Surgical Anatomy of the Common Iliac Veins During Para-Aortic and Pelvic Lymphadenectomy for Gynecologic Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PERIPHERAL VASCULATURE Average Vessel Diameter
PERIPHERAL VASCULATURE Average Vessel Diameter A Trio of Technologies. Peripheral Embolization Solutions A Single Solution. Fathom™ Steerable Guidewires Total Hypotube Tip Proximal/ UPN Length (cm) Length (cm) Length (cm) Distal O.D. Hepatic, Gastro-Intestinal and Splenic Vasculature 24 8-10 mm Common Iliac Artery 39 2-4 mm Internal Pudendal Artery M00150 900 0 140 10 10 cm .016 in 25 6-8 mm External Iliac Artery 40 2-4 mm Middle Rectal M00150 901 0 140 20 20 cm .016 in 26 4-6 mm Internal Iliac Artery 41 2-4 mm Obturator Artery M00150 910 0 180 10 10 cm .016 in 27 5-8 mm Renal Vein 42 2-4 mm Inferior Vesical Artery 28 43 M00150 911 0 180 20 20 cm .016 in 15-25 mm Vena Cava 2-4 mm Superficial Epigastric Artery 29 44 M00150 811 0 200 10 10 cm pre-shaped .014 in 6-8 mm Superior Mesenteric Artery 5-8 mm Femoral Artery 30 3-5 mm Inferior Mesenteric Artery 45 2-4 mm External Pudendal Artery M00150 810 0 200 10 10 cm .014 in 31 1-3 mm Intestinal Arteries M00150 814 0 300 10 10 cm .014 in 32 Male 2-4 mm Superior Rectal Artery A M00150 815 0 300 10 10 cm .014 in 33 1-3 mm Testicular Arteries 1-3 mm Middle Sacral Artery B 1-3 mm Testicular Veins 34 2-4 mm Inferior Epigastric Artery Direxion™ Torqueable Microcatheters 35 2-4 mm Iliolumbar Artery Female 36 2-4 mm Lateral Sacral Artery C 1-3 mm Ovarian Arteries Usable 37 D UPN Tip Shape RO Markers 3-5 mm Superior Gluteal Artery 1-3 mm Ovarian Veins Length (cm) 38 2-4 mm Inferior Gluteal Artery E 2-4 mm Uterine Artery M001195200 105 Straight 1 M001195210 130 Straight 1 M001195220 155 Straight 1 Pelvic -

Anatomy of the Large Blood Vessels-Veins
Anatomy of the large blood vessels-Veins Cardiovascular Block - Lecture 4 Color index: !"#$%&'(& !( "')*+, ,)-.*, $()/ Don’t forget to check the Editing File !( 0*"')*+, ,)-.*, $()/ 1$ ($&*, 23&%' -(0$%"'&-$(4 *3#)'('&-$( Objectives: ● Define veins, and understand the general principles of venous system. ● Describe the superior & inferior Vena Cava and their tributaries. ● List major veins and their tributaries in the body. ● Describe the Portal Vein. ● Describe the Portocaval Anastomosis Veins ◇ Veins are blood vessels that bring blood back to the heart. ◇ All veins carry deoxygenated blood. with the exception of the pulmonary veins(to the left atrium) and umbilical vein(umbilical vein during fetal development). Vein can be classified in two ways based on Location Circulation ◇ Superficial veins: close to the surface of the body ◇ Veins of the systemic circulation: NO corresponding arteries Superior and Inferior vena cava with their tributaries ◇ Deep veins: found deeper in the body ◇ Veins of the portal circulation: With corresponding arteries Portal vein Superior Vena Cava ◇Formed by the union of the right and left Brachiocephalic veins. ◇Brachiocephalic veins are formed by the union of internal jugular and subclavian veins. Drains venous blood from : ◇ Head & neck ◇ Thoracic wall ◇ Upper limbs It Passes downward and enter the right atrium. Receives azygos vein on its posterior aspect just before it enters the heart. Veins of Head & Neck Superficial veins Deep vein External jugular vein Anterior Jugular Vein Internal Jugular Vein Begins just behind the angle of mandible It begins in the upper part of the neck by - It descends in the neck along with the by union of posterior auricular vein the union of the submental veins. -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Rare Case of a Kidney and Inferior Vena Cava Abnormalities With
Clinics and Practice 2018; volume 8:1079 Rare case of a kidney and inferior vena cava Case Report Correspondence: Timir K. Paul, Division of Cardiology, Department of Medicine, East abnormalities with extensive A 27-year-old male with no significant Tennessee State University, 329 N State of lower extremity deep vein past medical history was admitted with Franklin Rd, Johnson City, TN 37604, USA. right lower extremity pain and swelling that Tel.: 423.979.4100 - Fax: 423.979.4134. thrombosis in a young started a week ago. Patient first noted E-mail: [email protected] healthy male swelling in the right ankle that was associ- ated with pain in the calf and thigh. Pain Key words: Deep vein thrombosis; Inferior vena cava hypoplasia; Renal hypoplasia. was described as progressively worsening Muhammad Khalid,1 1 1 with tightness and heaviness in the affected Contributions: MK wrote the initial manu- Manisha Nukavarapu, Rupal Shah, leg that was exacerbated with ambulation. 2 script draft and literature review; MN and RS Timir K. Paul Patient endorsed recent short duration of reviewed the initial draft with editions and TK 1Department of Medicine; 2Division of immobility involving a 4 hour road trip but did final revision and any edition as needed. Cardiology, Department of Medicine, denied any recent surgery, prior history of thrombosis, weight changes, new bone pain, Conflict of interest: the authors declare no East Tennessee State University, potential conflict of interest. Johnson City, TN, USA or history of easy bruising or bleeding. No known history of any congenital abnormal- Funding: none. ities, intra uterine growth restriction, oligo- hydramnios and no pregnancy related com- Received for publication: 6 May 2018. -

