Back of Leg I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study of Variation of Great Saphenous Veins and Its Surgical Significance (Original Study)
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 17, Issue 2 Ver. 10 February. (2018), PP 21-26 www.iosrjournals.org Study of Variation of Great Saphenous Veins and Its Surgical Significance (Original Study) Dr Surekha W. Meshram1, Dr. Yogesh Ganorkar2, Dr V.P. Rukhmode3, Dr. Tarkeshwar Golghate4 1(M.B.B.S,M.D) Associate Professor, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 2(M.B.B.S,M.D) Assistant Professor, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 3 (M.B.B.S, M.S) Professor and Head, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 4(M.B.B.S, M.D) Assiciate Professor, Dept. of Anatomy Govt. Medical College, Nagpur, Maharashtra Corresponding Author: Dr. Surekha W. Meshram Abstract Introduction: Veins of lower limbs are more involves for various venous disorders as compare to upper limbs. Most common venous disorders occurring in lower limbs are varicose veins, deep venous thrombosis and venous ulcers. Varicose veins are found in large population of world affecting both the males and females. Surgical operations are performed in all over the world to cure it. In the varicose vein surgery, surgeon successfully do the ligation as well as stripping of the great saphenous vein and its tributaries. Duplication of a great saphenous vein can be a potential cause for recurrent varicose veins after surgery as well as complications may occur during the surgery. Method: The present study was done by dissection method on 50 lower limbs of cadavers. Its aim was to identify the incidence and pattern of duplication of long saphenous vein in Indian population. -

Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’S Collin G
Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’s Collin G. Messerly DPM, Keegan A. Duelfer DPM, Troy J. Boffeli DPM, FACFAS, Tyler K. Sorensen, DPM Regions Hospital / HealthPartners Institute for Education and Research - Saint Paul, MN Figure 1. Zone of Dense Bone in Medial Malleolar ORIF Figure 4. Measuring Distal – Most 5% to Medial Malleolus Table 2. Distance Between Epiphyseal Scar & Distal – Most 5% of RESULTS STATEMENT OF PURPOSE The epiphyseal scar is located in the distal The medial malleolus to distal – most 5% mark Tibia 97 WB ankle CT scans evaluated in uninjured ankles Medial malleolar fractures are one of the most common fracture types metaphysis of the tibia, and can oftentimes be was measured on the coronal WB CT slice with Measurement of interest Male: Mean ± SD Female: Mean ± SD (mm) In males < 60 years old there was a 12.75 mm zone of increased bone the widest medial malleolus. Screw threads observed in the ankle joint and have been long fixated with two screws; easily visualized on X-ray and CT scan (red line). (mm) density, as compared to 13.66 mm in those ≥ 60 which was not statistically The distal – most 5% of the tibia (distal to the beyond this point will purchase less dense bone however, the bone density of the distal tibia has potential for poor screw significant. purchase due to compromised bone density. This is especially true in elderly black line) contains dense bone with marked in the medullary canal with potential to not have Epiphyseal Scar to Medial Malleolus 12.75 ± 2.91 9.39 ± 2.38 In females < 60 years old there was 9.39 mm zone of increased bone populations with osteoporotic bone. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -

Peroneal Nerve Injury Associated with Sports-Related Knee Injury
Neurosurg Focus 31 (5):E11, 2011 Peroneal nerve injury associated with sports-related knee injury DOSANG CHO, M.D., PH.D.,1 KRIANGSAK SAETIA, M.D.,2 SANGKOOK LEE, M.D.,4 DAVID G. KLINE, M.D.,3 AND DANIEL H. KIM, M.D.4 1Department of Neurosurgery, School of Medicine, Ewha Womans University, Seoul, Korea; 2Division of Neurosurgery, Department of Surgery, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 3Department of Neurosurgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana; and 4Department of Neurosurgery, Baylor College of Medicine, Houston, Texas Object. This study analyzes 84 cases of peroneal nerve injuries associated with sports-related knee injuries and their surgical outcome and management. Methods. The authors retrospectively reviewed the cases of peroneal nerve injury associated with sports between the years 1970 and 2010. Each patient was evaluated for injury mechanism, preoperative neurological status, electro- physiological studies, lesion type, and operative technique (neurolysis and graft repair). Preoperative status of injury was evaluated by using a grading system published by the senior authors. All lesions in continuity had intraoperative nerve action potential recordings. Results. Eighty-four (approximately 18%) of 448 cases of peroneal nerve injury were found to be sports related, which included skiing (42 cases), football (23 cases), soccer (8 cases), basketball (6 cases), ice hockey (2 cases), track (2 cases) and volleyball (1 case). Of these 84 cases, 48 were identified as not having fracture/dislocation and 36 cases were identified with fracture/dislocation for surgical interventions. Good functional outcomes from graft repair of graft length < 6 cm (70%) and neurolysis (85%) in low-intensity peroneal nerve injuries associated with sports were obtained. -

