Guideline/Protocol Title: GUIDELINES for the USE of ANTITHROMBOTIC AGENTS in the SETTING of NEURAXIAL PROCEDURES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
USOO9498481 B2 (12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao et al. (45) Date of Patent: *Nov. 22, 2016 (54) CYCLOPROPYL MODULATORS OF P2Y12 WO WO95/26325 10, 1995 RECEPTOR WO WO99/O5142 2, 1999 WO WOOO/34283 6, 2000 WO WO O1/92262 12/2001 (71) Applicant: Apharaceuticals. Inc., La WO WO O1/922.63 12/2001 olla, CA (US) WO WO 2011/O17108 2, 2011 (72) Inventors: Tadimeti Rao, San Diego, CA (US); Chengzhi Zhang, San Diego, CA (US) OTHER PUBLICATIONS Drugs of the Future 32(10), 845-853 (2007).* (73) Assignee: Auspex Pharmaceuticals, Inc., LaJolla, Tantry et al. in Expert Opin. Invest. Drugs (2007) 16(2):225-229.* CA (US) Wallentin et al. in the New England Journal of Medicine, 361 (11), 1045-1057 (2009).* (*) Notice: Subject to any disclaimer, the term of this Husted et al. in The European Heart Journal 27, 1038-1047 (2006).* patent is extended or adjusted under 35 Auspex in www.businesswire.com/news/home/20081023005201/ U.S.C. 154(b) by Od en/Auspex-Pharmaceuticals-Announces-Positive-Results-Clinical M YW- (b) by ayS. Study (published: Oct. 23, 2008).* This patent is Subject to a terminal dis- Concert In www.concertpharma. com/news/ claimer ConcertPresentsPreclinicalResultsNAMS.htm (published: Sep. 25. 2008).* Concert2 in Expert Rev. Anti Infect. Ther. 6(6), 782 (2008).* (21) Appl. No.: 14/977,056 Springthorpe et al. in Bioorganic & Medicinal Chemistry Letters 17. 6013-6018 (2007).* (22) Filed: Dec. 21, 2015 Leis et al. in Current Organic Chemistry 2, 131-144 (1998).* Angiolillo et al., Pharmacology of emerging novel platelet inhibi (65) Prior Publication Data tors, American Heart Journal, 2008, 156(2) Supp. -

Cangrelor Ameliorates CLP-Induced Pulmonary Injury in Sepsis By
Luo et al. Eur J Med Res (2021) 26:70 https://doi.org/10.1186/s40001-021-00536-4 European Journal of Medical Research RESEARCH Open Access Cangrelor ameliorates CLP-induced pulmonary injury in sepsis by inhibiting GPR17 Qiancheng Luo1†, Rui Liu2†, Kaili Qu3, Guorong Liu1, Min Hang1, Guo Chen1, Lei Xu1, Qinqin Jin1 , Dongfeng Guo1* and Qi Kang1* Abstract Background: Sepsis is a common complication of severe wound injury and infection, with a very high mortality rate. The P2Y12 receptor inhibitor, cangrelor, is an antagonist anti-platelet drug. Methods: In our study, we investigated the protective mechanisms of cangrelor in CLP-induced pulmonary injury in sepsis, using C57BL/6 mouse models. Results: TdT-mediated dUTP Nick-End Labeling (TUNEL) and Masson staining showed that apoptosis and fbrosis in lungs were alleviated by cangrelor treatment. Cangrelor signifcantly promoted surface expression of CD40L on platelets and inhibited CLP-induced neutrophils in Bronchoalveolar lavage fuid (BALF) (p < 0.001). We also found that cangrelor decreased the infammatory response in the CLP mouse model and inhibited the expression of infamma- tory cytokines, IL-1β (p < 0.01), IL-6 (p < 0.05), and TNF-α (p < 0.001). Western blotting and RT-PCR showed that cangre- lor inhibited the increased levels of G-protein-coupled receptor 17 (GPR17) induced by CLP (p < 0.001). Conclusion: Our study indicated that cangrelor repressed the levels of GPR17, followed by a decrease in the infam- matory response and a rise of neutrophils in BALF, potentially reversing CLP-mediated pulmonary injury during sepsis. Keywords: Sepsis, Infammation, Cangrelor, Platelet, GPR17 Background Te lung is one of the initial target organ of the systemic Sepsis is a serious disease and will lead a high mortal- infammatory response caused by sepsis, leading to alve- ity rate of approximately 22% in all over the world [1]. -

Kengrexal, INN-Cangrelor Tetrasodium
