Timing of Surgery Following SARS‐Cov‐2 Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
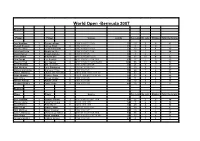
Stats Bermuda World Open 2007
World Open -Bermuda 2007 Round 1 Player Player Scores points Yes Lets No Lets Strokes Total Decisions Amr Shabana 3 Renan Lavigne 1 11/9 11/8 7/11 11/9 77 19 3 5 27 Stewart Boswell 3 James Stout 0 11/5 11/3 11/4 45 1 0 0 1 Thierry Lincou 3 Julian Illingworth 1 11/5 11/3 5/11 11/0 57 13 3 4 20 Jonathan Kemp 3 Ong beng Hee 1 11/8 11/7 8/11 11/4 71 16 1 7 24 David Palmer 3 Shawn Delierre 0 11/4 11/4 11/5 46 3 2 2 7 Peter Barker 3 Bradley Ball 1 8/11 11/8 13/11 11/5 78 37 11 4 52 Alex Gough 3 Lee Beachill 2 4/11 11/8 5/11 11/4 11/5 81 17 1 5 23 Wael El Hindi 3 Eric Galvez 2 9/11 11/6 8/11 12/10 12/10 100 55 11 10 76 Omar Mosaad 3 Olli Tuominen 1 1/11 11/4 11/9 11/4 29 21 3 7 31 Nick Matthew 3 Joey Barrington 1 11/1 8/11 11/6 11/2 61 30 5 2 37 Mohammad Abbas 3 Cameron Pilley 0 11/8 11/6 11/8 55 24 7 6 37 James Willstrop 3 Lauren Jan Anjema 2 10/12 8/11 11/8 11/9 11/3 94 37 7 4 48 Azlan Iskander 3 Shahier Razik 2 11/13 11/6 9/11 11/3 11/6 92 33 8 7 48 John White 3 Alistair Walker 0 11/8 11/4 11/5 50 11 0 4 15 Hisham Ashour 3 Adrian Grant 0 11/7 11/7 11/8 55 10 4 2 16 Gregory Gaultier 3 Darryl Selby 0 11/4 11/7 11/0 44 16 5 1 22 Round 2 Player Player Scores Yes Lets No Lets Strokes Total Decisions Amr Shabana 3 Stewart Boswell 2 8/11 11/4 11/2 9/11 11/4 82 26 0 8 34 Thierry Lincou 3 Jonathan Kemp 0 12/10 11/5 11/5 54 7 6 3 16 David Palmer 3 Peter Barker 0 12/10 11/7 11/9 60 28 4 2 34 Alex Gough 3 Wael El Hindi 1 11/1 7/11 11/4 11/7 63 38 5 8 51 Nick Matthew 3 Omar Mosaad 0 11/6 11/9 11/7 55 19 1 2 22 James Willstrop 3 Mohammad Abbas 2 5/11 9/11 -

Download the World Squash Update In
WORLD SQUASH UPDATE Issue 83 November / December 2019 FOR ALL WSF REGIONAL & NATIONAL FEDERATIONS cc: WSF Regional Presidents, WSF Commission Members, Stakeholders, PSA members, SPINs, Media, Accredited Products and Companies CAPE TOWN HOSTS SUCCESSFUL AGM The World Squash Federation Annual General Meeting took place on 6 November in Cape Town, South Africa, hosted by Squash South Africa. The WSF Conference, which preceded the AGM, facilitated informal discussions and featured presentations to update the delegates on key initiatives - including the World Squash Officiating, a joint enterprise between the WSF and Professional Squash Association (PSA) to develop an online platform that will provide National Federations with the tools to develop refereeing in their country. The new initiative is scheduled to go live before the end of the year. Additionally James Sandwith, from BEBRAND, presented the findings of a strategic review commissioned by WSF, with the report now available for all member nations to appraise. The 49th Annual General Meeting, attended by representatives of 24 National Federations, saw delegates agree an amendment to the Articles of Association to reduce