A Case of May-Thurner Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Surgical Anatomy of the Common Iliac Veins During Para-Aortic and Pelvic Lymphadenectomy for Gynecologic Cancer
Original Article J Gynecol Oncol Vol. 25, No. 1:64-69 http://dx.doi.org/10.3802/jgo.2014.25.1.64 pISSN 2005-0380·eISSN 2005-0399 Surgical anatomy of the common iliac veins during para-aortic and pelvic lymphadenectomy for gynecologic cancer Kazuyoshi Kato, Shinichi Tate, Kyoko Nishikimi, Makio Shozu Department of Gynecology, Chiba University School of Medicine, Chiba, Japan See accompanying editorial by Lee on page 1. Objective: Compression of the left common iliac vein between the right common iliac artery and the vertebrae is known to be associated with the occurrence of left iliofemoral deep vein thrombosis (DVT). In this study, we described the variability in vascular anatomy of the common iliac veins and evaluated the relationship between the degree of iliac vein compression and the presence of DVT using the data from surgeries for gynecologic cancer. Methods: The anatomical variations and the degrees of iliac vein compression were determined in 119 patients who underwent systematic para-aortic and pelvic lymphadenectomy during surgery for primary gynecologic cancer. Their medical records were reviewed with respect to patient-, disease-, and surgery-related data. Results: The degrees of common iliac vein compression were classified into three grades: grade A (n=28, 23.5%), with a calculated percentage of 0%-25% compression; grade B (n=47, 39.5%), with a calculated percentage of 26%-50% compression; and grade C (n=44, 37%), with a calculated percentage of more than 50% compression. Seven patients (5.9%) had common iliac veins with anomalous anatomies; three were divided into small caliber vessels, two with a flattened structure, and two had double inferior vena cavae. -

Co-Existence of the Double Inferior Vena Cava with Complex Interiliac
Folia Morphol. Vol. 77, No. 1, pp. 151–155 DOI: 10.5603/FM.a2017.0074 C A S E R E P O R T Copyright © 2018 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Co-existence of the double inferior vena cava with complex interiliac venous communication and aberrant common hepatic artery arising from superior mesenteric artery: a case report V. Chentanez, N. Nateniyom, T. Huanmanop, S. Agthong Department of Anatomy, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand [Received: 19 June 2017; Accepted: 31 July 2017] Variations of the arterial and venous system of the abdomen and pelvis have im- portant clinical significance in hepatobiliary surgery, abdominal laparoscopy, and radiological intervention. A case of double inferior vena cava (IVC) with complex interiliac communication and variation of the common hepatic artery (CHA) arising from superior mesenteric artery (SMA) in a 79-year-old male cadaver is presented. Both IVCs ascended on either side of the abdominal aorta. The left-sided IVC crossed anterior to the aorta at the level of the left renal vein. The union of both IVCs was at the level just above the right renal vein. The diameter of right-sided IVC, left-sided IVC and the common IVC were 16.73 mm, 21.57 mm and 28.75 mm, respectively. In the pelvic cavity, the right common iliac vein was formed by a union of right external and internal iliac veins while the formation of left common iliac vein was from the external iliac vein and two internal iliac veins. An interiliac vein ran from right internal iliac vein to left common iliac vein with an additional communicating vein running from the middle of this interiliac vein to the right common iliac vein. -

Pelvic Venous Disorders
PELVIC VENOUS DISORDERS Anatomy and Pathophysiology Two Abdomino-Pelvic Compression Syndromes DIAGNOSIS of ABDOMINOO-PELVICP z Nutcracker Syndrome 9 Compression of the left renal vein COMPRESSIONCO SS O SYNDROMES S O with venous congestion of the left (with Emphasis on Duplex Ultrasound) kidney and left ovarian vein reflux R. Eugene Zierler, M.D. z May-Thurner Syndrome 9 Compression of the left common iliac vein by the right common The DD.. EE.. StrandnessStrandness,, JrJr.. Vascular Laboratory iliac artery with left lower University of Washington Medical Center extremity venous stasis and left DivisionDivision of Vascular Surgery internal iliac vein reflux University of Washington, School of Medicine ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome Left Renal Vein Entrapment z Grant 1937: Anatomical observation “…the left renal vein, as it lies between the aorta and superior mesenteric artery, resembles a nut between the jaws of a nutcracker.” X z El-Sadr 1950: Described first patient with the clinical syndrome X z De Shepper 1972: Named the disorder “Nutcracker Syndrome” Copy Here z Nutcracker Phenomenon z Nutcracker Syndrome 9 Anatomic finding only 9 Hematuria, proteinuria 9 Compression of left renal 9 Flank pain vein - medial narrowing 9 Pelvic pain/congestion with lateral (hilar) dilation 9 Varicocele ABDOMINO-PELVIC COMPRESSION ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome - Diagnosis Nutcracker Syndrome z Anterior Nutcracker z Posterior Nutcracker z Evaluate the left renal vein for aorto-mesenteric compression 9 Compression between -
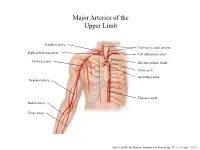
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