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Kengrexal 50 mg powder for concentrate for solution for injection/infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains cangrelor tetrasodium corresponding to 50 mg cangrelor. After reconstitution 1 mL of concentrate contains 10 mg cangrelor. After dilution 1 mL of solution contains 200 micrograms cangrelor. Excipient with known effect Each vial contains 52.2 mg sorbitol. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder for concentrate for solution for injection/infusion. White to off-white lyophilised powder. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Kengrexal, co-administered with acetylsalicylic acid (ASA), is indicated for the reduction of thrombotic cardiovascular events in adult patients with coronary artery disease undergoing percutaneous coronary intervention (PCI) who have not received an oral P2Y12 inhibitor prior to the PCI procedure and in whom oral therapy with P2Y12 inhibitors is not feasible or desirable. 4.2 Posology and method of administration Kengrexal should be administered by a physician experienced in either acute coronary care or in coronary intervention procedures and is intended for specialised use in an acute and hospital setting. Posology The recommended dose of Kengrexal for patients undergoing PCI is a 30 micrograms/kg intravenous bolus followed immediately by 4 micrograms/kg/min intravenous infusion. The bolus and infusion should be initiated prior to the procedure and continued for at least two hours or for the duration of the procedure, whichever is longer. At the discretion of the physician, the infusion may be continued for a total duration of four hours, see section 5.1. -

Characterising the Risk of Major Bleeding in Patients With
EU PE&PV Research Network under the Framework Service Contract (nr. EMA/2015/27/PH) Study Protocol Characterising the risk of major bleeding in patients with Non-Valvular Atrial Fibrillation: non-interventional study of patients taking Direct Oral Anticoagulants in the EU Version 3.0 1 June 2018 EU PAS Register No: 16014 EMA/2015/27/PH EUPAS16014 Version 3.0 1 June 2018 1 TABLE OF CONTENTS 1 Title ........................................................................................................................................... 5 2 Marketing authorization holder ................................................................................................. 5 3 Responsible parties ................................................................................................................... 5 4 Abstract ..................................................................................................................................... 6 5 Amendments and updates ......................................................................................................... 7 6 Milestones ................................................................................................................................. 8 7 Rationale and background ......................................................................................................... 9 8 Research question and objectives .............................................................................................. 9 9 Research methods .................................................................................................................... -
Sulodexide: Review of Recent Clinical Efficacy Data
ISSN 2277-0879; Volume 2, Issue 5, pp. 57-61; May, 2013 Online Journal of Medicine and Medical Science Research ©2013 Online Research Journals Review Article Available Online at http://www.onlineresearchjournals.org/JMMSR Sulodexide: Review of recent clinical efficacy data Massimo Milani MD Private practice, Milan Italy, Via A. Nota 18, Milan, Italy. E-Mail: [email protected]. Received 17 April, 2013 Accepted 8 May, 2013 Sulodexide (SLX) is a peculiar and interesting antithrombotic drug. It is a highly purified mixture of glycosaminoglycans (GAG) with anticoagulant and antithrombotic properties used for the prophylaxis and treatment of thromboembolic diseases. The pharmacological effects of SLX differ substantially from other GAG and are mainly characterized by a prolonged half-life and reduced effect on global