the risk of inappropriate leadership behavior and to ensure that delegates in attendance at an AGM have a formal connection with their National Federations. There were no changes to the standard Rules of Squash. However, the Rules of Squash 57 were updated, adding an extra ball rebound resilience at 33 degrees C that will help to ensure that the differential between blue and black balls - and their range of bounce - will be more uniform across the brands that are WSF-approved. The WSF Championship Regulations were updated with respect to player eligibility, the use of random draws and a new timeline and procedure for seeding juniors. -

Measles in Sudan
Measles in Sudan Diagnosis, Epidemiology and Humoral Immune Response Mazelen in Soedan Diagnostiek, epidemiologie en humorale imuunrespons Thesis to obtain the degree of Doctor from the Erasmus University Rotterdam by command of the Rector Magnificus Prof.dr. S.W.J. Lamberts and according to the decision of the Doctorate Board The public defence shall be held on Wednesday 28 January 2004 at 15.45 hrs by Haja Sittana El Mubarak born at Maryland, USA Doctoral Committee Promotor: Prof.dr. A.D.M.E. Osterhaus Other members: Prof.dr. R. de Groot Prof.dr. E.H.J.H.M. Claassen Prof.dr. C.P. Muller Copromotor: Dr. R.L. de Swart The studies described in this thesis were performed at the department of Virology of the Erasmus MC in Rotterdam, the Netherlands, in close collaboration with the Institute of Endemic Diseases of the University of Khartoum, Sudan. The studies received financial support from INCO-DC grant IC18CT96-0116 from the European Commission. Printing of this thesis was financially supported by: ViroClinics BV, Rotterdam, ViroNovative BV, Rotterdam, Meddens Diagnostics BV, Vorden, DakoCytomation BV, Glostrup. Production: Optima Grafische Communicatie, Rotterdam, The Netherlands To Mohammed and Nimah, my dear parents, lovely family and to Sudan Contents Chapter 1 General Introduction 10 Chapter 2 Diagnosis and molecular epidemiology 23 2.1 Serological and virological characterisation of 25 clinically diagnosed measles cases in suburban Khartoum. J Clin Microbiol 2000;38: 987-991 2.2 Prevention of measles in Sudan: a prospective study 35 on vaccination, diagnosis and epidemiology. Vaccine 2001; 19: 2254-2257 2.3 Genetic characterisation of wild-type measles viruses 41 circulating in suburban Khartoum, 1997-2000. -

By Submitted in Partial Fulfillment of the Requirements for the Degree Of
FROM DIWAN TO PALACE: JORDANIAN TRIBAL POLITICS AND ELECTIONS by LAURA C. WEIR Submitted in partial fulfillment of the requirements For the degree of Doctor of Philosophy Dissertation Adviser: Dr. Pete Moore Department of Political Science CASE WESTERN RESERVE UNIVERSITY January, 2013 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Laura Weir candidate for the Doctor of Philosophy degree *. Pete Moore, Ph.D (chair of the committee) Vincent E. McHale, Ph.D. Kelly