A Ureteral Mass Presenting As Deep Vein Thrombosis: a Very Rare Presentation
Urology & Nephrology Open Access Journal Case Report Open Access A ureteral mass presenting as deep vein thrombosis: a very rare presentation Abstract Volume 6 Issue 3 - 2018 Venous Thromboembolism is a dreaded condition. Many conditions and systemic Dushiant Sharma, Umesh Sharma, Sumit diseases are known to predispose to its occurrence including malignancy, pancreatitis, burns, clotting disorders and direct compression. All of these have been known to affect Gehlawat Department of Urology, RML Hospital & PGIMER, Delhi, India one or more factors in Virchows Triad proposed roughly a century ago.1 It consists of Hypercoagulability, Vascular Endothelial Dysfunction, Stasis. Stasis, one of the factors in Correspondence: Dushiant Sharma, Department of Urology, Virchows triad has been studied to a very small extent and it is this feature that is mostly Dr RML Hospital & PGIMER, Baba Khadak Singh Marg, New responsible for the development of Deep Vein Thrombosis (DVT) due to direct compression. Delhi, 110001, Tel 011-2340-4323, Email [email protected] Iliofemoral thrombosis in malignancy patients can be caused due to vein compression by pelvic malignancy and usually presents as unilateral lower limb swelling. In patients with Received: November 15, 2018 | Published: June 22, 2018 sudden onset of unilateral lower limb swelling without any perceived or diagnosed medical condition, detailed evaluation may lead to early identification, appropriate management and possibly cure. We present a case of acute unilateral ilio-femoral DVT caused by external compression by a mid-ureteric mass. Keywords: deep vein thrombosis, ileofemoral thrombosis, ureteric malignancy, upper tract urothelial cancers Abbreviations: DVT, Deep Vein Thrombosis; VTE, Venous Nephrouretectomy with bladder cuff excision was planned. -

Sources of Venous Blood Supply of Kidneys in Chicken of Haysex White Breed
M. V. Pervenetskaya et al /J. Pharm. Sci. & Res. Vol. 10(10), 2018, 2639-2641 Sources of Venous Blood Supply of Kidneys in Chicken of Haysex White Breed M. V. Pervenetskaya, L. V. Fomenko, G. A. Honin Omsk State Agrarian University named after P.A. Stolypin, 644008, Omsk, Russian Federation, Institutskaya Square, 1 Abstract: As a result of our studies, it has been found that blood from pelvic extremities in chicken flows along the right and left external iliac veins into the pelvic cavity. The caudal portal vein of the kidney branches from it in the caudal direction - from cranial part of kidneys. The caudal portal vein collects blood from middle and caudal parts of the kidney. The caudal portal vein, slightly bending in the caudomedial direction, joins the caudal portal vein from the opposite side. Coccygeal mesenteric vein branches from junctions of these veins. The right and left renal veins when joining together with an acute angle flow into the common iliac vein, which in turn enters caudal vena cava. Intraorgan veins of the kidney are divided into interlobular, perilobular, intralobular veins and capillaries. Venous blood from kidneys flows by three different ways. The first way is carried out by the hepatic veins from the midst and caudal parts of kidney. Firstly, these veins flow into the common iliac vein, and then into the caudal part of vena cava. The second way of outflow is carried out through the coccygeal mesenteric vein in the liver. The third way is carried out along the right and left cranial anterior portal veins from the anterior part of the kidney into the vertebral venous canal. -

