Anatomy, Bony Pelvis and Lower Limb, Leg Bones
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Posterior Compartment Of
POSTERIOR COMPARTMENT OF LEG Cross Section of Leg Cutaneous Innervation Superficial vessels of leg Deep Fascia of Posterior Compartment Boundaries and Sub-divisions Flexor Retinaculum Muscles of Posterior Compartment I. Superficial Muscles a) Gastrocnemius b) Soleus c) Plantaris a) Gastrocnemius Origin:- by 2 heads i. Lateral head- lateral aspect of lateral condyle of femur ii. Medial head- popliteal surface of femur above medial condyle Insertion:- Posterior surface of calcaneum as Tendo-calcaneus b) Soleus Origin:- i. Inverted ‘V’ shaped from soleal line on tibia ii. Upper 1/4th of upper surface of shaft of fibula iii. Fibrous arch between these 2 bones Insertion:- Posterior surface of calcaneum as Tendo-calcaneus c) Plantaris- fusiform belly Origin:- Lateral supracondylar ridge of femur Insertion:- Posterior surface of calcaneum medial to Tendo- calcaneus Superficial Strata Deep Strata I. Deep Muscles a) Popliteus b) Flexor Digitorum Longus c) Flexor Hallucis Longus d) Tibialis Posterior a) Popliteus Origin:- Groove on lateral surface of lat. femoral condyle Insertion:- Triangular area on posterior surface of tibia b) Flexor Digitorum Longus Origin:- i. Upper 2/3rds of medial part of post. surface of tibia ii. Fascia covering tibialis posterior Insertion:- Plantar surface of base of distal phalanx of lateral 4 toes a) Flexor Hallucis Longus Origin:- i. Lower 3/4th of post. surface of fibula ii. Interosseous membrane Insertion:- Plantar surface of base of distal phalanx of great toe a) Tibialis Posterior Origin:- i. Upper 2/3rds of lat. Part of posterior surface of tibia ii. Post. Surface of fibula and interosseous membrane Insertion:- Tuberosity of navicular bone Posterior Tibial Artery • Larger terminal branch of Popliteal artery • Branches:- a. -

Anatomy: Lower Leg, Knee, & Patella Positioning
Reading assignment: Lower Leg Anatomy: lower leg, knee, & Merrils, Vol. 1: Chapter 6 Film Critique #3 patella Lab demonstration Positioning: lower leg Positioning: knee Reading assignment: Knee Merrils, Vol. 1: Chapter 6 Film Critique #4 & Lab demonstration Positioning: intercondylar fossa Reading assignment: Intercondylar fossa and patella & patella Merrils, Vol. 1: Chapter 6 Lab demonstration Anatomy: Femur Reading assignment: Femur Positioning: Femur Merrils, Vol. 1: Chapters 6 & 7 Film Critique #5 Lab demonstration Leg…… The leg is composed of two long bones: Tibia – medial bone; second largest bone in the body Fibula – lateral bone The tibia has several anatomical features of note. See whether you can locate each on the diagram. Proximal end: Medial condyle Lateral condyle Tibial plateaus Intercondylar eminence Tibial tuberosity Body – features anterior crest Distal end: Medial malleolus Fibular notch The head of the fibula is located at its proximal end and has a pointed apex laterally. Distally, the fibular features the lateral malleolus. The articulations between the two leg bones are discussed on Screen 1.13. Knee….. The knee joint is the articulation between the femoral condyles and the tibial plateaus. Numerous soft tissues support and reinforce the knee, including the: Menisci Cruciate ligaments Collateral ligaments These supporting soft tissue structures are enclosed in a common joint capsule. The knee joint is of the hinge type, capable of flexion and extension only. The anterior knee joint is protected by the patella and patellofemoral joint. The patella is the largest and most constant sesamoid bone. It develops in the quadriceps femoris tendon between the ages of 3 and 5 years. -

Back of Leg I
