Diagnosis of Iliac Vein Obstruction with Duplex Ultrasound
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prep for Practical II
Images for Practical II BSC 2086L "Endocrine" A A B C A. Hypothalamus B. Pineal Gland (Body) C. Pituitary Gland "Endocrine" 1.Thyroid 2.Adrenal Gland 3.Pancreas "The Pancreas" "The Adrenal Glands" "The Ovary" "The Testes" Erythrocyte Neutrophil Eosinophil Basophil Lymphocyte Monocyte Platelet Figure 29-3 Photomicrograph of a human blood smear stained with Wright’s stain (765). Eosinophil Lymphocyte Monocyte Platelets Neutrophils Erythrocytes "Blood Typing" "Heart Coronal" 1.Right Atrium 3 4 2.Superior Vena Cava 5 2 3.Aortic Arch 6 4.Pulmonary Trunk 1 5.Left Atrium 12 9 6.Bicuspid Valve 10 7.Interventricular Septum 11 8.Apex of The Heart 9. Chordae tendineae 10.Papillary Muscle 7 11.Tricuspid Valve 12. Fossa Ovalis "Heart Coronal Section" Coronal Section of the Heart to show valves 1. Bicuspid 2. Pulmonary Semilunar 3. Tricuspid 4. Aortic Semilunar 5. Left Ventricle 6. Right Ventricle "Heart Coronal" 1.Pulmonary trunk 2.Right Atrium 3.Tricuspid Valve 4.Pulmonary Semilunar Valve 5.Myocardium 6.Interventricular Septum 7.Trabeculae Carneae 8.Papillary Muscle 9.Chordae Tendineae 10.Bicuspid Valve "Heart Anterior" 1. Brachiocephalic Artery 2. Left Common Carotid Artery 3. Ligamentum Arteriosum 4. Left Coronary Artery 5. Circumflex Artery 6. Great Cardiac Vein 7. Myocardium 8. Apex of The Heart 9. Pericardium (Visceral) 10. Right Coronary Artery 11. Auricle of Right Atrium 12. Pulmonary Trunk 13. Superior Vena Cava 14. Aortic Arch 15. Brachiocephalic vein "Heart Posterolateral" 1. Left Brachiocephalic vein 2. Right Brachiocephalic vein 3. Brachiocephalic Artery 4. Left Common Carotid Artery 5. Left Subclavian Artery 6. Aortic Arch 7. -

Corona Mortis: the Abnormal Obturator Vessels in Filipino Cadavers
ORIGINAL ARTICLE Corona Mortis: the Abnormal Obturator Vessels in Filipino Cadavers Imelda A. Luna Department of Anatomy, College of Medicine, University of the Philippines Manila ABSTRACT Objectives. This is a descriptive study to determine the origin of abnormal obturator arteries, the drainage of abnormal obturator veins, and if any anastomoses exist between these abnormal vessels in Filipino cadavers. Methods. A total of 54 cadaver halves, 50 dissected by UP medical students and 4 by UP Dentistry students were included in this survey. Results. Results showed the abnormal obturator arteries arising from the inferior epigastric arteries in 7 halves (12.96%) and the abnormal communicating veins draining into the inferior epigastric or external iliac veins in 16 (29.62%). There were also arterial anastomoses in 5 (9.25%) with the inferior epigastric artery, and venous anastomoses in 16 (29.62%) with the inferior epigastric or external iliac veins. Bilateral abnormalities were noted in a total 6 cadavers, 3 with both arterial and venous, and the remaining 3 with only venous anastomoses. Conclusion. It is important to be aware of the presence of these abnormalities that if found during surgery, must first be ligated to avoid intraoperative bleeding complications. Key Words: obturator vessels, abnormal, corona mortis INtroDUCTION The main artery to the pelvic region is the internal iliac artery (IIA) with two exceptions: the ovarian/testicular artery arises directly from the aorta and the superior rectal artery from the inferior mesenteric artery (IMA). The internal iliac or hypogastric artery is one of the most variable arterial systems of the human body, its parietal branches, particularly the obturator artery (OBA) accounts for most of its variability. -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Cat Dissection