Cat Dissection
Cat Dissection Muscular Labs Tibialis anterior External oblique Pectroalis minor Sartorius Gastrocnemius Pectoralis major Levator scapula External oblique Trapezius Gastrocnemius Semitendinosis Trapezius Latissimus dorsi Sartorius Gluteal muscles Biceps femoris Deltoid Trapezius Deltoid Lumbodorsal fascia Sternohyoid Sternomastoid Pectoralis minor Pectoralis major Rectus abdominis Transverse abdominis External oblique External oblique (reflected) Internal oblique Lumbodorsal Deltoid fascia Latissimus dorsi Trapezius Trapezius Trapezius Deltoid Levator scapula Deltoid Trapezius Trapezius Trapezius Latissimus dorsi Flexor carpi radialis Brachioradialis Extensor carpi radialis Flexor carpi ulnaris Biceps brachii Triceps brachii Biceps brachii Flexor carpi radialis Flexor carpi ulnaris Extensor carpi ulnaris Triceps brachii Extensor carpi radialis longus Triceps brachii Deltoid Deltoid Deltoid Trapezius Sartorius Adductor longus Adductor femoris Semimembranosus Vastus Tensor fasciae latae medialis Rectus femoris Vastus lateralis Tibialis anterior Gastrocnemius Flexor digitorum longus Biceps femoris Tensor fasciae latae Semimembranosus Semitendinosus Gluteus medius Gluteus maximus Extensor digitorum longus Gastrocnemius Soleus Fibularis muscles Brachioradiallis Triceps (lateral and long heads) Brachioradialis Biceps brachii Triceps (medial head) Trapezius Deltoid Deltoid Levator scapula Trapezius Deltoid Trapezius Latissimus dorsi External oblique (right side cut and reflected) Rectus abdominis Transversus abdominis Internal oblique Pectoralis -

Co-Existence of the Double Inferior Vena Cava with Complex Interiliac
Folia Morphol. Vol. 77, No. 1, pp. 151–155 DOI: 10.5603/FM.a2017.0074 C A S E R E P O R T Copyright © 2018 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Co-existence of the double inferior vena cava with complex interiliac venous communication and aberrant common hepatic artery arising from superior mesenteric artery: a case report V. Chentanez, N. Nateniyom, T. Huanmanop, S. Agthong Department of Anatomy, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand [Received: 19 June 2017; Accepted: 31 July 2017] Variations of the arterial and venous system of the abdomen and pelvis have im- portant clinical significance in hepatobiliary surgery, abdominal laparoscopy, and radiological intervention. A case of double inferior vena cava (IVC) with complex interiliac communication and variation of the common hepatic artery (CHA) arising from superior mesenteric artery (SMA) in a 79-year-old male cadaver is presented. Both IVCs ascended on either side of the abdominal aorta. The left-sided IVC crossed anterior to the aorta at the level of the left renal vein. The union of both IVCs was at the level just above the right renal vein. The diameter of right-sided IVC, left-sided IVC and the common IVC were 16.73 mm, 21.57 mm and 28.75 mm, respectively. In the pelvic cavity, the right common iliac vein was formed by a union of right external and internal iliac veins while the formation of left common iliac vein was from the external iliac vein and two internal iliac veins. An interiliac vein ran from right internal iliac vein to left common iliac vein with an additional communicating vein running from the middle of this interiliac vein to the right common iliac vein. -

