Joints of Foot.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skeletal Foot Structure
Foot Skeletal Structure The disarticulated bones of the left foot, from above (The talus and calcaneus remain articulated) 1 Calcaneus 2 Talus 3 Navicular 4 Medial cuneiform 5 Intermediate cuneiform 6 Lateral cuneiform 7 Cuboid 8 First metatarsal 9 Second metatarsal 10 Third metatarsal 11 Fourth metatarsal 12 Fifth metatarsal 13 Proximal phalanx of great toe 14 Distal phalanx of great toe 15 Proximal phalanx of second toe 16 Middle phalanx of second toe 17 Distal phalanx of second toe Bones of the tarsus, the back part of the foot Talus Calcaneus Navicular bone Cuboid bone Medial, intermediate and lateral cuneiform bones Bones of the metatarsus, the forepart of the foot First to fifth metatarsal bones (numbered from the medial side) Bones of the toes or digits Phalanges -- a proximal and a distal phalanx for the great toe; proximal, middle and distal phalanges for the second to fifth toes Sesamoid bones Two always present in the tendons of flexor hallucis brevis Origin and meaning of some terms associated with the foot Tibia: Latin for a flute or pipe; the shin bone has a fanciful resemblance to this wind instrument. Fibula: Latin for a pin or skewer; the long thin bone of the leg. Adjective fibular or peroneal, which is from the Greek for pin. Tarsus: Greek for a wicker frame; the basic framework for the back of the foot. Metatarsus: Greek for beyond the tarsus; the forepart of the foot. Talus (astragalus): Latin (Greek) for one of a set of dice; viewed from above the main part of the talus has a rather square appearance. -

Fractures of the Anterior Process of the Calcaneum; a Review and Proposed Treatment Algorithm
Foot and Ankle Surgery 25 (2019) 258–263 Contents lists available at ScienceDirect Foot and Ankle Surgery journal homepage: www.elsevier.com/locate/fas Review Fractures of the anterior process of the calcaneum; a review and proposed treatment algorithm a, b b b b Baljinder S. Dhinsa *, Ahmed Latif , Roland Walker , Ali Abbasian , Diane Back , b Sam Singh a William Harvey Hospital, Kennington Road, Willesborough, Ashford TN24 0LZ, United Kingdom b Guy’s and St Thomas’ NHS Foundation Trust, Great Maze Pond, London SE1 9RT, United Kingdom A R T I C L E I N F O A B S T R A C T Article history: Background: There remains a lack of recognition of these fractures, which leads to a delay in diagnosis and Received 18 June 2017 appropriate management. Received in revised form 1 February 2018 Methods: A comprehensive literature search was performed. Following inclusion and exclusion criteria, Accepted 3 February 2018 23 studies were available for analysis. Results: Delay in diagnosis is common and has a negative impact on outcome. If an APC fracture is Keywords: suspected; anteroposterior, lateral and oblique plain radiographs should be requested. Further Fracture investigation with computed tomography or magnetic resonance imaging is indicated if plain Calcaneum radiographs are inconclusive and patient remains symptomatic. Non-operative measures are usually Anterior process Avulsion adequate for most undisplaced fractures, however surgical intervention maybe required for large, intra- Compression articular fractures in the acute setting and for non-union. Calcaneocuboid Conclusions: A treatment algorithm is suggested that may help with the diagnosis and management of these injuries. -