Back of Leg I Dr. Garima Sehgal Associate Professor “Only those who risk going too far, can possibly find King George’s Medical University out how far one can go.” UP, Lucknow — T.S. Elliot DISCLAIMER Presentation has been made only for educational purpose Images and data used in the presentation have been taken from various textbooks and other online resources Author of the presentation claims no ownership for this material Learning Objectives By the end of this teaching session on Back of leg – I all the MBBS 1st year students must be able to: • Enumerate the contents of superficial fascia of back of leg • Write a short note on small saphenous vein • Describe cutaneous innervation in the back of leg • Write a short note on sural nerve • Enumerate the boundaries of posterior compartment of leg • Enumerate the fascial compartments in back of leg & their contents • Write a short note on flexor retinaculum of leg- its attachments & structures passing underneath • Describe the origin, insertion nerve supply and actions of superficial muscles of the posterior compartment of leg Introduction- Back of Leg / Calf • Powerful superficial antigravity muscles • (gastrocnemius, soleus) • Muscles are large in size • Inserted into the heel • Raise the heel during walking Superficial fascia of Back of leg • Contains superficial veins- • small saphenous vein with its tributaries • part of course of great saphenous vein • Cutaneous nerves in the back of leg- 1. Saphenous nerve 2. Posterior division of medial cutaneous nerve of thigh 3. Posterior cutaneous -

1 Anatomy – Lower Limb – Bones
Anatomy – Lower limb – Bones Hip (innominate) bone Acetabulum lat, pubic symph ant Ilium, pubis and ischium which fuse in Y-shaped epiphysis involving acetabulum Acetabulum - Articulates with head femur Ilium Iliac crest from ASIS to PSIS Gluteal surface - Three gluteal lines Glut max above superior Glut med between superior-middle Glut min between middle-inferior Pubis Obturator groove lodges obturator nerve/vessels Ischium L-shaped Ischial spine projects medially, divide greater/lesser sciatic notch Lesser sciatic notch forms lesser sciatic foramen due to bridging of sacrotuberous ligament Medial surface Pectineal line, arcuate line Lesser Sciatic Foramen Between lesser sciatic notch ilium and sacrotuberbous/sacrospinous ligaments Contents Tendon obturator internus, Int pudendal artery/vein, pudendal nerve Greater Sciatic Foramen Between greater sciatic notch ilium and sacrotuberbous/sacrospinous ligaments Contents Above Piriformis: sup gluteal vessels/nerve Below Piriformis: inf gluteal/int pudendal vessels; inf gluteal, pudendal, sciatic, post fem cutaneous nerves Femur Linea aspera and intercondylar fossa post Head hyaline cartilage Neck Upwards and medially G trochanter - Glut min ant, med post, Piri sup Obturator externus/internus in troch fossa Quadratus femoris L trochanter - Psoas major/iliacus Shaft Linea aspera middle 1/3 shaft posteriorly Vastus med/lat/int, Add magnus/longus/brevis, Quadratus femoris, Short head biceps, Pectineus Medial and lateral condyles Intercondylar fossa between, Patella surf ant Medial epicondyle - TCL, medial head gastroc Lateral epicondyle - FCL, plantaris, popliteus Articulations: talus, fibula, femur at patellofemoral joint Tibia Med mall lat, sharp ant border 1 Articulations - Femoral condyles, Talus, Fibula – prox/distal Tibial plateau Tubercles of intercondylar eminence Many ant horn med meniscus Amorous ant cruciate Ladies ant horn lat meniscus Like post horn lat meniscus My post horn med meniscus P…. -
Bones of the Lower Limb Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Bones of the Lower Limb Doctors Notes Notes/Extra explanation Editing File Objectives Classify the bones of the three regions of the lower limb (thigh, leg and foot). Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula) – Bones of the foot (tarsals, metatarsals and phalanges) Recognize the side of the bone. ﻻ تنصدمون من عدد ال رشائح نصها رشح زائد وملخصات واسئلة Some pictures in the original slides have been replaced with other pictures which are more clear BUT they have the same information and labels. Terminology (Team 434) شيء مرتفع /Eminence a small projection or bump Terminology (Team 434) Bones of thigh (Femur and Patella) Femur o Articulates (joins): (1) above with Acetabulum of hip bone to form the hip joint, (2) below with tibia and patella to form the knee joint. Body of femur (shaft) o Femur consists of: I. Upper end. II. Shaft. III. Lower end. Note: All long bones consist of three things: 1- upper/proximal end posterior 2- shaft anterior 3- lower/distal end I. Upper End of Femur The upper end contains: A. Head B. Neck C. Greater trochanter & D. Lesser trochanter A. Head: o Articulates (joins) with acetabulum of hip bone to form the hip joint. o Has a depression in the center called Fovea Capitis. o The fovea capitis is for the attachment of ligament of the head of Femur. o An artery called Obturator Artery passes along this ligament to supply head of Femur. B. Neck: o Connects head to the shaft. -

