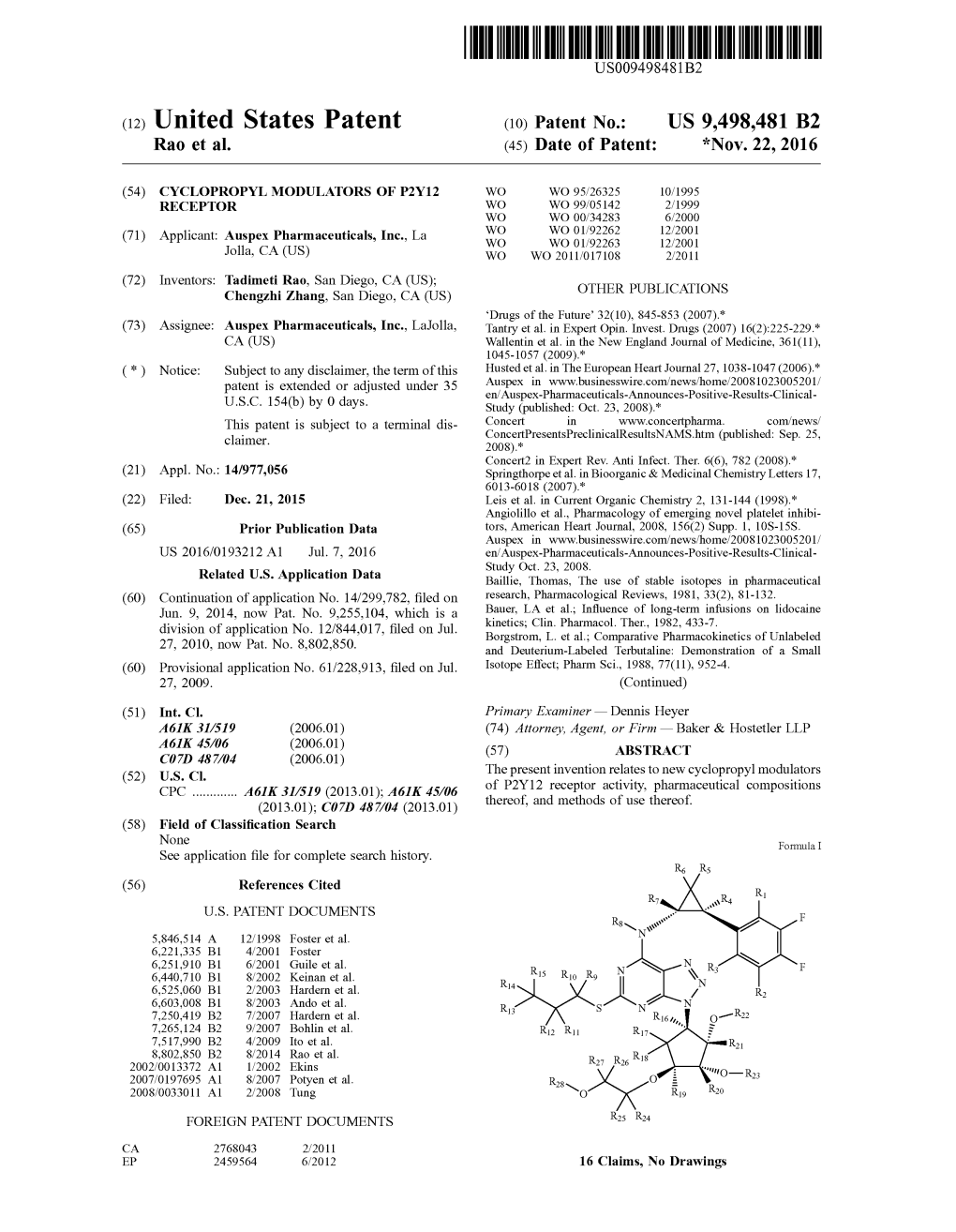
(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UC San Francisco Electronic Theses and Dissertations
UCSF UC San Francisco Electronic Theses and Dissertations Title Machine Learning for Medical Image Analysis and Compound-Target Interactions Permalink https://escholarship.org/uc/item/8c54b5m7 Author Gaskins, Garrett Publication Date 2020 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California Machine Learning for Medical Image Analysis and Compound-Target Interactions by Garrett Gaskins DISSERTATION Submitted in partial satisfaction of the requirements for degree of DOCTOR OF PHILOSOPHY in Biological and Medical Informatics in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, SAN FRANCISCO Approved: ______________________________________________________________________________Michael J Keiser Chair ______________________________________________________________________________Jason Gestwicki ______________________________________________________________________________Sourav Bandyopadhyay ______________________________________________________________________________ ______________________________________________________________________________ Committee Members Copyright 2020 by Garrett Gaskins ii ACKNOWLEDGEMENTS The graduate process is quite an experience. There is a subtle difficulty in describing it, as a peculiar quality of its existence is defined by the uniqueness of it all. Everyone I’ve known to be a part of or to have gone through graduate school has described a truly different journey. Perhaps this is integral to what makes the whole thing work. At the least, -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

(12) United States Patent (10) Patent No.: US 6,469,065 B1 Garvey Et Al
USOO6469.065B1 (12) United States Patent (10) Patent No.: US 6,469,065 B1 Garvey et al. (45) Date of Patent: Oct. 22, 2002 (54) NITROSATED AND NITROSYLATED 5,612,314 A 3/1997 Stamler et al. C-ADRENERGIC RECEPTOR ANTAGONIST, 5,635,204 A 6/1997 Gevirtz et al. .............. 424/449 COMPOSITIONS AND METHODS OF USE 5,646,181 A 7/1997 Fung et al. 5,648,393 A 7/1997 Stamler et al. 5,698,589 A 12/1997 Allen (75) Inventors: David S. Garvey, Dover; Joseph D. 5,731,339 A 3/1998 Lowrey Schroeder, Dedham, both of MA (US); 5,767,160 A 6/1998 Kaesemeyer Inigo Saenez de Tejada, Madrid (ES); 5,773,457 A 6/1998 Nahoum Ricky D. Gaston, Malden, MA (US); 5,789.442 A 8/1998 Garfield et al. Tatiana E. Shelekhin, Acton, MA 5,877,216 A 3/1999 Place et al. (US); Tiansheng Wang, Concord, MA (US) FOREIGN PATENT DOCUMENTS EP O346297 12/1989 (73) Assignee: NitroMed, Inc., Bedford, MA (US) EP O357581 3/1990 EP O432199 6/1991 (*) Notice: Subject to any disclaimer, the term of this FR 2547SO1 12/1984 patent is extended or adjusted under 35 JP 8O26962 1/1998 U.S.C. 154(b) by 0 days. WO 97/27749 * 8/1997 WO 97.27749 8/1997 WO 97.42.946 11/1997 (21) Appl. No.: 09/387,724 WO 9852569 11/1998 Filed: Sep. 1, 1999 WO 99.01132 1/1999 (22) WO 9907353 2/1999 WO 99.07695 2/1999 Related U.S. -