Cat Dissection Muscular Labs Tibialis anterior External oblique Pectroalis minor Sartorius Gastrocnemius Pectoralis major Levator scapula External oblique Trapezius Gastrocnemius Semitendinosis Trapezius Latissimus dorsi Sartorius Gluteal muscles Biceps femoris Deltoid Trapezius Deltoid Lumbodorsal fascia Sternohyoid Sternomastoid Pectoralis minor Pectoralis major Rectus abdominis Transverse abdominis External oblique External oblique (reflected) Internal oblique Lumbodorsal Deltoid fascia Latissimus dorsi Trapezius Trapezius Trapezius Deltoid Levator scapula Deltoid Trapezius Trapezius Trapezius Latissimus dorsi Flexor carpi radialis Brachioradialis Extensor carpi radialis Flexor carpi ulnaris Biceps brachii Triceps brachii Biceps brachii Flexor carpi radialis Flexor carpi ulnaris Extensor carpi ulnaris Triceps brachii Extensor carpi radialis longus Triceps brachii Deltoid Deltoid Deltoid Trapezius Sartorius Adductor longus Adductor femoris Semimembranosus Vastus Tensor fasciae latae medialis Rectus femoris Vastus lateralis Tibialis anterior Gastrocnemius Flexor digitorum longus Biceps femoris Tensor fasciae latae Semimembranosus Semitendinosus Gluteus medius Gluteus maximus Extensor digitorum longus Gastrocnemius Soleus Fibularis muscles Brachioradiallis Triceps (lateral and long heads) Brachioradialis Biceps brachii Triceps (medial head) Trapezius Deltoid Deltoid Levator scapula Trapezius Deltoid Trapezius Latissimus dorsi External oblique (right side cut and reflected) Rectus abdominis Transversus abdominis Internal oblique Pectoralis -
Nervous and Vascular System
NO. A100 KEY CHART FOR MODEL NERVOUS AND VASCULAR SYSTEM 神経系・循環系・門脈系 模型 MADE IN JAPAN KEY CHART FOR MODEL NO. A100 NERVOUS AND VASCULAR SYSTEM 神経系・循環系・門脈系模型 White labels BRAIN ENCEPHALON 脳 A.Frontal lobe of cerebrum A. Lobus frontalis A. 前頭葉 1. Marginal gyrus 1. Gyrus frontalis superior 1. 上前頭回 2. Middle frontal gyrus 2. Gyrus frontalis medius 2. 中前頭回 3. Inferior frontal gyrus 3. Gyrus frontalis inferior 3. 下前頭回 4. Precentral gyru 4. Gyrus precentralis 4. 中心前回 B. Parietal lobe of cerebrum B. Lobus parietalis B. 全頂葉 5. Postcentral gyrus 5. Gyrus postcentralis 5. 中心後回 6. Superior parietal lobule 6. Lobulus parietalis superior 6. 上頭頂小葉 7. Inferior parietal lobule 7. Lobulus parietalis inferior 7. 下頭頂小葉 C.Occipital lobe of cerebrum C. Lobus occipitalis C. 後頭葉 D. Temporal lobe D. Lobus temporalis D. 側頭葉 8. Superior temporal gyrus 8. Gyrus temporalis superior 8. 上側頭回 9. Middle temporal gyrus 9. Gyrus temporalis medius 9. 中側頭回 10. Inferior temporal gyrus 10. Gyrus temporalis inferior 10. 下側頭回 11. Lateral sulcus 11. Sulcus lateralis 11. 外側溝(外側大脳裂) E. Cerebellum E. Cerebellum E. 小脳 12. Biventer lobule 12. Lobulus biventer 12. 二腹小葉 13. Superior semilunar lobule 13. Lobulus semilunaris superior 13. 上半月小葉 14. Inferior lobulus semilunaris 14. Lobulus semilunaris inferior 14. 下半月小葉 15. Tonsil of cerebellum 15. Tonsilla cerebelli 15. 小脳扁桃 16. Floccule 16. Flocculus 16. 片葉 F.Pons F. Pons F. 橋 G.Medullary G. Medulla oblongata G. 延髄 SPINAL CORD MEDULLA SPINALIS 脊髄 H. Cervical enlargement H.Intumescentia cervicalis H. 頸膨大 I.Lumbosacral enlargement I. Intumescentia lumbalis I. 腰膨大 J.Cauda equina J. -

Surgical Anatomy of the Common Iliac Veins During Para-Aortic and Pelvic Lymphadenectomy for Gynecologic Cancer