coagulation and bleeding parameters. SLX is able to potentiate the antiprotease activities of both antithrombin III and heparin cofactor II. SLX shows also in vitro and in vivo profibrinolytic actions. SLX exhibits antithrombotic and profibrinolytic properties in several animal models of venous and arterial thrombosis and has relatively high affinity for endothelial cells. By oral route SLX is able to release tissue plasminogen activator and increase fibrinolytic activities. SLX is clinically effective in the treatment of peripheral arterial vascular diseases and in the treatment of deep venous thrombosis. SLX has also been found clinically active in the treatment of venous ulcers of the leg. SLX has been also used with success in tinnitus and in the thrombosis of central ocular vein. Recent data suggest that SLX could have beneficial effects in the treatment of diabetic nephropathy and in reducing microalbuminuria. -

P2 Receptors in Cardiovascular Regulation and Disease
Purinergic Signalling (2008) 4:1–20 DOI 10.1007/s11302-007-9078-7 REVIEW P2 receptors in cardiovascular regulation and disease David Erlinge & Geoffrey Burnstock Received: 3 May 2007 /Accepted: 22 August 2007 /Published online: 21 September 2007 # Springer Science + Business Media B.V. 2007 Abstract The role of ATP as an extracellular signalling Introduction molecule is now well established and evidence is accumulating that ATP and other nucleotides (ADP, UTP and UDP) play Ever since the first proposition of cell surface receptors for important roles in cardiovascular physiology and pathophysi- nucleotides [1, 2], it has become increasingly clear that, in ology, acting via P2X (ion channel) and P2Y (G protein- addition to functioning as an intracellular energy source, the coupled) receptors. In this article we consider the dual role of purines and pyrimidines ATP, adenosine diphosphate ATP in regulation of vascular tone, released as a cotransmitter (ADP), uridine triphosphate (UTP) and uridine diphosphate from sympathetic nerves or released in the vascular lumen in (UDP) can serve as important extracellular signalling response to changes in blood flow and hypoxia. Further, molecules [3, 4] acting on 13 P2X homo- and heteromul- purinergic long-term trophic and inflammatory signalling is timer ionotropic and 8 P2Y metabotropic receptor subtypes described in cell proliferation, differentiation, migration and [5, 6] (Table 1). To terminate signalling, ectonucleotidases death in angiogenesis, vascular remodelling, restenosis and are present in the circulation and on cell surfaces, rapidly atherosclerosis. The effects on haemostasis and cardiac degrading extracellular ATP into ADP, AMP and adenosine regulation is reviewed. The involvement of ATP in vascular [7, 8]. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

A Comparative Study of Molecular Structure, Pka, Lipophilicity, Solubility, Absorption and Polar Surface Area of Some Antiplatelet Drugs
International Journal of Molecular Sciences Article A Comparative Study of Molecular Structure, pKa, Lipophilicity, Solubility, Absorption and Polar Surface Area of Some Antiplatelet Drugs Milan Remko 1,*, Anna Remková 2 and Ria Broer 3 1 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Comenius University in Bratislava, Odbojarov 10, SK-832 32 Bratislava, Slovakia 2 Department of Internal Medicine, Faculty of Medicine, Slovak Medical University, Limbová 12, SK–833 03 Bratislava, Slovakia; [email protected] 3 Department of Theoretical Chemistry, Zernike Institute for Advanced Materials, University of Groningen, Nijenborgh 4, 9747 AG Groningen, The Netherlands; [email protected] * Correspondence: [email protected]; Tel.: +421-2-5011-7291 Academic Editor: Michael Henein Received: 18 February 2016; Accepted: 11 March 2016; Published: 19 March 2016 Abstract: Theoretical chemistry methods have been used to study the molecular properties of antiplatelet agents (ticlopidine, clopidogrel, prasugrel, elinogrel, ticagrelor and cangrelor) and several thiol-containing active metabolites. The