Zebrafish Behavioral Profiling Links Drugs to Biological Targets and Rest/Wake Regulation
www.sciencemag.org/cgi/content/full/327/5963/348/DC1 Supporting Online Material for Zebrafish Behavioral Profiling Links Drugs to Biological Targets and Rest/Wake Regulation Jason Rihel,* David A. Prober, Anthony Arvanites, Kelvin Lam, Steven Zimmerman, Sumin Jang, Stephen J. Haggarty, David Kokel, Lee L. Rubin, Randall T. Peterson, Alexander F. Schier* *To whom correspondence should be addressed. E-mail: [email protected] (A.F.S.); [email protected] (J.R.) Published 15 January 2010, Science 327, 348 (2010) DOI: 10.1126/science.1183090 This PDF file includes: Materials and Methods SOM Text Figs. S1 to S18 Table S1 References Supporting Online Material Table of Contents Materials and Methods, pages 2-4 Supplemental Text 1-7, pages 5-10 Text 1. Psychotropic Drug Discovery, page 5 Text 2. Dose, pages 5-6 Text 3. Therapeutic Classes of Drugs Induce Correlated Behaviors, page 6 Text 4. Polypharmacology, pages 6-7 Text 5. Pharmacological Conservation, pages 7-9 Text 6. Non-overlapping Regulation of Rest/Wake States, page 9 Text 7. High Throughput Behavioral Screening in Practice, page 10 Supplemental Figure Legends, pages 11-14 Figure S1. Expanded hierarchical clustering analysis, pages 15-18 Figure S2. Hierarchical and k-means clustering yield similar cluster architectures, page 19 Figure S3. Expanded k-means clustergram, pages 20-23 Figure S4. Behavioral fingerprints are stable across a range of doses, page 24 Figure S5. Compounds that share biological targets have highly correlated behavioral fingerprints, page 25 Figure S6. Examples of compounds that share biological targets and/or structural similarity that give similar behavioral profiles, page 26 Figure S7. -

Customs Tariff - Schedule
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2020 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT, CEUT, UAT, CPTPT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Subject Index
Subject Index A-64662 497 classification 11-14 AA-861 511 (fig) function 111-114 acebutolol 69,70 hemodynamic effects 110-121 brand names 868 (table) in hypertensive disease 114 dosage 83 (table), 860 (table) mechanism of action 110-121 intrinsic sympathomimetic activity 82 metabolism 108-110 pharmacological profile 83 (table) pharmacodynamics 110-121 see also diuretics 83 pharmacokinetics 108-110 acetazolamide 22, 24 sUbtypes 111,241-246 chemical structure 23 (fig), 24 (table) a2- 246 duration of action 39 (table) classification at central cardiovascular fractional sodium excretion 30 (table) sites 242-244 metabolism 37 definition at peripheral sites onset of action 39 (table) 241-242 peak of action 39 (table) a-adrenoceptor agonists 113 (table) pKa 37 (table) a-adrenoceptor antagonists 15, 105-125 plasma elimination half-life 37 antihypertensive activity 114-119 