Morphological and Biomechanical Implications of Cuboid Facet of the Navicular Bone in the Gait
Int. J. Morphol., 37(4):1397-1403, 2019. Morphological and Biomechanical Implications of Cuboid Facet of the Navicular Bone in the Gait Implicaciones Morfológicas y Biomecánicas de la Faceta Cuboídea del Navicular en la Marcha Eduardo Saldías1; Assumpció Malgosa1; Xavier Jordana1 & Albert Isidro2 SALDÍAS, E.; MALGOSA, A.; JORDANA, X. & ISIDRO, A. Morphological and biomechanical implications of cuboid facet of the navicular bone in the gait. Int. J. Morphol., 37(4):1397-1403, 2019. SUMMARY: The cuboid facet of the navicular bone is an irregular flat surface, present in non-human primates and some human ancestors. In modern humans, it is not always present and it is described as an “occasional finding”. To date, there is not enough data about its incidence in ancient and contemporary populations, nor a biomechanical explanation about its presence or absence. The aim of the study was to evaluate the presence of the cuboid facet in ancient and recent populations, its relationship with the dimensions of the midtarsal bones and its role in the biomechanics of the gait. 354 pairs of naviculars and other tarsal bones from historical and contemporary populations from Catalonia, Spain, have been studied. We used nine measurements applied to the talus, navicular, and cuboid to check its relationship with facet presence. To analyze biomechanical parameters of the facet, X-ray cinematography was used in living patients. The results showed that about 50 % of individuals developed this surface without differences about sex or series. We also observed larger sagittal lengths of the talar facet (LSAGTAL) in navicular bones with cuboid facet. No significant differences were found in the bones contact during any of the phases of the gait. -
Bones of the Upper and Lower Limb
Bones of the Upper and Lower limb Musculoskeletal block- Anatomy-lecture 1 Editing file Objectives Color guide : important in Red ✓ Classify the bones of the three regions of the lower Doctor note in Green limb (thigh, leg and foot). Extra information in Grey ✓ Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula) – Bones of the foot (tarsals, metatarsals and phalanges) ✓ Recognize the side of the bone. Note: this lecture is based on female slides since Prof abuel makarem said only things that are mentioned in the female slides will come in the exam Note : All bones picture which are described in this lecture are bones on the right side of the body Before start :Please make yourself familiar with these terms to better understand the lecture Terms Meaning Example Ridge The long and narrow upper edge, angle, or crest The supracondylar ridges (in the distal part of of something (the humerus The trochlear notch (in the proximal part of the Notch An indentation, (incision) on an edge or surface (ulna A nodule or a small rounded projection on the Tubercles (Dorsal tubercle (in the distal part of the radius bone A hollow place (The Notch is not complete but the Subscapular fossa (in the concave part of the Fossa fossa is complete and both of them act as the lock (scapula (of the joint A large prominence on a bone usually serving for Deltoid tuberosity (in the humorous) and it Tuberosity the attachment of muscles or ligaments (is a connects the deltoid muscle (bigger projection than the Tubercle -

Morphological Characteristics of the Lateral Talocalcaneal Ligament: a Large-Scale Anatomical Study
Surgical and Radiologic Anatomy (2019) 41:25–28 https://doi.org/10.1007/s00276-018-2128-8 ANATOMIC VARIATIONS Morphological characteristics of the lateral talocalcaneal ligament: a large-scale anatomical study Mutsuaki Edama1,2 · Ikuo Kageyama2 · Takaniri Kikumoto1 · Tomoya Takabayashi1 · Takuma Inai1 · Ryo Hirabayashi1 · Wataru Ito1 · Emi Nakamura1 · Masahiro Ikezu1 · Fumiya Kaneko1 · Akira Kumazaki3 · Hiromi Inaba4 · Go Omori3 Received: 9 August 2018 / Accepted: 4 September 2018 / Published online: 30 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose The purpose of this study is to clarify the morphological characteristics of the lateral talocalcaneal ligament (LTCL). Methods This study examined 100 legs from 54 Japanese cadavers. The LTCL was classified into three types: Type I, the LTCL branches from the calcaneofibular ligament (CFL); Type II, the LTCL is independent of the CFL and runs parallel to the calcaneus; and Type III, the LTCL is absent. The morphological features measured were fiber bundle length, fiber bundle width, and fiber bundle thickness. Results The LTCL was classified as Type I in 18 feet (18%), Type II in 24 feet (24%), and Type III in 58 feet (58%). All LTCLs were associated with the anterior talofibular ligament at the talus. There was no significant difference in morphologi- cal characteristics by Type for each ligament. Conclusions The LTCL was similar to the CFL in terms of fiber bundle width and fiber bundle thickness. Keywords Calcaneofibular · Ligament · Subtalar joint · Gross anatomy Introduction features, as well as complex three-dimensional mobility, making it a challenge to conduct quantitative evaluations. Of patients with chronic ankle instability, 42% [6] present Ligaments that are associated with the stability of the with mechanical instability of the talocrural joint, and 58% subtalar joint include the calcaneofibular ligament (CFL), have mechanical instability of the subtalar joint [3], each of the lateral talocalcaneal ligament (LTCL), the interosseous them at high percentages. -