In Situ Morphology of the Aorta and Common Iliac Artery in the Fetal and Neonatal Rat
003 1-3998/93/3303-0302$03.00/0 PEDIATRIC RESEARCH Vol. 33, No. 3, 1993 Copyright 0 1993 International Pediatric Research Foundation, Inc. Pr~ntedin U.S.A. In Situ Morphology of the Aorta and Common Iliac Artery in the Fetal and Neonatal Rat KAZUO MOMMA, TADAHIKO ITO, AND MASAHIKO AND0 Departmen1 ofpediutric Cardiology, The Heart Institute of Japan, Tokyo Women's Medical College, Tokyo, Japan ABSTRACT. In situ cross-sectional morphology of the cular morphology was studied using the rapid whole-body freez- ascending, descending, and abdominal aorta and the com- ing technique, as previously reported (3, 5-7). For fetal studies, mon iliac arteries was studied after rapid, whole-body six pregnant rats were killed on the 2 1 st d by cervical dislocation freezing of fetal and neonatal rats. In the fetus, the ascend- and frozen immediately in liquid nitrogen, followed by removal ing aorta was smaller than the descending aorta and the of the frozen fetuses. For the newborn rat study, 14 mother rats abdominal aorta was relatively large, continuing to the nursed newborns for 1, 2, 3, or 4 d, at which time the newborns large right common iliac artery and the umbilical artery. were frozen in dry ice-acetone. For the study of neonates im- After birth, the umbilical artery and the ductus arteriosus mediately after birth, fetuses were delivered by cesarean section closed rapidly, and the size of the aorta changed within a from two rats on the 21st d, the umbilical cord was cut bluntly, few days. The ascending aorta became larger than the and the fetuses were frozen immediately in dry ice-acetone. -

Ectopic Kidney in Front of the Right Common Iliac Artery and Its Blood Vascular Supply - a Case Report
Okajimas Folia Anat. Jpn., 70(1): 29-34, May, 1993 Ectopic Kidney in Front of the Right Common Iliac Artery and Its Blood Vascular Supply - a Case Report By Aiji OHTSUKA, Akio KIKUTA, Takehito TAGUCHI and Takuro MURAKAMI Human Morphology Section, Department of Anatomy, Okayama University School of Medicine, Okayama 700, Japan -Received for Publication, January 28, 1993- Key Words: Ectopic kidney, Renal blood vessels, Human, Anomaly, Gross anatomy Summary: A discoid-shaped ectopic kidney located in front of the right common iliac artery was observed in a 71-year-old Japanese man. The right kidney was normally positioned, but the left kidney was not observed in the normal position. The ureter of the ectopic kidney descended laterally to the left ductus deferens. The ectopic kidney received three arteries which arose from the anterior aspect of the abdominal aorta. Two of the arteries supplied the left half of the kidney. The other supplied the right half and gave off two branches to the adipose tissue around the right kidney; these branches meant that this artery belonged to the right side. Venous drainage from the kidney was handled by two veins. One collected venous radicles from the right half of the kidney and flowed into the inferior vena cava; this vein belonged to the right side. The other served the left half and joined with the left lumbar vein, which finally drained into the left common iliac vein; this vein was attributed to the left side. The present ectopic kidney had a left-side ureter, and vascular supply on both the right and left sides. -

Anomalous Communication Between Right Internal Iliac Vein
NUJHS Vol. 4, No.3, September 2014, ISSN 2249-7110 Nitte University Journal of Health Science Case Report ANOMALOUS COMMUNICATION BETWEEN RIGHT INTERNAL ILIAC VEIN AND LEFT COMMON ILIAC VEIN - A CASE REPORT Huban Thomas R.1, Prakashbabu B.2 & Radhakrishnan P.3 1 Senior Lecturer, 2 Associate Professor, 3 P.G. Student, Department of Anatomy, Kasturba Medical College, Manipal University, Manipal - 576 104. Karnataka, India. Correspondence : Huban Thomas R. Department of Anatomy, Kasturba Medical College, Manipal University, Manipal - 576 104, Karnataka, India. Mobile : +91 98443 43546 E-mail : [email protected] Abstract : Inferior vena cava (IVC) is formed by the union of the common iliac veins anterior to the body of the fifth lumbar vertebra, a little to its right side. It conveys blood to the right atrium from all the structures below the diaphragm. During routine educational dissection for medical undergraduates, we have come across a case of an anomalous communication between right internal iliac vein and left common iliac vein and a variation in the formation of inferior vena cava in a 55-year-old male cadaver. Due to its complex embryogenesis and relationship with other abdominal and thoracic structures, IVC may develop abnormally. These anatomical variations are often clinically silent and discovered incidentally. Knowledge of these variations may be helpful to clinicians and anatomists during surgical exploration, atypical clinical presentations and cadaveric findings. Keywords: Inferior vena cava, common iliac veins, internal iliac vein Introduction : the lower right, back side of the heart. The internal iliac vein (hypogastric vein) begins near the Case Presentation : upper part of the greater sciatic foramen, passes upward During routine educational dissection for medical behind and slightly medial to the Internal iliac artery and, at undergraduates, we have come across a case of an the brim of the pelvis, joins with the external iliac vein to anomalous communication between right internal iliac form the common iliac vein. -