geometries and energies of most stable conformers of these drugs have been computed at the Becke3LYP/6-311++G(d,p) level of density functional theory. Computed dissociation constants show that the active metabolites of prodrugs (ticlopidine, clopidogrel and prasugrel) and drugs elinogrel and cangrelor are completely ionized at pH 7.4. Both ticagrelor and its active metabolite are present at pH = 7.4 in neutral undissociated form. The thienopyridine prodrugs ticlopidine, clopidogrel and prasugrel are lipophilic and insoluble in water. Their lipophilicity is very high (about 2.5–3.5 logP values). The polar surface area, with regard to the structurally-heterogeneous character of these antiplatelet drugs, is from very large interval of values of 3–255 Å2. -

Cilostazol Protects Rats Against Alcohol‑Induced Hepatic Fibrosis Via Suppression of TGF‑Β1/CTGF Activation and the Camp/Epac1 Pathway
EXPERIMENTAL AND THERAPEUTIC MEDICINE 17: 2381-2388, 2019 Cilostazol protects rats against alcohol‑induced hepatic fibrosis via suppression of TGF‑β1/CTGF activation and the cAMP/Epac1 pathway KUN HAN, YANTING ZHANG and ZHENWEI YANG Department of Gastroenterology, Xi'an Central Hospital, Xi'an, Shaanxi 710003, P.R. China Received July 2, 2018; Accepted November 23, 2018 DOI: 10.3892/etm.2019.7207 Abstract. Alcohol abuse and chronic alcohol consump- Introduction tion are major causes of alcoholic liver disease worldwide, particularly alcohol‑induced hepatic fibrosis (AHF). Liver Liver fibrosis is a wound‑healing response to a variety of liver fibrosis is an important public health concern because of its insults, including excessive alcohol intake. Alcohol abuse and high morbidity and mortality. The present study examined chronic alcohol consumption are major causes of alcoholic the mechanisms and effects of the phosphodiesterase III liver disease (ALD) worldwide (1). Alcohol‑induced hepatic inhibitor cilostazol on AHF. Rats received alcohol infu- fibrosis (AHF) may cause serious hepatic cirrhosis, and is sions via gavage to induce liver fibrosis and were treated widely accepted as a milestone event in ALD (2). However, with colchicine (positive control) or cilostazol. The serum recent evidence indicates that liver fibrosis is reversible and alcohol dehydrogenase (ADH) and acetaldehyde dehydro- that the liver may recover from cirrhosis (3). Therefore, eluci- genase (ALDH) activities and the albumin/globulin (A/G), dation of the cellular and molecular mechanisms is urgently enzymes and hyaluronic acid (HA), type III precollagen required to prevent AHF. (PC III), laminin (LA), and type IV collagen (IV‑C) levels The exact mechanism remains unclear, but certain changes were measured using commercially available kits. -
Wo 2010/075090 A2
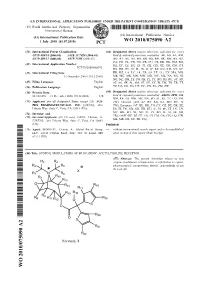
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Treatment for Superficial Thrombophlebitis of The
Treatment for superficial thrombophlebitis of the leg (Review) Di Nisio M, Wichers IM, Middeldorp S This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2012, Issue 3 http://www.thecochranelibrary.com Treatment for superficial thrombophlebitis of the leg (Review) Copyright © 2012 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 5 Figure1. ..................................... 7 Figure2. ..................................... 8 DISCUSSION ..................................... 11 AUTHORS’CONCLUSIONS . 12 ACKNOWLEDGEMENTS . 12 REFERENCES ..................................... 12 CHARACTERISTICSOFSTUDIES . 17 DATAANDANALYSES. 42 Analysis 1.1. Comparison 1 Fondaparinux versus placebo, Outcome 1 Pulmonary embolism. 51 Analysis 1.2. Comparison 1 Fondaparinux versus placebo, Outcome 2 Deep vein thrombosis. 51 Analysis 1.3. Comparison 1 Fondaparinux versus placebo, Outcome 3 Deep vein thrombosis and pulmonary embolism. 52 Analysis 1.4. Comparison 1 Fondaparinux versus placebo, Outcome 4 Extension of ST. 52 Analysis 1.5. Comparison 1 Fondaparinux versus placebo, Outcome 5 Recurrence of ST. 53 Analysis 1.6. Comparison 1 Fondaparinux