Posterior Compartment Of
POSTERIOR COMPARTMENT OF LEG Cross Section of Leg Cutaneous Innervation Superficial vessels of leg Deep Fascia of Posterior Compartment Boundaries and Sub-divisions Flexor Retinaculum Muscles of Posterior Compartment I. Superficial Muscles a) Gastrocnemius b) Soleus c) Plantaris a) Gastrocnemius Origin:- by 2 heads i. Lateral head- lateral aspect of lateral condyle of femur ii. Medial head- popliteal surface of femur above medial condyle Insertion:- Posterior surface of calcaneum as Tendo-calcaneus b) Soleus Origin:- i. Inverted ‘V’ shaped from soleal line on tibia ii. Upper 1/4th of upper surface of shaft of fibula iii. Fibrous arch between these 2 bones Insertion:- Posterior surface of calcaneum as Tendo-calcaneus c) Plantaris- fusiform belly Origin:- Lateral supracondylar ridge of femur Insertion:- Posterior surface of calcaneum medial to Tendo- calcaneus Superficial Strata Deep Strata I. Deep Muscles a) Popliteus b) Flexor Digitorum Longus c) Flexor Hallucis Longus d) Tibialis Posterior a) Popliteus Origin:- Groove on lateral surface of lat. femoral condyle Insertion:- Triangular area on posterior surface of tibia b) Flexor Digitorum Longus Origin:- i. Upper 2/3rds of medial part of post. surface of tibia ii. Fascia covering tibialis posterior Insertion:- Plantar surface of base of distal phalanx of lateral 4 toes a) Flexor Hallucis Longus Origin:- i. Lower 3/4th of post. surface of fibula ii. Interosseous membrane Insertion:- Plantar surface of base of distal phalanx of great toe a) Tibialis Posterior Origin:- i. Upper 2/3rds of lat. Part of posterior surface of tibia ii. Post. Surface of fibula and interosseous membrane Insertion:- Tuberosity of navicular bone Posterior Tibial Artery • Larger terminal branch of Popliteal artery • Branches:- a. -

Compression Garments for Leg Lymphoedema
Compression garments for leg lymphoedema You have been fitted with a compression garment to help reduce the lymphoedema in your leg. Compression stockings work by limiting the amount of fluid building up in your leg. They provide firm support, enabling the muscles to pump fluid away more effectively. They provide most pressure at the foot and less at the top of the leg so fluid is pushed out of the limb where it will drain away more easily. How do I wear it? • Wear your garment every day to control the swelling in your leg. • Put your garment on as soon as possible after getting up in the morning. This is because as soon as you stand up and start to move around extra fluid goes into your leg and it begins to swell. • Take the garment off before bedtime unless otherwise instructed by your therapist. We appreciate that in hot weather garments can be uncomfortable, but unfortunately this is when it is important to wear it as the heat can increase the swelling. If you would like to leave off your garment for a special occasion please ask the clinic for advice. What should I look out for? Your garment should feel firm but not uncomfortable: • If you notice the garment is rubbing or cutting in, adjust the garment or remove it and reapply it. • If your garment feels tight during the day, try and think about what may have caused this. If you have been busy, sit down and elevate your leg and rest for at least 30 minutes. -
LECTURE (SACRAL PLEXUS, SCIATIC NERVE and FEMORAL NERVE) Done By: Manar Al-Eid Reviewed By: Abdullah Alanazi
CNS-432 LECTURE (SACRAL PLEXUS, SCIATIC NERVE AND FEMORAL NERVE) Done by: Manar Al-Eid Reviewed by: Abdullah Alanazi If there is any mistake please feel free to contact us: [email protected] Both - Black Male Notes - BLUE Female Notes - GREEN Explanation and additional notes - ORANGE Very Important note - Red CNS-432 Objectives: By the end of the lecture, students should be able to: . Describe the formation of sacral plexus (site & root value). List the main branches of sacral plexus. Describe the course of the femoral & the sciatic nerves . List the motor and sensory distribution of femoral & sciatic nerves. Describe the effects of lesion of the femoral & the sciatic nerves (motor & sensory). CNS-432 The Mind Maps Lumber Plexus 1 Branches Iliohypogastric - obturator ilioinguinal Femoral Cutaneous branches Muscular branches to abdomen and lower limb 2 Sacral Plexus Branches Pudendal nerve. Pelvic Splanchnic Sciatic nerve (largest nerves nerve), divides into: Tibial and divides Fibular and divides into : into: Medial and lateral Deep peroneal Superficial planter nerves . peroneal CNS-432 Remember !! gastrocnemius Planter flexion – knee flexion. soleus Planter flexion Iliacus –sartorius- pectineus – Hip flexion psoas major Quadriceps femoris Knee extension Hamstring muscles Knee flexion and hip extension gracilis Hip flexion and aids in knee flexion *popliteal fossa structures (superficial to deep): 1-tibial nerve 2-popliteal vein 3-popliteal artery. *foot drop : planter flexed position Common peroneal nerve injury leads to Equinovarus Tibial nerve injury leads to Calcaneovalgus CNS-432 Lumbar Plexus Formation Ventral (anterior) rami of the upper 4 lumbar spinal nerves (L1,2,3 and L4). Site Within the substance of the psoas major muscle. -

