Cilostazol Tablets, USP50 Mg and 100 Mgrx Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

Cilostazol Protects Rats Against Alcohol‑Induced Hepatic Fibrosis Via Suppression of TGF‑Β1/CTGF Activation and the Camp/Epac1 Pathway
EXPERIMENTAL AND THERAPEUTIC MEDICINE 17: 2381-2388, 2019 Cilostazol protects rats against alcohol‑induced hepatic fibrosis via suppression of TGF‑β1/CTGF activation and the cAMP/Epac1 pathway KUN HAN, YANTING ZHANG and ZHENWEI YANG Department of Gastroenterology, Xi'an Central Hospital, Xi'an, Shaanxi 710003, P.R. China Received July 2, 2018; Accepted November 23, 2018 DOI: 10.3892/etm.2019.7207 Abstract. Alcohol abuse and chronic alcohol consump- Introduction tion are major causes of alcoholic liver disease worldwide, particularly alcohol‑induced hepatic fibrosis (AHF). Liver Liver fibrosis is a wound‑healing response to a variety of liver fibrosis is an important public health concern because of its insults, including excessive alcohol intake. Alcohol abuse and high morbidity and mortality. The present study examined chronic alcohol consumption are major causes of alcoholic the mechanisms and effects of the phosphodiesterase III liver disease (ALD) worldwide (1). Alcohol‑induced hepatic inhibitor cilostazol on AHF. Rats received alcohol infu- fibrosis (AHF) may cause serious hepatic cirrhosis, and is sions via gavage to induce liver fibrosis and were treated widely accepted as a milestone event in ALD (2). However, with colchicine (positive control) or cilostazol. The serum recent evidence indicates that liver fibrosis is reversible and alcohol dehydrogenase (ADH) and acetaldehyde dehydro- that the liver may recover from cirrhosis (3). Therefore, eluci- genase (ALDH) activities and the albumin/globulin (A/G), dation of the cellular and molecular mechanisms is urgently enzymes and hyaluronic acid (HA), type III precollagen required to prevent AHF. (PC III), laminin (LA), and type IV collagen (IV‑C) levels The exact mechanism remains unclear, but certain changes were measured using commercially available kits. -
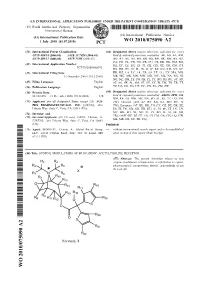
Wo 2010/075090 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Pharmacokinetic Characteristics of Cilostazol 200 Mg Controlled
2016;24(4):183-188 TCP Transl Clin Pharmacol http://dx.doi.org/10.12793/tcp.2016.24.4.183 Pharmacokinetic characteristics of cilostazol 200 mg controlled-release tablet compared with two cilostazol 100 mg immediate-release tablets (Pletal) after single oral dose in healthy Korean male volunteers ORIGINAL ARTICLE Jin Dong Son1,4, Sang Min Cho2, Youn Woong Choi2, Soo-Hwan Kim3, In Sun Kwon4, Eun-Heui Jin4, Jae Woo Kim4 and Jang Hee Hong1,4,5* 1Department of Medical Science, College of Medicine, Chungnam National University, Daejeon 35015, republic of Korea, 2Korea Unit- ed Pharm.Inc., Seoul 06116, Republic of Korea, 3Caleb Multilab Inc., Seoul 06745, Republic of Korea, 4Clinical Trials Center, Chun- gnam National University Hospital, Daejeon 35015, South Korea, 5Department of Pharmacology, College of Medicine, Chungnam National University, Daejeon 35015, Republic of Korea *Correspondence: J.H. Hong; Tel: +82-42-280-6940, Fax: +82-42-280-6940, E-mail: [email protected] Received 8 Sep 2016 Cilostazol controlled-release (CR) tablets have recently been developed by Korea United Pharm Revised 28 Nov 2016 (Seoul, Korea). The tablets use a patented double CR system, which improves drug compliance by Accepted 29 Nov 2016 allowing “once daily” administration and reduces adverse events by sustaining a more even plasma Keywords concentration for 24 h. We conducted an open, randomized, two-period, two-treatment, cross- Cilostazol, OPC-13015, over study to compare the pharmacokinetic (PK) characteristics and tolerability of cilostazol when OPC-13213, administered to healthy Korean male volunteers as CR or immediate release (IR) tablets (Pletal, bioequivalence, Korea Otsuka Pharmaceutical Co., Gyeonggi-do, Korea). -