Bones of Lower Limb
BONES OF LOWER LIMB ANATOMY DEPARTMENT Dr. Sanaa Alshaarawi OBJECTIVES • At the end of the lecture the students should be able to: • Classify the bones of the three regions of the lower limb (thigh, leg and foot). • Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula). – Bones of the foot (tarsals, metatarsals and phalanges) • Recognize the side of the bone BONES OF THIGH (Femur and Patella) Femur: . Articulates above with acetabulum of hip bone to form the hip joint. Articulates below with tibia and patella to form the knee joint. BONES OF THIGH (Femur and Patella) • Femur : Consists of : • Upper end • Shaft • Lower end Posterior view Anterior View UPPER END OF FEMUR • Head : • It articulates with acetabulum of hip bone to form hip joint. • Has a depression in the center (fovea capitis), for the attachment of ligament NECK of the head of femur. • Obturator artery passes along this ligament to supply head of femur. • Neck : • It connects head to the shaft. UPPER END OF FEMUR • Greater & lesser trochanters : • Anteriorly, connecting the 2 trochanters, the inter-trochanteric line, where the iliofemoral ligament is attached. • Posteriorly, the inter- trochanteric crest, on which is the quadrate tubercle (Qudratus femoris muscle). SHAFT OF FEMUR It has 3 surfaces Anterior Medial Lateral It has 3 borders Two rounded medial and lateral One thick posterior border or ridge called Anterior view Posterior view linea aspera SHAFT OF FEMUR • Anteriorly : is smooth and rounded. • Posteriorly : has a ridge, the linea aspera. • Posteriorly : below the greater trochanter is the gluteal tuberosity for attachment of gluteus M maximus muscle. -

A Fibular Notch Approach for the Treatment of Ankle Fractures Involving the Distal Tibial Plafond
A Fibular Notch Approach for the Treatment of Ankle Fractures Involving the Distal Tibial Plafond Tong Liu Department of Orthopaedics, Yantaishan Hospital Yiheng Cheng Department of Orthopaedics, Yantaishan Hospital Wenqing Qu ( [email protected] ) Department of Orthopaedics, Qilu Hospital(Qingdao) , Shandong University; 2 Department of Orthopedics,Yantaishan Hospital https://orcid.org/0000-0002-0099-1858 Research article Keywords: Ankle fractures, Pilon fractures, Distal tibial plafond fractures, Surgical approach, Fibular notch Posted Date: December 21st, 2020 DOI: https://doi.org/10.21203/rs.3.rs-129852/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on February 8th, 2021. See the published version at https://doi.org/10.1186/s13018-021-02270-3. Page 1/12 Abstract BACKGROUND: Although several approaches have been used for the treatment of complex ankle fractures, there are still some ankle fractures which can not obtain ideal intraoperative exposure with these traditional approaches. The purpose of this study was to present an innovative bular notch approach in detail for the treatment of ankle fractures involving the distal tibial plafond and to present a series of patients with either functional or radiographic outcomes. METHODS: Between March 2015 and October 2018, 22 patients with distal tibial plafond fractures with concomitant bular and distal tibiobular syndesmosis injuries were treated through a bular notch approach. The details of the surgical technique were reviewed from the operative notes. Relevant data were reviewed from the medical records. The quality of fractures and syndesmosis reduction was examined using CT scans, and lateral stability of the ankle was assessed by physical examination and stress radiographs. -
Lab Activity 9