Pelvic Venous Disorders
PELVIC VENOUS DISORDERS Anatomy and Pathophysiology Two Abdomino-Pelvic Compression Syndromes DIAGNOSIS of ABDOMINOO-PELVICP z Nutcracker Syndrome 9 Compression of the left renal vein COMPRESSIONCO SS O SYNDROMES S O with venous congestion of the left (with Emphasis on Duplex Ultrasound) kidney and left ovarian vein reflux R. Eugene Zierler, M.D. z May-Thurner Syndrome 9 Compression of the left common iliac vein by the right common The DD.. EE.. StrandnessStrandness,, JrJr.. Vascular Laboratory iliac artery with left lower University of Washington Medical Center extremity venous stasis and left DivisionDivision of Vascular Surgery internal iliac vein reflux University of Washington, School of Medicine ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome Left Renal Vein Entrapment z Grant 1937: Anatomical observation “…the left renal vein, as it lies between the aorta and superior mesenteric artery, resembles a nut between the jaws of a nutcracker.” X z El-Sadr 1950: Described first patient with the clinical syndrome X z De Shepper 1972: Named the disorder “Nutcracker Syndrome” Copy Here z Nutcracker Phenomenon z Nutcracker Syndrome 9 Anatomic finding only 9 Hematuria, proteinuria 9 Compression of left renal 9 Flank pain vein - medial narrowing 9 Pelvic pain/congestion with lateral (hilar) dilation 9 Varicocele ABDOMINO-PELVIC COMPRESSION ABDOMINO-PELVIC COMPRESSION Nutcracker Syndrome - Diagnosis Nutcracker Syndrome z Anterior Nutcracker z Posterior Nutcracker z Evaluate the left renal vein for aorto-mesenteric compression 9 Compression between -

Multiple Variations of Branches of Abdominal Aorta Salve V M , Ratanprabha C
KATHMANDU UNIVERSITY MEDICAL JOURNAL Multiple Variations of Branches of Abdominal Aorta Salve V M , Ratanprabha C Dept.Of Anatomy ABSTRACT: Dr Pinnamaneni Siddhartha Institute Of Medical The Abdominal aorta and its major branches supply oxygenated blood to nearly Sciences & Reasearch Foundation, all the organs in the abdominal cavity. During routine dissection (January 2009) of a middle aged male cadaver at Dr. PSIMS, Gannavaram, Krishna Dist. (INDIA), Chinnaoutpalli, Gannavaram Mandal, the following variations of branches of abdominal aorta were found. The coeliac Krishna District, A.P. India trunk gave off three branches. The first branch was left inferior phrenic artery which arose directly from coeliac trunk. The second branch bifurcates into left gastric artery and accessory hepatic artery for left lobe of liver. The second branch gave off splenic artery and common hepatic artery. The right testicular artery took its origin from right aberrant renal artery. This variation was associated with the presence CORRESPONDING of bilateral aberrant renal arteries for lower poles of both kidneys arising from abdominal aorta and aberrant renal arteries bilateral for upper poles originating Dr Vishal M. Salve from the renal arteries. Anatomical variation of testicular arteries is reported to be 4.7 %. Apart from creating hazards during abdominal surgery, vascular variation can Associate Professor also become a technical problem for infusion therapy and chemoembolisation of neoplasm in the liver. Dept.Of Anatomy KEY WORDS Dr Pinnamaneni Siddhartha Institute Of Medical Sciences & Reasearch Foundation, Abdominal aorta, celiac trunk, aberrant renal arteries, accessory hepatic artery, inferior phrenic artery, splenic artery. Chinnaoutpalli, Gannavaram Mandal, Krishna District, A.P, India E-mail: [email protected] Citation Salve V M, Ratanprabha C. -