McMann, Ph.D. Neda Zawahri, Ph.D. (date) October 19, 2012 *We also certify that written approval has been obtained for any proprietary material contained therein. ii TABLE OF CONTENTS List of Tables v List of Maps and Illustrations viii List of Abbreviations x CHAPTERS 1. RESEARCH PUZZLE AND QUESTIONS Introduction 1 Literature Review 6 Tribal Politics and Elections 11 Case Study 21 Potential Challenges of the Study 30 Conclusion 35 2. THE HISTORY OF THE JORDANIAN ―STATE IN SOCIETY‖ Introduction 38 The First Wave: Early Development, pre-1921 40 The Second Wave: The Arab Revolt and the British, 1921-1946 46 The Third Wave: Ideological and Regional Threats, 1946-1967 56 The Fourth Wave: The 1967 War and Black September, 1967-1970 61 Conclusion 66 3. SCARCE RESOURCES: THE STATE, TRIBAL POLITICS, AND OPPOSITION GROUPS Introduction 68 How Tribal Politics Work 71 State Institutions 81 iii Good Governance Challenges 92 Guests in Our Country: The Palestinian Jordanians 101 4. THREATS AND OPPORTUNITIES: FAILURE OF POLITICAL PARTIES AND THE RISE OF TRIBAL POLITICS Introduction 118 Political Threats and Opportunities, 1921-1970 125 The Political Significance of Black September 139 Tribes and Parties, 1989-2007 141 The Muslim Brotherhood 146 Conclusion 152 5. -
DIPBOOK2021.Pdf
MINISTRY OF FOREIGN AFFAIRS BRUNEI DARUSSALAM DIPLOMATIC AND CONSULAR LIST 2021 Brunei Darussalam Diplomatic and Consular List 2021 is published by MINISTRY OF FOREIGN AFFAIRS Jalan Subok Bandar Seri Begawan BD2710 Brunei Darussalam Telephone : (673) 2261177 / 1291 / 1292 / 1293 / 1294 / 1295 Fax : (673) 2261740 (Protocol & Consular Affairs Department) Email : [email protected] Website : www.mfa.gov.bn All information is correct as of 18 August 2021 Any amendments can be reported to the Protocol and Consular Affairs Department, Ministry of Foreign Affairs, Brunei Darussalam. Email: [email protected] Use QR Code to download an electronic version for this book Printed by Print Plus Sdn Bhd Brunei Darussalam TABLE OF CONTENTS Contents TABLE OF CONTENTS ................................................................................................... 4 DIPLOMATIC MISSIONS ................................................................................................ 1 AFGHANISTAN ............................................................................................................... 2 ALGERIA ....................................................................................................................... 3 ANGOLA ........................................................................................................................ 4 ARGENTINA .................................................................................................................. 5 AUSTRALIA .................................................................................................................. -
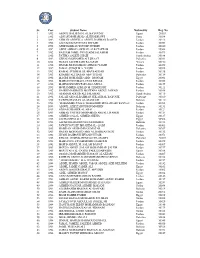