Extensive DVT of the Femoral and External Iliac Veins Case Study
Clearing the Clot Case Report: The ZelanteDVT™ Thrombectomy Catheter for Venous Thrombosis Extending From the Popliteal to External Iliac Vein BY JEFFREY Y. WANG, MD, FACS his case study illustrates the endovascular manage- aggressive hydration. Patients receive postoperative educa- ment of venous thrombosis extending from the tion on potential signs and symptoms of internal bleeding, T popliteal vein to the external iliac vein utilizing a hemoglobinuria, and the importance of hydration. The two-part ambulatory venous pharmacomechanical throm- patient is then discharged to home and receives follow-up bectomy technique with the newest AngioJet™ catheter on calls the next morning and afternoon. the market, the 8-F ZelanteDVT™ catheter (Boston Scientific I primarily choose to use this technique for three reasons. Corporation). First, it has proven to be effective for me, with 90% to 100% thrombus clearance of the acute clot within the vessel AMBULATORY VENOUS THROMBECTOMY lumen. This does not include intermediate or chronic age TECHNIQUE thrombus, which is addressed with secondary interven- Two-part ambulatory venous thrombectomy is a tech- tion. Second, it has proven to be safe in my experience. nique that I developed 7 years ago that involves bringing the Although every patient will develop hemoglobinuria for patient into the procedure room to obtain access through 24 to 48 hours after the procedure, no patient has needed a distal vein—typically the popliteal for lower extremity periprocedure hospitalization or transfusion for bleeding. deep vein thrombosis (DVT). I deliver the lytic agent (usu- Third, it allows for the procedure to be performed within a ally 10 mg tPA mixed in 50 mL for a single limb) using the 6-hour period, including the 2-hour postprocedure recov- AngioJet Thrombectomy System in Power Pulse™ mode. -

A Rare Presentation of the Double Inferior Vena Cava with an Anomalous Retrocaval Right Ureter: Embryogenesis and Anatomy Section Clinical Implications
Case Report DOI: 10.7860/JCDR/2013/4576.2810 A Rare Presentation of the Double Inferior Vena Cava with an Anomalous Retrocaval Right Ureter: Embryogenesis and Anatomy Section Clinical Implications PRATIBHA GUPTA, MEENAKSHI KHULLAR, RaviKANT SHARMA, RICHHpaL SINGH ABSTRACT a venacaval duplication and its surgical implications, but here, On dissection of the abdomen of an adult male cadaver, in addition we are presenting a unique case of a double inferior vena cava to the normal inferior vena cava on the right side, an unusual with an anomalous retrocaval ureter. A conglo meration of such venous channel which connected the left renal vein with the left vascular malformations is of immense surgical importance, and common iliac vein was found; (probably the left inferior vena cava). it is indicative of a grossly defective angiogenesis. The left testicular and the left suprarenal veins were opening into Keeping in mind the clinical relevance of the variations which were the left renal vein as usual. Other than this, a retrocaval ureter was observed, an attempt was made to explain them in the light of the found on the right side. embryogenic development. The works of previous authors have highlighted the incidence of Key Words: Retrocaval ureter, Venacaval duplication, Angiogenesis INTRODUCTION been reported worldwide. It is reported to be present in 0.06- Embryogenesis of the Inferior Vena Cava (IVC) is a complex 0.17% of the autopsy materials. The incidence is greater in males process which involves the formation of anastomoses between than in females, with a ratio of 2.8:1 [3]. three paired embryonic veins.