Use of Antiplatelet Therapies During Primary Percutaneous Coronary Intervention for Acute Myocardial Infarction
REVIEW Use of antiplatelet therapies during primary percutaneous coronary intervention for acute myocardial infarction Inhibition of platelet function is necessary to achieve successful and long-lasting primary percutaneous coronary intervention (PCI) for acute myocardial infarction. For many years, antiplatelet therapy in the setting of primary PCI consisted of two drugs that inhibit platelet activation (aspirin and clopidogrel) and an intravenous blocker of platelet aggregation (abciximab). The development of new, more potent oral antiplatelet drugs (prasugrel and ticagrelor) as well as new data on clopidogrel dosing regimens limited the use of abciximab after pretreatment with aspirin and clopidogrel. Thus, intracoronary administration of abciximab and the use of small molecule glycoprotein IIb/IIIa blockers (tirofiban or eptifibatide) challenge the contemporary schemes of antiplatelet treatment in primary PCI. We review recently published data with particular attention on patients and drug characteristics and propose an update of existing recommendations. 1 KEYWORDS: acute myocardial infarction n antiplatelet therapy n aspirin n cilostazol Łukasz A Małek n clopidogrel n glycoprotein IIb/IIIa blockers n prasugrel n primary percutaneous & Adam Witkowski†1 coronary intervention n ticagrelor 1Department of Interventional Cardiology & Angiology, Institute of Cardiology, Alpejska 42, Rupture of the vulnerable atherosclerotic many years, antiplatelet therapy in the setting 04‑628 Warsaw, Poland plaque in the coronary artery wall leading of primary PCI included two oral antiplate- †Author for correspondence: Tel.: +48 22 343 4127 to activation and aggregation of platelets to let drugs, which irreversibly block platelet Fax: +48 22 613 3819 form an artery occluding thrombus is the most activation (aspirin and clopidogrel) together [email protected] frequent cause of acute myocardial infarc- with an inhibition of platelet aggregation by tion (AMI) [1–3]. -

New Drugs: T-Score for Transparency
New drugs: T-score for transparency Access to information about drugs is essential for the quality For 2011, the T-score has been revised to include the AusPAR. use of medicines. Pharmaceutical companies and regulatory agencies, such as the Therapeutic Goods Administration The revised T-scores will be as follows: (TGA), hold large quantities of information about individual drugs, but do not always share this information. To encourage T T T manufacturer provided complete clinical evaluation transparency, Australian Prescriber rates companies' willingness to provide clinical information about new drugs. T T manufacturer provided additional useful Table 1 shows how the companies have performed between information January 2009 and December 2010. The TGA is now publishing Australian Public Assessment T manufacturer provided the AusPAR and/or the Reports (AusPARs) for prescription medicines. While the product information Editorial Executive Committee welcomes this move to greater transparency, it will still ask companies to provide the clinical T manufacturer declined to supply data evaluations for their new products. While there are similarities, the AusPAR may not include all the details found in the X manufacturer did not respond to request for data regulator's clinical evaluation. Table 1 Pharmaceutical company responses to requests for clinical evaluation data for drugs marketed Jan 2009 – Dec 2010 Company Drug T T T manufacturer provided clinical evaluation Amgen denosumab Ferring degarelix Pfizer anidulafungin eletriptan PharmaLink cilostazol Phebra caffeine citrate Roche methoxy polyethylene glycol-epoetin beta tocilizumab Sanofi Pasteur H5N1 influenza vaccine Shire icatibant Wyeth methylnaltrexone T T manufacturer provided additional useful information Abbott omega-3-acid ethyl esters Celgene azacitidine Commercial Eyes melatonin CSL H1N1 influenza vaccine Japanese encephalitis vaccine Eli Lilly prasugrel Table continued.. -