Sr. Year Student Name Nationality Reg. No. 1 1992 ABDUL HALEEM M
Sr. Year Student Name Nationality Reg. No. 1 1992 ABDUL HALEEM M. AL BAYOUMY Egypt 20053 2 1992 ADNAN MOHAMAD AL KHADRAWI Syria 30038 3 1992 AHMAD ABDULLA ABDUL RAHMAN DAOUD Jordan 30213 4 1992 ALI SALEM MUSTAFA DWAIRI Jordan 40051 5 1992 ATEF HABBAS YOUSEF HUSEIN Jordan 40040 6 1992 AWNI AHMAD AWWAD ALFATAFTAH Jordan 20064 7 1992 BASSAM JAMIL SWAILAIM SALAMEH Jordan 40073 8 1992 FATIMA SALEH GHAZI Saudi Arabia 30188 9 1992 GEHAD MOHAMED ALI SHAAT Palestine 30031 10 1992 HASAN SALEH SAID BAJAFAR Yemen 30150 11 1992 ISMAIL MOHAMMAD AHMAD YAGHI Jordan 40059 12 1992 JAMAL SUDQI M.A. YASIN Jordan 30028 13 1992 KAMAL SUBHI M. EL-HAJ BADDAR Jordan 30136 14 1992 KHAMIS ALI HASAN ABU TUHAH Palestine 30134 15 1992 MAGDI MOHAMED ABD - MONAM Egypt 20061 16 1992 MAHMOUD ISMAEL OUDI KHALIL Jordan 40028 17 1992 MAHMOUD MUSTAFA ESA MUSA Jordan 30157 18 1992 MOHAMMED AHMAD M. HAMSHARI Jordan 30111 19 1992 NAJEH MAHMOUD MOSTAFA ABDUL JAWAD Jordan 30058 20 1992 OSAMAH ADEEB ALI SALAMAH Saudi Arabia 30119 21 1992 SALAH ABD ALRAHMAN SHLASH AL BAYOUK Palestine 30010 22 1992 TAWFIQ HASSAN AL-MASKATI Bahrain 30110 23 1993 "MOHAMMED JUMA'A" MOHAMMED HUSSAIN ABU RAYYAN Jordan 40058 24 1993 ABDUL-AZIZ ZAINUDDIN MOHSIN Bahrain 30131 25 1993 ADNAN SHAHER AL'ARAJ Jordan 40121 26 1993 AHMAD YOUSEF MOHAMMD ABDALL HABEH Jordan 40124 27 1993 AHMED GALAL AHMED SHEHA Egypt 20137 28 1993 ALI HASHEM ALI Egypt 30306 29 1993 ALI MOHAMED HUSSN MOHAMED Bahrain 30183 30 1993 FAWZI YOUSEF IBRAHIM AL- QAISI Jordan 40003 31 1993 HAMDAN ALI HAMDAN MATAR Palestine 30267 32 1993 HASAN MOHAMED ABD AL RAHMAN BZEI Jordan 40132 33 1993 HUSNI BAHPOUH HUSAIN UTAIR Jordan 30071 34 1993 KHALIL GUMMA HEMDAN EL-MASRY Palestine 30007 35 1993 MAHMOUD ATYEH MOHD DAHBOUR Jordan 30079 36 1993 MOH'D ABDUL M. -

Men's Athlete Profiles 1 49KG – SIMPLICE FOTSALA – CAMEROON
Gold Coast 2018 Commonwealth Games - Men's Athlete Profiles 49KG – SIMPLICE FOTSALA – CAMEROON (CMR) Date Of Birth : 09/05/1989 Place Of Birth : Yaoundé Height : 160cm Residence : Region du Centre 2018 – Indian Open Boxing Tournament (New Delhi, IND) 5th place – 49KG Lost to Amit Panghal (IND) 5:0 in the quarter-final; Won against Muhammad Fuad Bin Mohamed Redzuan (MAS) 5:0 in the first preliminary round 2017 – AFBC African Confederation Boxing Championships (Brazzaville, CGO) 2nd place – 49KG Lost to Matias Hamunyela (NAM) 5:0 in the final; Won against Mohamed Yassine Touareg (ALG) 5:0 in the semi- final; Won against Said Bounkoult (MAR) 3:1 in the quarter-final 2016 – Rio 2016 Olympic Games (Rio de Janeiro, BRA) participant – 49KG Lost to Galal Yafai (ENG) 3:0 in the first preliminary round 2016 – Nikolay Manger Memorial Tournament (Kherson, UKR) 2nd place – 49KG Lost to Ievgen Ovsiannikov (UKR) 2:1 in the final 2016 – AIBA African Olympic Qualification Event (Yaoundé, CMR) 1st place – 49KG Won against Matias Hamunyela (NAM) WO in the final; Won against