Mcilroy's Ankle Injury Explained
McIlroy’s Ankle Injury Explained By Eva Nugent MISCP The Anterior Talofibular Ligament is big news this week because of world number 1 golf player Rory McIlroy’s injury sustained while having a football “kick about” with friends. McIlroy reports sustaining a “total rupture of his left ATFL and damage to the associated ankle joint capsule”. This unfortunate injury has put his golf season in doubt with the Open Championship starting just next week the 16th of July. But what exactly is the ATFL? And what does the rehabilitation for this injury involve? The Anterior Talofibular Ligament is one of three ligaments that make of the lateral ligament complex of the ankle joint. It originates at the fibular malleoulus of the lateral shin bone (fibula) and runs forward to and attaches to the Talus (ankle bone). The other two ligaments are the Posterior talofibular ligament (PTFL) and the Calcaneofibular ligament (CFL). The function of these ligaments is to provide stability and support to the ankle joint. The ATFL specifically prevents the anterior translation of the shin in relation to the foot/ankle. The ATFL is the most commonly injured ankle ligament and is most vulnerable when the foot is pointing downwards and inwards as the body’s centre of gravity rolls over the ankle (plantarflexed and inverted position). This is commonly described as “going over on your ankle”. It is commonly injured in sports like football or GAA where unpredictable fast turns or cutting movements are involved. This is referred to as an ankle sprain and results in damage to the fibres of the ligament as they are overstretched. -

Anatomy: Lower Leg, Knee, & Patella Positioning
Reading assignment: Lower Leg Anatomy: lower leg, knee, & Merrils, Vol. 1: Chapter 6 Film Critique #3 patella Lab demonstration Positioning: lower leg Positioning: knee Reading assignment: Knee Merrils, Vol. 1: Chapter 6 Film Critique #4 & Lab demonstration Positioning: intercondylar fossa Reading assignment: Intercondylar fossa and patella & patella Merrils, Vol. 1: Chapter 6 Lab demonstration Anatomy: Femur Reading assignment: Femur Positioning: Femur Merrils, Vol. 1: Chapters 6 & 7 Film Critique #5 Lab demonstration Leg…… The leg is composed of two long bones: Tibia – medial bone; second largest bone in the body Fibula – lateral bone The tibia has several anatomical features of note. See whether you can locate each on the diagram. Proximal end: Medial condyle Lateral condyle Tibial plateaus Intercondylar eminence Tibial tuberosity Body – features anterior crest Distal end: Medial malleolus Fibular notch The head of the fibula is located at its proximal end and has a pointed apex laterally. Distally, the fibular features the lateral malleolus. The articulations between the two leg bones are discussed on Screen 1.13. Knee….. The knee joint is the articulation between the femoral condyles and the tibial plateaus. Numerous soft tissues support and reinforce the knee, including the: Menisci Cruciate ligaments Collateral ligaments These supporting soft tissue structures are enclosed in a common joint capsule. The knee joint is of the hinge type, capable of flexion and extension only. The anterior knee joint is protected by the patella and patellofemoral joint. The patella is the largest and most constant sesamoid bone. It develops in the quadriceps femoris tendon between the ages of 3 and 5 years. -
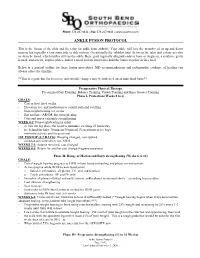
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

SUBTALAR JOINT RECONSTRUCTION by George E
SUBTALAR JOINT RECONSTRUCTION By George E. Quill, Jr., M.D. The single axis subtalar joint is a hinge joining the talus and calcaneus that allows adaptation of the foot on uneven ground. This joint modifies the forces of ambulation imposed on the rest of the skeleton and influences the performance of the more distal foot articulations as well. When the structure and function of this joint are altered by trauma, instability, arthritis, infection, or tarsal coalition, subtalar reconstruction, usually in the form of arthrodesis, may prove to be a very successful procedure in treating the patient's resultant disability. The subtalar joint is, in this author's opinion, a very under appreciated joint. Even though it is estimated that up to 3 percent of the general population may have an asymptomatic talocalcaneal coalition present from a very young age and function very well, patients with a stiffened subtalar joint secondary to post-traumatic subtalar osteoarthrosis have very poor biomechanical function. Many patients presenting with "ankle " pain or who have pain from an ankle sprain that "just won't go away", may actually have subtalar pathology as an etiology for their discomfort. It is the astute orthopaedic surgeon who can recognize and successfully treat this pathology. Subtalar arthrodesis performed for the appropriate indications has proven to be one of this author's most gratifying, time-tested procedures in alleviating pain and improving function in patients so affected. Therefore, it is prudent that we understand the anatomic and functional aspects of the subtalar joint. The subtalar joint consists of three separate facets for articulation between the talus and calcaneus (Figure 1). -