protein binding 37 (table) chemistry 106-108 renal site/mechanism of action 26, 30 combination with other drugs 123 (table) contraindications 123-124 site of action 29 differential antagonism 242 teratogenesis 800,800-802 dosage 121-123 tubular fluid/plasma-sodium drug interactions 123 concentrations ratio 30 (fig) effects on: c10nidine 240-241 see also diuretics guanfacine 240-241 acetylcholine 316 a-methyldopa 240-241 acetylsalicylic acid 53 hemodynamic profile 119-120 Actinomycetales extracts/compounds side effects 124 728 therapeutic use 121-123 adenosine-3, 5-cyclic monophosphate toxicity 124 (cAMP) 73 ~-adrenoceptor antagonists 66-67, 815 adenosine triphosphate 73,268 a-adrenoceptor -

Adrenoceptor Subtype 1Ian Marshall, Richard P
Brifish Journal of Pharmacology (I995) 115, 781 - 786 1995 Stockton Press All rights reserved 0007-1188/95 $12.00 X Noradrenaline contractions of human prostate mediated by aClA- (cxlc) adrenoceptor subtype 1Ian Marshall, Richard P. Burt & *Christopher R. Chapple Department of Pharmacology, University College London, Gower Street, London WC1E 6BT and *Department of Urology, The Royal Hallamshire Hospital, Glossop Road, Sheffield SlO 2JF 1 The subtype of a1-adrenoceptor mediating contractions of human prostate to noradrenaline was characterized by use of a range of competitive and non-competitive antagonists. 2 Contractions of the prostate to either noradrenaline (pD2 5.5), phenylephrine (pD2 5.1) or methoxamine (pD2 4.4) were unaltered by the presence of neuronal and extraneuronal uptake blockers. Noradrenaline was about 3 and 10 times more potent than phenylephrine and methoxamine respectively. Phenylephrine and methoxamine were partial agonists. 3 Pretreatment with the alkylating agent, chlorethylclonidine (10-4 M) shifted the noradrenaline concentration-contraction curve about 3 fold to the right and depressed the maximum response by 31%. This shift is 100 fold less than that previously shown to be produced by chlorethylclonidine under the same conditions on OlB-adrenoceptor-mediated contractions. 4 Cumulative concentration-contraction curves for noradrenaline were competitively antagonized by WB 4101 (pA2 9.0), 5-methyl-urapidil (pA2 8.6), phentolamine (pA2 7.6), benoxathian (pA2 8.5), spiperone (pA2 7.3), indoramin (pA2 8.2) and BMY 7378 (pA2 6.6). These values correlated best with published pKi values for their displacement of [3H]-prazosin binding on membranes expressing cloned oczc-adrenoceptors and poorly with values from cloned lb- and cld-adrenoceptors. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0115729 A1 Qin Et Al