Platelet-Inhibiting Drugs: a Hematologist’S Perspective
Platelet-Inhibiting Drugs: A Hematologist’s Perspective A. Koneti Rao, M.D., Sol Sherry Professor of Medicine Chief, Hematology Section Co-Director, Sol Sherry Thrombosis Research Center Temple University School of Medicine 2012 Chile Akkerman JW, Bouma BN, Sixma JJ. Atlas of Hemostasis, 1979. STRATEGIES FOR ANTITHROMBOTIC THERAPY VASCULAR INJURY RISK FACTOR REDUCTION PLATELET ADHERANCE PLATELET AGGREGATION INHIBITORS COAGULATION ACTIVATION THROMBIN GENERATION ANTICOAGULANTS FIBRIN FORMATION PLASMIN GENERATION THROMBOLYTICS FIBRINOLYSIS AKR/2003 Platelet Responses to Activation Membrane Shape Change Aggregation Dense AGONIST Receptor Granule Secretion Thromboxane Alpha Granule Production TxA2 Acid Hydrolase ADP / Serotonin Rao/2010 GPIIb/IIIa GPIIb/IIIa Fibrinogen GPIIb/IIIa GPVI GPIa/IIa a5b1 GPIb/V/IX GPIV Damaged vWF Fibronectin Endothelium Collagen AKR/2004 Platelet-Inhibiting Drugs Platelet Inhibiting Drugs Aspirin Sulfinpyrazone Dipyridamole P2Y12 Antagonists • Thienopyridines - Ticlopidine, Clopidogrel, Prasugrel (Effient) • Non-Thienopyridine - Ticagrelor (Brilinta) GPIIb/IIIa Inhibitors Abciximab (c7E3 Fab, ReoPro) Eptifibatide (Integrilin) Tirofiban (Aggrastat) Cilostazol (Pletal) AKR-2012 Cyclooxygenase Arachidonic Acid Ser OH 529 COOH OCOCH 3 PGG2, PGH2 Aspirin Cyclooxygenase Thromboxane A2 Ser OCOCH 3 AKR/09 529 GPIIb-IIIa cAMP Fibrinogen ADP (P2Y12) Gi AC Aggregation Ticlopidine P ATP Pleckstrin Clopidogrel GP IIb/IIIa Prasugrel PKC Antagonists TxA2 ADP Gq Secretion (P2Y1) DG TS Gq PGG2/PGH2 Thrombin PLC PIP2 CO Aspirin -

Antithrombotic Therapy for Secondary Prevention in Patients with Non-Cardioembolic Stroke Or Transient Ischemic Attack: a Systematic Review
life Review Antithrombotic Therapy for Secondary Prevention in Patients with Non-Cardioembolic Stroke or Transient Ischemic Attack: A Systematic Review Dániel Tornyos , Alexandra Bálint ,Péter Kupó, Oumaima El Alaoui El Abdallaoui and András Komócsi * Department of Interventional Cardiology, Heart Institute, Medical School, University of Pécs, Ifjúság útja 13, 7624 Pécs, Hungary; [email protected] (D.T.); [email protected] (A.B.); [email protected] (P.K.); [email protected] (O.E.A.E.A.) * Correspondence: [email protected]; Tel.: +36-72-536-001; Fax: +36-72-536-387 Abstract: Stroke embodies one of the leading causes of death and disability worldwide. We aimed to provide a comprehensive insight into the effectiveness and safety of antiplatelet agents and anticoagulants in the secondary prevention of ischemic stroke or transient ischemic attack. A systematic search for randomized controlled trials, comparing antiplatelet or anticoagulant therapy versus aspirin or placebo among patients with ischemic stroke or transient ischemic attack, was performed in order to summarize data regarding the different regimens. Keyword-based searches in the MEDLINE, EMBASE, and Cochrane Library databases were conducted until the 1st of January 2021. Our search explored 46 randomized controlled trials involving ten antiplatelet agents, six combinations with aspirin, and four anticoagulant therapies. The review of the literature reflects Citation: Tornyos, D.; Bálint, A.; that antiplatelet therapy improves outcome in patients with ischemic stroke or transient ischemic Kupó, P.; El Abdallaoui, O.E.A.; attack. Monotherapy proved to be an effective and safe choice, especially in patients with a high risk Komócsi, A. Antithrombotic Therapy of bleeding. -