Peter Mungai Warui (KEN) 2:1 in the semi-final; Won against Zoheir Toudjine (ALG) 3:0 in the quarter-final; Won against David De Pina (CPV) 3:0 in the first preliminary round 2015 – African Zone 3 Championships (Libreville, GAB) 2nd place – 49KG Lost to Marcus Edou Ngoua (GAB) 3:0 in the final 2014 – Dixiades Games (Yaounde, CMR) 3rd place – 49KG Lost to Marcus Edou Ngoua (GAB) 3:0 in the semi- final 2014 – Cameroon Regional Tournament 1st place – 49KG Won against Tchouta Bianda (CMR) -
2017 Initiates Alphabetical List
AMERICAN COLLEGE OF SURGEONS 2017 INITIATES ALPHABETICAL LIST 30 Hanser Antonio Abreu Quezada Khaled Sami Ahmad Ali Alaraj A Santiago, Dominican Republic Riyadh, Saudi Arabia Chicago, IL Amaar Awad Hussien Hussien Carlos Maria Abril Vega Siddique Ahmad Yakout Hameed Alaraji Aamery Abu Dhabi, United Arab Emirates Peshawar, Pakistan Dubai, United Arab Emirates Wolverhampton, United Kingdom Walid Abu Tahoun Usman Ahmad Nasrin Alavi Wesley M. Abadie Dhahran, Saudi Arabia Cleveland, OH Tehran, Iran, Islamic Republic of Williamsburg, VA Abdelrahman Hassan Abusabeib Azam S. Ahmed Marco Alfonso Albán Garcia Andrea M. Abbott Doha, Qatar Madison, WI Santiago, Chile Mount Pleasant, SC Jihad Achkar Tanveer Ahmed Hamdullah Hadi Al-Baseesee Abdel Rahman Abdel Fattah M. Beirut, Lebanon Dhaka, Bangladesh Najaf, Iraq Abdel Aal Doha, Qatar Alison Alden Acott Manish Ahuja Michael A. Albin Little Rock, AR Mumbai, India South Pasadena, CA Karim Sabry Abdel Samee Cairo, Egypt Badih Adada Naveen Kumar Ahuja Saleh Mohammad Aldaqal Weston, FL Hamilton, NJ Jeddah, Saudi Arabia Eltayib Yousif Abdelaleem Doha, Qatar Patrick Temi Adegun Begum Akay Saad A. A. A. Aldousari Ado-Ekiti, Nigeria Birmingham, MI Kuwait City, Kuwait Tamer Mohamed Said Abdelbaki Salama James Olaniyi Adeniran Hakkı Tankut Akay Matthew J. Alef Cairo, Egypt Ilorin, Kwara State, Nigeria Ankara, Turkey Winooski, VT Kareem R. AbdelFattah Adedoyin Adekunle Adesanya Raed Hatmal Akayleh Farzad Alemi Dallas, TX Lagos, Nigeria Amman, Jordan Kansas City, MO Khaled Mohamed Saad Obinna Ogochukwu Adibe Ahmet Akman Naif Abdullah Alenazi Mostafa Abdelgalel Chapel Hill, NC Ankara, Turkey Riyadh, Saudi Arabia Ajman, United Arab Emirates Farrell C. Adkins Mohamed Gomah Hamed Falih Mohssen Algazgooz Ahmed Mohamed Abdelkader Roanoke, VA Al Aqqad Basra, Iraq Dubai, United Arab Emirates Dubai, United Arab Emirates John Affuso Mohammed S. -

P19.E$S 3 Layout 1
SUNDAY, NOVEMBER 16, 2014 SPORTS ‘Don’t think, just play’: MIT engineers football success NEW YORK: The Massachusetts Institute common.” The architect of the school’s because it gives him a chance to “not place in pop culture decades ago when “Four years ago, we didn’t get a lot of of Technology’s reputation of academic new-found gridiron greatness is 42-year- think.” He said it’s natural for MIT players late comedian George Carlin read the people out to the games,” said senior superiority is well chronicled. But