US 201201.15729A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0115729 A1 Qin et al. (43) Pub. Date: May 10, 2012 (54) PROCESS FOR FORMING FILMS, FIBERS, Publication Classification AND BEADS FROM CHITNOUS BOMASS (51) Int. Cl (75) Inventors: Ying Qin, Tuscaloosa, AL (US); AOIN 25/00 (2006.01) Robin D. Rogers, Tuscaloosa, AL A6II 47/36 (2006.01) AL(US); (US) Daniel T. Daly, Tuscaloosa, tish 9.8 (2006.01)C (52) U.S. Cl. ............ 504/358:536/20: 514/777; 426/658 (73) Assignee: THE BOARD OF TRUSTEES OF THE UNIVERSITY OF 57 ABSTRACT ALABAMA, Tuscaloosa, AL (US) (57) Disclosed is a process for forming films, fibers, and beads (21) Appl. No.: 13/375,245 comprising a chitinous mass, for example, chitin, chitosan obtained from one or more biomasses. The disclosed process (22) PCT Filed: Jun. 1, 2010 can be used to prepare films, fibers, and beads comprising only polymers, i.e., chitin, obtained from a suitable biomass, (86). PCT No.: PCT/US 10/36904 or the films, fibers, and beads can comprise a mixture of polymers obtained from a suitable biomass and a naturally S3712). (4) (c)(1), Date: Jan. 26, 2012 occurring and/or synthetic polymer. Disclosed herein are the (2), (4) Date: an. AO. films, fibers, and beads obtained from the disclosed process. O O This Abstract is presented solely to aid in searching the sub Related U.S. Application Data ject matter disclosed herein and is not intended to define, (60)60) Provisional applicationpp No. 61/182,833,sy- - - s filed on Jun. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

Attenuated 5-Hydroxytryptamine Receptor-Mediated Responses in Aortae from Streptozotocin-Induced Diabetic Rats G.M
Br. J. Pharmacol. (1994), 111, 370-376 '." Macmillan Press Ltd, 1994 Attenuated 5-hydroxytryptamine receptor-mediated responses in aortae from streptozotocin-induced diabetic rats G.M. James, 1W.C. Hodgson, E.A. Davis & 2J.M. Haynes Department of Pharmacology, Monash University, Clayton, Victoria, Australia, 3168 1 This study was designed to examine further the attenuated contractile responses to 5-hydroxy- tryptamine (5-HT) previously observed in aortae from diabetic rats. 2 Cumulative concentration-response curves to 5-HT, and the 5-HT receptor agonists, at-methyl 5-HT (a-Me-5-HT, 5-HT21lc agonist), (± )-1-(2,5-dimethoxy-4-iodophenyl)-2-aminopropane (DOI, 5-HT21IC agonist) and 5-carboxamidotryptamine (5-CT, 5-HTIA/1B/1D agonist), were examined in endothelium- intact and -denuded aortae from 2-week streptozotocin (STZ)-diabetic and control rats. 3 In endothelium-intact and -denuded aortae from diabetic rats, maximum responses to 5-HT and a-Me-5-HT were significantly reduced compared to those of aortae from control rats. Responses to these agonists were inhibited by the 5-HT21lc receptor antagonist, ketanserin (0.1 jAM). 4 The attenuated responses to 5-HT of aortae from diabetic rats were normalized by chronic insulin treatment of the rats (5 units day-', s.c.), but not by altering the glucose concentration of the bathing fluid. 5 The nitric oxide synthase inhibitor N-nitro-L-arginine (NOLA, 0.1 mM) significantly potentiated responses to both 5-HT and a-Me-5-HT in endothelium-intact aortae. However, the difference between maximum responses of aortae from diabetic and control rats was still evident in the presence of NOLA.