A Randomized, Controlled Trial Comparing Cilostazol with Extended Release Dipyridamole in the Management of Intermittent Claudication in Peripheral Artery Disease
1 IRB PROTOCOL Geetha F. Pinto, MD Dec 18th, 2007 2 A Randomized, Controlled Trial Comparing Cilostazol with Extended Release Dipyridamole in the Management of Intermittent Claudication in Peripheral Artery Disease A. Study Purpose: The main goal of this prospective, double-blinded, randomized, controlled, trial is to compare the efficacy of extended-release dipyridamole with cilostazol in the management of lower extremity claudication in patients with peripheral vascular disease (PAD). B. Rationale: Intermittent claudication (IC) is defined as a reproducible discomfort of a defined group of muscles which is induced by exercise and relieved with rest. The symptoms result from an imbalance between supply and demand of blood flow that fails to satisfy ongoing metabolic requirements. [1] Not only is PAD now considered coronary heart disease (CHD) equivalent, symptomatic PAD contributes significantly to the morbidity and quality of life in patients with IC. The prevalence of IC would appear to increase from about 3% in patients aged 40 to 6% in patients aged 60 years. [2] Despite this prevalence, the treatment options for IC are limited. The Trans-Atlantic Inter-Society Consensus Document on Management of Peripheral Arterial Disease II (TASC II), a working group of expert representatives recently published a summary of all the evidence for the particular drug therapies available for the management of IC in the United States being limited to cilostazol, a phosphodiesterase III inhibitor with vasodilator, metabolic and antiplatelet activity. Though many other drugs have been studied including other vasoactive and antiplatelet agents, only one other drug, naftidrofuryl ( l5- hydroxytryptamine type 2 antagonist), a drug available only in Europe has shown comparable efficacy in the management of IC. -

Co-Loaded Curcumin and Methotrexate Nanocapsules Enhance Cytotoxicity Against Non-Small-Cell Lung Cancer Cells
molecules Article Co-Loaded Curcumin and Methotrexate Nanocapsules Enhance Cytotoxicity against Non-Small-Cell Lung Cancer Cells Loanda Aparecida Cabral Rudnik 1, Paulo Vitor Farago 1,2, Jane Manfron Budel 1,* , Amanda Lyra 1 , Fernanda Malaquias Barboza 1, Traudi Klein 1, Carla Cristine Kanunfre 3, Jessica Mendes Nadal 1, Matheus Coelho Bandéca 4, Vijayasankar Raman 5 , Andressa Novatski 1, Alessandro Dourado Loguércio 1 and Sandra Maria Warumby Zanin 2 1 Postgraduate Program in Pharmaceutical Sciences, Department of Pharmaceutical Sciences, State University of Ponta Grossa, 84030-900 Ponta Grossa, Brazil; [email protected] (L.A.C.R.); [email protected] (P.V.F.); [email protected] (A.L.); [email protected] (F.M.B.); [email protected] (T.K.); [email protected] (J.M.N.); [email protected] (A.N.); [email protected] (A.D.L.) 2 Postgraduate Program in Pharmaceutical Sciences, Department of Pharmacy, Federal University of Paraná, 81020-430 Curitiba, Brazil; [email protected] 3 Postgraduate Program in Biomedical Science, Department of General Biology, State University of Ponta Grossa, 84030-900 Ponta Grossa, Brazil; [email protected] 4 Postgraduate Program in Dentistry, Ceuma University, 65065-470 São Luís, Brazil; [email protected] 5 National Center for Natural Products Research, School of Pharmacy, University of Mississippi, University, MS 38677, USA; [email protected] * Correspondence: [email protected]; Tel.: +55-42-3220-3124 Academic Editor: Maria Carla Marcotullio Received: 6 March 2020; Accepted: 17 April 2020; Published: 21 April 2020 Abstract: Background: As part of the efforts to find natural alternatives for cancer treatment and to overcome the barriers of cellular resistance to chemotherapeutic agents, polymeric nanocapsules containing curcumin and/or methotrexate were prepared by an interfacial deposition of preformed polymer method.