the pri- old Chad Martinovich, a soft-spoken to be analytical because their days in scoreline “MIT, 3 to the 4th power.” running back Justin Wallace, who has vate research university is now excelling coach who has the team riding a never- class revolve around problem-solving. No one is suggesting MIT is ready to scored 16 touchdowns this season while in a sector of society once deemed before-seen three-year winning streak. Still, the books versus ball balancing take on undefeated and top-ranked averaging an eyebrow-raising 7.4 yards unthinkable for a bastion of brainpower: He endures the kinds of problems act is a delicate one, he said. “I’m much Mississippi State, as the list of its victims per carry. “We do now.” With 81 Nobel football. you might expect coaching a bunch of more productive during the season,” this year includes Becker College, Salve laureates having ties to MIT, the percep- MIT is undefeated going into its last rocket scientists. “It’s both rewarding and Goldsberry said. -

Player Games Goals Kamel Massoud 9 0 Labib Mahmoud 8 4
Ahly Players' Stats in Zamalek Cup Derby Last updated 30-03-2019 [egyptianfootball.net 2019] Player Games Goals Kamel Massoud 9 0 Labib Mahmoud 8 4 Mahmoud Mokhtar El-Tetch 8 1 Amin Sabry 7 0 Moustafa Elwani "El-Kassar" 7 0 Saleh El-Sawwaf 7 1 Hussein Hamdi 6 1 Ahmed Mekawi 5 2 Amin Shoair 5 2 Aziz Fahmi - GK 5 -10 Hossam Ashour 5 0 Mourad Fahmi 5 1 Moustafa Latif 5 0 Wagih Moustafa 5 0 Abdel Karim Sakr 4 5 Abdou Saleh El-Wash 4 0 Ahmed Rifaat I 4 0 Ahmed Shobair - GK 4 -4 Emad Moteab 4 3 Hassan Zohni - GK 4 -4 Helmi Aboul Maaty 4 1 Hussein Madkour 4 1 Kamal Hamed - GK 4 -9 Mahmoud Hamdi “Karawan” 4 0 Adel Heikal - GK 3 -4 Ahmed El-Sayed 3 0 Ahmed Fathi 3 0 Alaa Abdel Sadek 3 0 Alaa Mayhoub 3 0 El-Sayed Ateya "Toto" 3 1 El-Sayed El-Dhizui 3 0 Foad Sedki 3 0 Hady Khashaba 3 0 Hani Kamel 3 0 Hussein Hassanain "El-Far" 3 0 Mahmoud Saleh 3 0 Mimi El-Sherbini 3 2 Mohamed Aboutraika 3 2 Mohamed Barakat 3 0 Mohamed Saad 3 0 Monem Salem 3 0 Mounir Hafez 3 0 Reda Abdel Hamid 3 0 Rifaat El-Fanageely 3 0 Saleh Selim 3 2 Sayed Osman 3 0 Tarek Selim 3 0 Abdel Aziz Hammami 2 0 Abdel Galil Hemaida - GK 2 -3 Abdel Hamid Hamdi - GK 2 0 Abdel Maguid El-Ashry 2 0 Abdel Wahab Selim 2 1 Abdullah El-Said 2 1 Ahmed Hassan Kamel 2 0 Ahmed Soliman “HENDENBERG” 2 0 Amr Anwar 2 0 Amr Gamal 2 0 Badr Ragab 2 0 Ahly Players' Stats in Zamalek Cup Derby Last updated 30-03-2019 [egyptianfootball.net 2019] Player Games Goals Dheyaa El-Sayed 2 0 Emad El-Nahhas 2 1 Fathi Khattab 2 1 Gamil El-Zobair 2 1 Hossam Hassan 2 0 Mahmoud El-Mehailmi 2 0 Moamen Zakaria 2 0 Mohamed -
9Roxph 1Xpehu $Xwxpq