Vena Saphena Magna – Peculiarities of Origin, Trajectory and Drainage *Anastasia Bendelic, Ilia Catereniuc
A. Bendelic et al. Moldovan Medical Journal. September 2020;63(3):26-31 ORIGINAL RESEarCH DOI: 10.5281/zenodo.3958531 UDC: 611.147.33 Vena saphena magna – peculiarities of origin, trajectory and drainage *Anastasia Bendelic, Ilia Catereniuc Department of Anatomy and Clinical Anatomy Nicolae Testemitanu State University of Medicine and Pharmacy, Chisinau, the Republic of Moldova Authors’ ORCID iDs, academic degrees and contributions are available at the end of the article *Corresponding author: [email protected] Manuscript received July 25, 2020; revised manuscript August 14, 2020; published online August 26, 2020 Abstract Background: Vena saphena magna (VSM) – one of the two superficial venous collectors of the lower limb, the longest vein of the human body, is often accompanied by parallel veins, of which clinical significance may be different. The objective of the study was to investigate the individual anatomical variability of the VSM, on macroscopic aspect, in cadavers, of which variability is important for the vascular surgeon and / or for the cardiac surgeon. Material and methods: This study was conducted on 22 formolized lower limbs using classical dissection methods. The observed anatomical variants were recorded and photographed. Results: The dorsal venous arch of the foot, the origin of the VSM, was double in 2 cases (9.1%), and it was absent in one case (4.55%), thus two dorsal metatarsal veins continued proximally with two medial marginal veins. In the leg, VSM was double in one case (4.55%), and in other 14 cases (63.63%) it was accompanied by accessory saphenous veins. In the thigh, it was double in 3 cases (13.6%), and in 10 cases (45.5%) it was accompanied by accessory saphenous veins. -

Sports Ankle Injuries Assessment and Management
FOCUS Sports injuries Sports ankle injuries Drew Slimmon Peter Brukner Assessment and management Background Case study Lucia is a female, 16 years of age, who plays netball with the Sports ankle injuries present commonly in the general state under 17s netball team. She presents with an ankle injury practice setting. The majority of these injuries are inversion sustained at training the previous night. She is on crutches and plantar flexion injuries that result in damage to the and is nonweight bearing. Examination raises the possibility of lateral ligament complex. a fracture, but X-ray is negative. You diagnose a severe lateral Objective ligament sprain and manage Lucia with ice, a compression The aim of this article is to review the assessment and bandage and a backslab initially. She then progresses through management of sports ankle injuries in the general practice a 6 week rehabilitation program and you recommend she wear setting. an ankle brace for at least 6 months. Discussion Assessment of an ankle injury begins with a detailed history to determine the severity, mechanism and velocity of the injury, what happened immediately after and whether there is a past history of inadequately rehabilitated ankle injury. Examination involves assessment of weight bearing, inspection, palpation, movement, and application of special examination tests. Plain X-rays may be helpful to exclude a fracture. If the diagnosis is uncertain, consider second The majority of ankle injuries are inversion and plantar line investigations including bone scan, computerised flexion injuries that result in damage to the lateral tomography or magnetic resonance imaging, and referral to a ligament complex (Figure 1). -
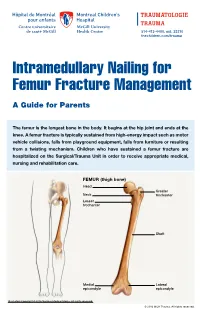
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

ANTERIOR KNEE PAIN Home Exercises
ANTERIOR KNEE PAIN Home Exercises Anterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including: • Weak or overused muscles • Chondromalacia of the patella (softening and breakdown of the cartilage on the underside of the kneecap) • Inflammations and tendon injury (bursitis, tendonitis) • Loose ligaments with instability of the kneecap • Articular cartilage damage (chondromalacia patella) • Swelling due to fluid buildup in the knee joint • An overload of the extensor mechanism of the knee with or without malalignment of the patella You may feel pain after exercising or when you sit too long. The pain may be a nagging ache or an occasional sharp twinge. Because the pain is around the front of your knee, treatment has traditionally focused on the knee itself and may include taping or bracing the kneecap, or patel- la, and/ or strengthening the thigh muscle—the quadriceps—that helps control your kneecap to improve the contact area between the kneecap and the thigh bone, or femur, beneath it. Howev- er, recent evidence suggests that strengthening your hip and core muscles can also help. The control of your knee from side to side comes from the glutes and core control; that is why those areas are so important in management of anterior knee pain. The exercises below will work on a combination of flexibility and strength of your knee, hip, and core. Although some soreness with exercise is expected, we do not want any sharp pain–pain that gets worse with each rep of an exercise or any increased soreness for more than 24 hours.