Original Article J Gynecol Oncol Vol. 25, No. 1:64-69 http://dx.doi.org/10.3802/jgo.2014.25.1.64 pISSN 2005-0380·eISSN 2005-0399 Surgical anatomy of the common iliac veins during para-aortic and pelvic lymphadenectomy for gynecologic cancer Kazuyoshi Kato, Shinichi Tate, Kyoko Nishikimi, Makio Shozu Department of Gynecology, Chiba University School of Medicine, Chiba, Japan See accompanying editorial by Lee on page 1. Objective: Compression of the left common iliac vein between the right common iliac artery and the vertebrae is known to be associated with the occurrence of left iliofemoral deep vein thrombosis (DVT). In this study, we described the variability in vascular anatomy of the common iliac veins and evaluated the relationship between the degree of iliac vein compression and the presence of DVT using the data from surgeries for gynecologic cancer. Methods: The anatomical variations and the degrees of iliac vein compression were determined in 119 patients who underwent systematic para-aortic and pelvic lymphadenectomy during surgery for primary gynecologic cancer. Their medical records were reviewed with respect to patient-, disease-, and surgery-related data. Results: The degrees of common iliac vein compression were classified into three grades: grade A (n=28, 23.5%), with a calculated percentage of 0%-25% compression; grade B (n=47, 39.5%), with a calculated percentage of 26%-50% compression; and grade C (n=44, 37%), with a calculated percentage of more than 50% compression. Seven patients (5.9%) had common iliac veins with anomalous anatomies; three were divided into small caliber vessels, two with a flattened structure, and two had double inferior vena cavae. -

Co-Existence of the Double Inferior Vena Cava with Complex Interiliac
Folia Morphol. Vol. 77, No. 1, pp. 151–155 DOI: 10.5603/FM.a2017.0074 C A S E R E P O R T Copyright © 2018 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Co-existence of the double inferior vena cava with complex interiliac venous communication and aberrant common hepatic artery arising from superior mesenteric artery: a case report V. Chentanez, N. Nateniyom, T. Huanmanop, S. Agthong Department of Anatomy, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand [Received: 19 June 2017; Accepted: 31 July 2017] Variations of the arterial and venous system of the abdomen and pelvis have im- portant clinical significance in hepatobiliary surgery, abdominal laparoscopy, and radiological intervention. A case of double inferior vena cava (IVC) with complex interiliac communication and variation of the common hepatic artery (CHA) arising from superior mesenteric artery (SMA) in a 79-year-old male cadaver is presented. Both IVCs ascended on either side of the abdominal aorta. The left-sided IVC crossed anterior to the aorta at the level of the left renal vein. The union of both IVCs was at the level just above the right renal vein. The diameter of right-sided IVC, left-sided IVC and the common IVC were 16.73 mm, 21.57 mm and 28.75 mm, respectively. In the pelvic cavity, the right common iliac vein was formed by a union of right external and internal iliac veins while the formation of left common iliac vein was from the external iliac vein and two internal iliac veins. An interiliac vein ran from right internal iliac vein to left common iliac vein with an additional communicating vein running from the middle of this interiliac vein to the right common iliac vein. -

Pelvic Venous Disorders