7KHVLV ,QWHUQDWLRQDO5HVHDUFK-RXUQDO 9ROXPH1XPEHU-XQH 9ROXPH $UWLFOHV 1XPEHU $XWXPQ 4XLWWLQJZLWK6W\OH/LQJXLVWLF$QDO\VLVRI3ROLWLFDO5HVLJQDWLRQ6SHHFKHV 6LOYDQD1HVKNRYVND S,661 R,661 ,QFOXVLRQRI&KLOGUHQZLWK(PRWLRQDO'LVRUGHUVLQ/HVVRQ3ODQQLQJE\(GXFDWRUV 9LROHWD%X]D$PLQD0XUDWL 7KH5HSXEOLFRI2EMHFWV3UROHJRPHQDWRDQ2EMHFW2ULHQWHG5HDGLQJRID7RXURQWKH 3UDLULHV 1DUXKLNR0LNDGR 7KH,PSDFWRI3URIHVVLRQDO3UDFWLFH6WDQGDUGVLQWKH3URIHVVLRQDO'HYHORSPHQWDQG 3HUIRUPDQFH$VVHVVPHQWRI6FKRRO'LUHFWRUV 8MNDQH+DQD%HVKLUL$UEsURUH%LFDM 8QGHUVWDQGLQJ9LUWXDOLW\$0L[HG0HWKRG6WXG\8VLQJ9LUWXDOLW\,QGH[LQ7HDPVRI *OREDO2XWVRXUFLQJ6HFWRU 8/73*XQDVHNDUH$MDQWKD'KDUPDVLUL 7HDFKHUV 3HUFHSWLRQVRIWKH&XUULFXODU5HIRUP,PSOHPHQWDWLRQLQ.RVRYR )DWMRQD$OLGHPDM 4XDOLW\RI3K\VLRWKHUDSHXWLF6HUYLFHVLQ.RVRYR$&RPSDUDWLYH$SSURDFKEHWZHHQ 3XEOLFDQG3ULYDWH6HFWRUV $ULRQD'HGXVKDM &RQWUDVWLYH$QDO\VLVRI3UHQRPLQDO0RGLILHUVLQ(QJOLVKDQG$OEDQLDQ1RXQ3KUDVHV ,PULMH$]HPL (PSOR\PHQW3ROLFLHVIRU3HRSOHZLWK'LVDELOLWLHVLQ.RVRYR <OEHU$OLX3HWULW%XVKL )XWXUH2SSRUWXQLWLHVIRU6SDWLDO'HYHORSPHQWRIWKH8QLYHUVLW\LQ/LQHZLWK &RQWHPSRUDU\&LW\&RQFHSWV $GHOLQD7DKLUL%XMDU'HPMDKD/XFLMD$çPDQ0RPLUVNL 7KH7HQVLRQVEHWZHHQ6FLHQWLILF7KHRULHVDQG5HDOLW\DVD.QRZOHGJH0HFKDQLVP +DMGLQ$ED]L 7KH)HDWXUHVRIWKH0DFHGRQLDQ6WDQGDUG/DQJXDJHLQWKH-RXUQDOLVWLF6XE6W\OH &ROXPQV 9LROHWD-DQXVKHYD 7KH/LQJXLVWLF'HSHQGHQFHRIDQ,QGHSHQGHQW&RXQWU\ %RUD6.DVDSROOL 1R 7KHVLV±,QWHUQDWLRQDO5HVHDUFK-RXUQDOZZZWKHVLVMRXUQDOQHW .ROHJML$$% =RQD,QGXVWULDOH3ULVKWLQs)XVKs.RVRYs 3ULVKWLQD5HSXEOLFRI.RVRYR 7HO H[W HPDLOWKHVLV#DDEHGXQHW Thesis International Research Journal PUBLISHER MST -

Diplomatic List – Fall 2018
United States Department of State Diplomatic List Fall 2018 Preface This publication contains the names of the members of the diplomatic staffs of all bilateral missions and delegations (herein after “missions”) and their spouses. Members of the diplomatic staff are the members of the staff of the mission having diplomatic rank. These persons, with the exception of those identified by asterisks, enjoy full immunity under provisions of the Vienna Convention on Diplomatic Relations. Pertinent provisions of the Convention include the following: Article 29 The person of a diplomatic agent shall be inviolable. He shall not be liable to any form of arrest or detention. The receiving State shall treat him with due respect and shall take all appropriate steps to prevent any attack on his person, freedom, or dignity. Article 31 A diplomatic agent shall enjoy immunity from the criminal jurisdiction of the receiving State. He shall also enjoy immunity from its civil and administrative jurisdiction, except in the case of: (a) a real action relating to private immovable property situated in the territory of the receiving State, unless he holds it on behalf of the sending State for the purposes of the mission; (b) an action relating to succession in which the diplomatic agent is involved as an executor, administrator, heir or legatee as a private person and not on behalf of the sending State; (c) an action relating to any professional or commercial activity exercised by the diplomatic agent in the receiving State outside of his official functions. -- A diplomatic agent’s family members are entitled to the same immunities unless they are United States Nationals.