Lab Activity 9 Appendicular Skeleton Martini Chapter 8 Portland Community College BI 231 Appendicular Skeleton • Upper & Lower extremities • Shoulder Girdle • Pelvic Girdle 2 Humerus 3 Humerus: Proximal End Greater tubercle Lesser tubercle Head: Above the epiphyseal line Anatomical Neck Surgical neck Intertubercular groove Anterior Medial Posterior4 Deltoid Tuberosity 5 Radial Groove 6 Trochlea (Distal Humerus) Anterior Posterior Anterior Posterior 7 Capitulum (Distal Humerus) Anterior Posterior Anterior Posterior 8 Olecranon Fossa (Distal Humerus) Anterior Posterior Anterior Posterior 9 Medial Epicondyle (Distal Humerus) Anterior Posterior Anterior Posterior 10 Lateral Epicondyle (Distal Humerus) Anterior Posterior Anterior Posterior 11 Radial Fossa (Distal Humerus) Anterior Posterior Anterior Posterior 12 Coronoid Fossa (Distal Humerus) Anterior Posterior Anterior Posterior 13 Lateral Supracondylar Ridge (Distal Humerus) Anterior Posterior Anterior Posterior 14 Medial Supracondylar Ridge (Distal Humerus) Anterior Posterior Anterior Posterior 15 Humerus: Distal End/Anterior Medial Lateral Supracondylar Supracondylar Ridge Ridge Coronoid Fossa Radial fossa Lateral Medial Epicondyle Epicondyle Capitulum Trochlea 16 Humerus: Distal End/Posterior Olecranon Fossa Medial Epicondyle Lateral Epicondyle Trochlea 17 Radius • “Rotates” • On the thumb side of the forearm 18 Radius: Head 19 Radial Tuberosity 20 Ulnar Notch of the Radius 21 Ulnar Notch of the Radius 22 Radius: Interosseous Ridge 23 Styloid Process of the Radius 24 Radius Distal Anterior -

Type of Article
Original Research Article The study of nutrient foramina of tibia in Marathwada region of Maharashtra R D Walwante1, S S Dhapate2*, K Thomas Manoj3 1,3Assistant Professor, 2Professor and HOD, Department of Anatomy, SRTRGMC, Ambajogai, Dist. Beed, INDIA. Email: [email protected] Abstract Background: Nutrient foramen is a natural opening into the shaft of a bone, allowing for passage of blood vessels into the medullary cavity. This study aims to determine the number, location and direction of nutrient foramina of tibia. Material and methods: 185 dry tibia from government medical colleges from Marathwada region were examined for nutrient foramina location number direction and its relation to the other bony land marks. Results: Single nutrient foramina directed downwards was the rule. The location of nutrient foramina closely resembled with the data of previous similar studies done in other part of world. Conclusion: The present study generated database for nutrient foramen of tibia from Marathwada area. This can be utilized by surgeon to preserve nutrient artery during operation for fracture repair, tumor and bone grafts involving tibia. Key words: Tibia, Nutrient artery, Nutrient foramen, Fracture repairs. *Address for Correspondence: Dr.S S Dhapate, Professor and HOD, Department of Anatomy Department, SRTRGMC, Ambajogai, Dist. Beed, INDIA. Email: [email protected] Received Date: 02/04/2019 Revised Date: 23/05/2019 Accepted Date: 01/07/2019 DOI: https://doi.org/10.26611/10011116 twice as fast as the other end. As a characteristic, the Access this article online nutrient vessels move away from the growing end in the 4 bone .The nutrient artery to the tibia is a branch of Quick Response Code: Website: posterior tibial artery or peroneal artery. -
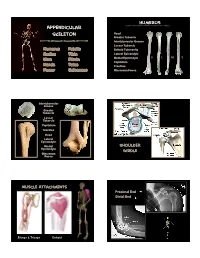
Appendicular Skeleton
Humerus Appendicular Skeleton Head Greater Tubercle Intertubercular Groove Lesser Tubercle Humerus Patella Deltoid Tuberosity Radius Tibia Lateral Epicondyle D L M V Ulna Fibula Medial Epicondyle Capitulum Hands Talus Trochlea Femur Calcaneus Olecrenon Fossa Intertubercular Groove Greater Tubercle Lesser Tubercle Capitulum Trochlea Head Lateral Epicondyle Medial Shoulder Epicondyle Girdle Olecrenon Fossa Muscle Attachments Proximal End Distal End Biceps & Triceps Deltoid 1 Radius Ulna Head Neck Radial Tuberosity Interosseous Crest Styloid Process Olecrenon Process Ulnar Notch Radial Notch Tuberosity L M D V Styloid Process D L M V Interosseous Crest Trochlea Radial Tuberosity Olecrenon Process Capitulum Head Medial Epicondyle Phalanges 1st 3rd Proximal Phalange 3rd Metacarpals 1st Proximal Phalange 