Tarsometatarsal Joint Injury/Arthritis John P
Tarsometatarsal joint injury/arthritis John P. Negrine FRACS Foot and ankle surgeon Dr John Negrine Adult Foot and Ankle surgeon Lisfranc injury • Named after a Napoleonic surgeon who didn’t actually describe the injury – he described am amputation through the joints Dr John Negrine Adult Foot and Ankle surgeon Jacques Lisfranc de St. Martin • 1790 – 1847 • “A surgeon and gynaecologist” • Trained as an assistant to Guillaume Dupuytren • “Pioneered operations including removal of the rectum, lithotomy in women as well as amputation of the cervix” Dr John Negrine Adult Foot and Ankle surgeon What do we call the “Lisfranc joints?” • The tarsometatarsal joints • Anatomy well known to you • The second metatarsal base is recessed and the strong ligament is on the plantar surface connecting the medial cuneiform to the base of the second metatarsal…the “Lisfranc ligament” Dr John Negrine Adult Foot and Ankle surgeon Lisfranc anatomy Dr John Negrine Adult Foot and Ankle surgeon Common injury • Commonly missed • Commonly underestimated • Long time to recovery • Don’t always do well! Dr John Negrine Adult Foot and Ankle surgeon Common ‐ ?Really? • No not really! • 0.2% of fractures • 1:70,000 people in a hospital catchment area • 20% are missed Dr John Negrine Adult Foot and Ankle surgeon Mechanism of injury • 43% Motor vehicle accidents • 24% from falls, jumps or twisting injury • 13% due to crush injury Dr John Negrine Adult Foot and Ankle surgeon Important to differentiate High velocity vs low velocity Dr John Negrine Adult Foot and Ankle surgeon -

Anatomy, Bony Pelvis and Lower Limb, Leg Bones
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Anatomy, Bony Pelvis and Lower Limb, Leg Bones Authors Austin J. Cantrell1; Matthew Varacallo2. Affiliations 1 University of Oklahoma College of Med. 2 Department of Orthopaedic Surgery, University of Kentucky School of Medicine Last Update: January 17, 2019. Introduction The leg is the region of the lower limb between the knee and the foot. It comprises two bones: the tibia and the fibula. The role of these two bones is to provide stability and support to the rest of the body, and through articulations with the femur and foot/ankle and the muscles attached to these bones, provide mobility and the ability to ambulate in an upright position. The tibia articulates with the femur at the knee joint. The knee joint consists of three compartments [1][2] medial tibiofemoral compartment lateral tibiofemoral compartment patellofemoral compartment At the ankle, the tibia and fibula create the articular surface for the talus. The ankle mortise is a specialized articulation providing support and optimizing motion and function through the ankle joint. A normal ankle joint ultimately optimizes and allows for physiologic mobility of the foot and its associated joints and articulations. The bones and fascia also divide the lower leg into four compartments [3][4] anterior compartment lateral compartment posterior compartment, superficial posterior compartment, deep Structure and Function The tibia is the second largest bone in the body and provides support for a significant portion of the weight-bearing forces transmitted from the rest of the body. -

ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique
CHAPTER 22 ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique Thomas A. Brosky, II, DPM Michael C. McGlamry, DPM Marie-Christine Bergeron, DPM Isolated subtalar joint (STJ) fusions are performed routinely as described by Sarraffi an. The talus and calcaneus move by many foot and ankle surgeons for various hindfoot in opposite directions: as the calcaneus abducts, everts and pathologies, but were historically avoided due to their extends, the talus will adduct, invert and plantarfl ex (9). potential complications on the adjacent joints (1). Since the inception of this isolated arthrodesis, multiple studies INDICATIONS have been undertaken to demonstrate the effects on the surrounding joints. Jouveniaux et al concluded with their Isolated STJ arthrodesis is indicated for the following: retrospective study of 37 isolated fusions that radiographic Stage II fl exible fl atfoot deformity, isolated arthritis, both changes suggesting arthritis in the adjacent joints were traumatic and non-traumatic, coalition, and neuromuscular common, but were moderate and asymptomatic in the disease affecting hindfoot motion (10). The literature majority of cases (2). Additionally, this technique is preferred has reported good results for stage II posterior tendon instead of a triple arthrodesis in cases where the calcaneal- dysfunction, but patient selection is the key to success (11). cuboid joint and talo-navicular joints are intact without Forefoot varus can be a contra-indication for this isolated arthritic changes. This preserves the overall function of the procedure unless it is addressed surgically (12). Taylor and hindfoot with the perceived joint stiffness that the triple Sammarco recommend isolated STJ arthrodesis in patients arthrodesis offers (3,4).