PELVIC VENOUS DISORDERS Anatomy and Pathophysiology Two Abdomino-Pelvic Compression Syndromes DIAGNOSIS of ABDOMINOO-PELVICP z Nutcracker Syndrome 9 Compression of the left renal vein COMPRESSIONCO SS O SYNDROMES S O with venous congestion of the left (with Emphasis on Duplex Ultrasound) kidney and left ovarian vein reflux R. Eugene Zierler, M.D. z May-Thurner Syndrome 9 Compression of the left common iliac vein by the right common The DD.. EE.. StrandnessStrandness,, JrJr.. Vascular Laboratory iliac artery with left lower University of Washington Medical Center extremity venous stasis and left DivisionDivision of Vascular Surgery internal iliac vein reflux University of Washington, School of Medicine ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome Left Renal Vein Entrapment z Grant 1937: Anatomical observation “…the left renal vein, as it lies between the aorta and superior mesenteric artery, resembles a nut between the jaws of a nutcracker.” X z El-Sadr 1950: Described first patient with the clinical syndrome X z De Shepper 1972: Named the disorder “Nutcracker Syndrome” Copy Here z Nutcracker Phenomenon z Nutcracker Syndrome 9 Anatomic finding only 9 Hematuria, proteinuria 9 Compression of left renal 9 Flank pain vein - medial narrowing 9 Pelvic pain/congestion with lateral (hilar) dilation 9 Varicocele ABDOMINO-PELVIC COMPRESSION ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome - Diagnosis Nutcracker Syndrome z Anterior Nutcracker z Posterior Nutcracker z Evaluate the left renal vein for aorto-mesenteric compression 9 Compression between -

Download Download
EJMED, European Journal of Medical and Health Sciences Vol. 2, No. 4, July 2020 Nonseminomatous Germ Cell Testicular Tumour With Metastatic Retroperitoneal Lymphadenopathy Presenting As Severe Backache Due To Ivc Thrombosis Sanjay M. Khaladkar, Rubab Kaur Sekhon, Khushboo Agrawal, Vikas LB Jadhav, and Rajesh S. Kuber Abstract — IVC thrombosis is often under-recognized. I. CASE REPORT Malignancy can cause spontaneous IVC thrombosis due to its A 26 years old male patient presented with lower back prothrombotic potential. Malignant tumors can compress, adhere or infiltrate the IVC wall causing endothelial damage ache, weight loss and fever. MRI Lumbosacral spine (Fig. 1) with subsequent thrombosis. Retroperitoneal done in an outside center showed a soft tissue signal lymphadenopathy can cause compressive distortion of IVC intensity retroperitoneal mass in aorto-caval region causing venous stasis and turbulent flow. Metastatic compressing IVC- likely lymph nodal mass. retroperitoneal lymphadenopathy from testicular tumor is a rare cause of IVC invasion with resultant IVC thrombosis which can rarely present as backache. High index of suspicion is needed to detect primary testicular tumor in cases of IVC thrombosis, especially in young individuals. A 26 -year old male presented with lower back ache, weight loss and fever. MRI Lumbosacral spine done outside showed a soft tissue signal intensity retroperitoneal mass in aortocaval region compressing IVC. Ultrasound (done outside) revealed mild right sided hydroureteronephrosis secondary to a lobulated heterogeneous mass in inter-aortocaval region encasing right ureter and invading IVC causing thrombosis. Contrast enhanced Computerized axial tomography of abdomen showed a heterogeneously enhancing lobulated mass with multiple internal calcifications, in inter-aortocaval region at L3-4 level invading the IVC causing IVC thrombosis. -
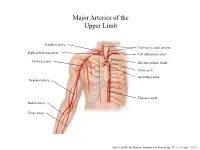
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

A Ureteral Mass Presenting As Deep Vein Thrombosis: a Very Rare Presentation