2 Femur Head, medial Larger epicondyle, lateral Femur head Olecrenon fossa, distal Fovea capitus Olecrenon process, proximal Greater trochanter Radial notch, lateral Lesser trochanter Styloid process, towards ‘pinky’ Linea aspera Head, proximal Medial condyle Tuberosity, medial Lateral condyle Styloid towards thumb Intercondylar fossa V D L M Patellar articular surface Proximal Femur Fovea capitus Trochanteric Fossa Greater Trochanter Lesser femur humerus Trochanter Proximal Femur Medial condyle Lateral condyle Patella Patellar articular surface Intercondylar notch V D Apex Base Facet for lateral femoral condyle Distal Femur Facet for medial femoral condyle 3 Tibia Tibia Lateral condyle Lateral condyle Medial condyle Medial condyle Fibular -
Lab Manual Appendicular Skele
1 PRE-LAB EXERCISES When studying the skeletal system, the bones are often sorted into two broad categories: the axial skeleton and the appendicular skeleton. This lab focuses on the appendicular skeleton, which is formed from the pectoral and pelvic girdles and the upper and lower limbs. View Module 7.2 Axial and Appendicular Skeleton to highlight the bones of the appendicular skeleton and compare them to those of the axial skeleton. Examine Module 11.1 Appendicular Skeleton to view only the bones of the appendicular skeleton. In addition to learning about all the bones of the appendicular skeleton, it is also important to identify some significant bone markings. Bone markings can have many shapes, including holes, round or sharp projections, and shallow or deep valleys, among others. These markings on the bones serve many purposes, including forming attachments to other bones or muscles and allowing passage of a blood vessel or nerve. It is helpful to understand the meanings of some of the more common bone marking terms. Before we get started, look up the definitions of these common bone marking terms: Canal: Condyle: Facet: Fissure: Foramen: (see Module 10.18 Foramina of Skull) Fossa: Margin: Process: Proximal: Trochanter: Tubercle: Tuberosity: Throughout this exercise, you will notice bold terms. This is meant to focus your attention on these important words. Make sure you pay attention to any bold words and know how to explain their definitions and/or where they are located. Use the following modules to guide your exploration of the appendicular skeleton. As you explore these bones in Visible Body’s app, also locate the bones and bone markings on any available charts, models, or specimens. -

Study of Distal Dimensions of Tibia in Correlation with The
International Journal of Anatomy and Research, Int J Anat Res 2018, Vol 6(2.3):5354-59. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2018.206 STUDY OF DISTAL DIMENSIONS OF TIBIA IN CORRELATION WITH THE LENGTH OF TIBIA Yogi Anupkumar Balakrishnan 1, S.Vikram *2, Chitra Prakash Rao 3, Sanjay Kumar B Revankar 4. 1 Assistant professor of Anatomy Malankara orthodox syrian church medical college, kolenchery Kerala, India. *2 Associate Professor of Anatomy A.J Institute of Medical Sciences and Research centre, Mangalore,India. 3 Professor and HOD of Anatomy A.J Institute of Medical Sciences and Research centre, Mangalore, India. 4 Assistant professor of Anatomy, A.J Institute of Medical Sciences and Research centre, Mangalore, India. ABSTRACT Background: In forensic analysis, the estimation of the stature is key in identification of an individual. The stature of an individual can be estimated from long bones especially the tibia and the femur as these have direct correlation to the height of an individual. The tibia is ideal in this application as it resists erosion and keeps its anatomical shape for long even after burial. Mechanical loading is especially high in the distal ends of long bones of the lower limb and as such they display significant inter-individual differences. The use of distal dimensions in estimation of the length of the tibia from skeletal remains has not been reported. Materials and methods: 150 dry and processed tibias irrespective of side, grossly normal and complete were randomly collected from a medical college of south India.