)729427883 Received: 10 June 2020; Accepted: 24 July 2020; Published: 27 July 2020 Abstract: The RNA-binding proteins (RBPs), some of them induced by transient receptor potential (TRP) ion channels, are crucial regulators of RNA function that can contribute to reproductive pathogenesis, including inflammation and immune dysfunction. This study aimed to reveal the influence of spermatozoa, seminal plasma, or natural mating on mRNA expression of RBPs and TRP ion channels in different segments of the internal genital tract of oestrous, preovulatory sows. -

Genes Implicated in Familial Parkinson's Disease Provide a Dual
International Journal of Molecular Sciences Review Genes Implicated in Familial Parkinson’s Disease Provide a Dual Picture of Nigral Dopaminergic Neurodegeneration with Mitochondria Taking Center Stage Rafael Franco 1,2,† , Rafael Rivas-Santisteban 1,2,† , Gemma Navarro 2,3,† , Annalisa Pinna 4,*,† and Irene Reyes-Resina 1,†,‡ 1 Department Biochemistry and Molecular Biomedicine, University of Barcelona, 08028 Barcelona, Spain; [email protected] (R.F.); [email protected] (R.R.-S.); [email protected] (I.R.-R.) 2 Centro de Investigación Biomédica en Red Enfermedades Neurodegenerativas (CiberNed), Instituto de Salud Carlos III, 28031 Madrid, Spain; [email protected] 3 Department Biochemistry and Physiology, School of Pharmacy and Food Sciences, University of Barcelona, 08028 Barcelona, Spain 4 National Research Council of Italy (CNR), Neuroscience Institute–Cagliari, Cittadella Universitaria, Blocco A, SP 8, Km 0.700, 09042 Monserrato (CA), Italy * Correspondence: [email protected] † These authors contributed equally to this work. ‡ Current address: RG Neuroplasticity, Leibniz Institute for Neurobiology, Brenneckestr 6, 39118 Magdeburg, Germany. Abstract: The mechanism of nigral dopaminergic neuronal degeneration in Parkinson’s disease (PD) Citation: Franco, R.; Rivas- is unknown. One of the pathological characteristics of the disease is the deposition of α-synuclein Santisteban, R.; Navarro, G.; Pinna, (α-syn) that occurs in the brain from both familial and sporadic PD patients. This paper constitutes a A.; Reyes-Resina, I. Genes Implicated narrative review that takes advantage of information related to genes (SNCA, LRRK2, GBA, UCHL1, in Familial Parkinson’s Disease VPS35, PRKN, PINK1, ATP13A2, PLA2G6, DNAJC6, SYNJ1, DJ-1/PARK7 and FBXO7) involved in Provide a Dual Picture of Nigral familial cases of Parkinson’s disease (PD) to explore their usefulness in deciphering the origin of Dopaminergic Neurodegeneration dopaminergic denervation in many types of PD. -

Computational Analyses of Small Molecules Activity from Phenotypic Screens
Computational analyses of small molecules activity from phenotypic screens Azedine Zoufir Hughes Hall This dissertation is submitted for the degree of Doctor of Philosophy July 2018 Declaration This thesis is submitted as the result of my own work and includes nothing which is the outcome of work done in collaboration except where specifically indicated in the text. It is not substantially the same as any that I have submitted, or, is being concurrently submitted for a degree or diploma or other qualification at the University of Cambridge or any other University or similar institution except as declared in the preface and specified in the text. I further state that no substantial part of my dissertation has already been submitted, or, is being concurrently submitted for any such degree, diploma or other qualification at the University of Cambridge or any other University or similar institution except as declared in the Preface and specified in the text. This dissertation does not exceed the word limit of 60,000 words. Azedine Zoufir July 2018 Summary Title: Computational analyses of small molecules activity from phenotypic screens Author: Azedine Zoufir Drug discovery is no longer relying on the one gene-one disease paradigm nor on target-based screening alone to discover new drugs. Phenotypic-based screening is regaining momentum to discover new compounds since those assays provide an environment closer to the physiological state of the disease and allow to better anticipate off-target effects and other factors that can limit the efficacy of the drugs. However, uncovering the mechanism of action of the compounds active in those assays relies on in vitro techniques that are expensive and time- consuming.