Urology & Nephrology Open Access Journal Case Report Open Access A ureteral mass presenting as deep vein thrombosis: a very rare presentation Abstract Volume 6 Issue 3 - 2018 Venous Thromboembolism is a dreaded condition. Many conditions and systemic Dushiant Sharma, Umesh Sharma, Sumit diseases are known to predispose to its occurrence including malignancy, pancreatitis, burns, clotting disorders and direct compression. All of these have been known to affect Gehlawat Department of Urology, RML Hospital & PGIMER, Delhi, India one or more factors in Virchows Triad proposed roughly a century ago.1 It consists of Hypercoagulability, Vascular Endothelial Dysfunction, Stasis. Stasis, one of the factors in Correspondence: Dushiant Sharma, Department of Urology, Virchows triad has been studied to a very small extent and it is this feature that is mostly Dr RML Hospital & PGIMER, Baba Khadak Singh Marg, New responsible for the development of Deep Vein Thrombosis (DVT) due to direct compression. Delhi, 110001, Tel 011-2340-4323, Email [email protected] Iliofemoral thrombosis in malignancy patients can be caused due to vein compression by pelvic malignancy and usually presents as unilateral lower limb swelling. In patients with Received: November 15, 2018 | Published: June 22, 2018 sudden onset of unilateral lower limb swelling without any perceived or diagnosed medical condition, detailed evaluation may lead to early identification, appropriate management and possibly cure. We present a case of acute unilateral ilio-femoral DVT caused by external compression by a mid-ureteric mass. Keywords: deep vein thrombosis, ileofemoral thrombosis, ureteric malignancy, upper tract urothelial cancers Abbreviations: DVT, Deep Vein Thrombosis; VTE, Venous Nephrouretectomy with bladder cuff excision was planned. -

How to Assess a CTA of the Abdomen to Plan an Autologous Breast Reconstruction
296 Visualized Surgery How to assess a CTA of the abdomen to plan an autologous breast reconstruction Warren M. Rozen1,2, Harmeet K. Bhullar2, David Hunter-Smith1,2 1Department of Plastic and Reconstructive Surgery, Peninsula Health, Frankston, Victoria, Australia; 2Peninsula Clinical School, Central Clinical School Faculty of Medicine, Monash University, Frankston, Victoria, Australia Correspondence to: Prof. Warren M. Rozen. Department of Plastic and Reconstructive Surgery, Frankston Hospital, Peninsula Health, 2 Hastings Road, Frankston, Victoria 3199, Australia. Email: [email protected]. Abstract: The deep inferior epigastric perforator (DIEP) flap is recognised as the most popular option for autologous breast reconstruction. Planning of the DIEP flap involves pre-operative assessment of abdominal vascular anatomy with imaging, of which computed tomographic angiography (CTA) has become the mainstay. CTA enables detailed planning of a range of surgical steps, leading to reduced operative times and improved surgical outcomes. The value of CTA is only demonstrated when the relevant vascular anatomy is able to be demonstrated and appraised. For optimal analysis, a 64-slice multi-detector row CT scanner and imaging software including OsiriX™, Siemens InSpace™ or Horos™ are required. The seven major steps to consider include: (I) perforator size; (II) perforator angiosome; (III) intramuscular course; (IV) deep inferior epigastric artery (DIEA) pedicle; (V) venous anatomy; (VI) superficial inferior epigastric artery (SIEA) and superficial inferior epigastric vein (SIEV); and (VII) abdominal wall structure. These steps should also be reviewed when marking the patient and planning the flap intra-operatively. While CTA has superior sensitivity and specificity in mapping perforator anatomy it also faces challenges due to ionising radiation exposure, contrast-induced allergy and potential nephrotoxicity.