Pelvic Venous Reflux Diseases
Open Access Journal of Family Medicine Review Article Pelvic Venous Reflux Diseases Arbid EJ* and Antezana JN Anatomic Considerations South Charlotte General and Vascular Surgery, 10512 Park Road Suite111, Charlotte, USA Each ovary is drained by a plexus forming one major vein *Corresponding author: Elias J. Arbid, South measuring normally 5mm in size. The left ovarian plexus drains into Charlotte General and Vascular Surgery, 10512 Park Road left ovarian vein, which empties into left renal vein; the right ovarian Suite111, Charlotte, NC 28120, USA plexus drains into the right ovarian vein, which drains into the Received: November 19, 2019; Accepted: January 07, anterolateral wall of the inferior vena cava (IVC) just below the right 2020; Published: January 14, 2020 renal vein. An interconnecting plexus of veins drains the ovaries, uterus, vagina, bladder, and rectum (Figure 1). Introduction The lower uterus and vagina drain into the uterine veins and Varicose veins and chronic venous insufficiency are common then into branches of the internal iliac veins; the fundus of the uterus disorders of the venous system in the lower extremities that have drains to either the uterine or the ovarian plexus (utero-ovarian and long been regarded as not worthy of treatment, because procedures salpingo ovarian veins) within the broad ligament. Vulvoperineal to remove them were once perceived as worse than the condition veins drain into the internal pudendal vein, then into the inferior itself. All too frequently, patients are forced to learn to live with them, gluteal vein, then the external pudendal vein, then into the saphenous or find "creative" ways to hide their legs. -
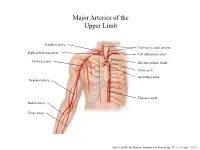
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

A Ureteral Mass Presenting As Deep Vein Thrombosis: a Very Rare Presentation
Urology & Nephrology Open Access Journal Case Report Open Access A ureteral mass presenting as deep vein thrombosis: a very rare presentation Abstract Volume 6 Issue 3 - 2018 Venous Thromboembolism is a dreaded condition. Many conditions and systemic Dushiant Sharma, Umesh Sharma, Sumit diseases are known to predispose to its occurrence including malignancy, pancreatitis, burns, clotting disorders and direct compression. All of these have been known to affect Gehlawat Department of Urology, RML Hospital & PGIMER, Delhi, India one or more factors in Virchows Triad proposed roughly a century ago.1 It consists of Hypercoagulability, Vascular Endothelial Dysfunction, Stasis. Stasis, one of the factors in Correspondence: Dushiant Sharma, Department of Urology, Virchows triad has been studied to a very small extent and it is this feature that is mostly Dr RML Hospital & PGIMER, Baba Khadak Singh Marg, New responsible for the development of Deep Vein Thrombosis (DVT) due to direct compression. Delhi, 110001, Tel 011-2340-4323, Email [email protected] Iliofemoral thrombosis in malignancy patients can be caused due to vein compression by pelvic malignancy and usually presents as unilateral lower limb swelling. In patients with Received: November 15, 2018 | Published: June 22, 2018 sudden onset of unilateral lower limb swelling without any perceived or diagnosed medical condition, detailed evaluation may lead to early identification, appropriate management and possibly cure. We present a case of acute unilateral ilio-femoral DVT caused by external compression by a mid-ureteric mass. Keywords: deep vein thrombosis, ileofemoral thrombosis, ureteric malignancy, upper tract urothelial cancers Abbreviations: DVT, Deep Vein Thrombosis; VTE, Venous Nephrouretectomy with bladder cuff excision was planned. -

Transection of Common Iliac Arteries and Veins Bilaterally a Survival After Bilateral Temporary Arterial Shunts and a Unique Postoperative Complication
European Journal of Trauma Case Study Transection of Common Iliac Arteries and Veins Bilaterally A Survival after Bilateral Temporary Arterial Shunts and a Unique Postoperative Complication Eric J. Kuncir, Demetrios Demetriades1 Abstract Case Study This is an unusual case report of a victim of a single J.M., a 23-year-old Hispanic male, sustained a single gunshot wound with transection of all four common gunshot wound to the left flank at about the mid axillary iliac vessels. The patient developed preoperative car- line at the level of the umbilicus. Los Angeles County diac arrest for which he underwent a successful resus- Paramedics responded quickly to the scene, and the citative thoracotomy. The iliac veins were managed by patient was unresponsive and had no obtainable vital ligation and the iliac arteries were stented as part of signs during transport. The patient arrived in the trauma damage control. The patient developed delayed acute room at LAC + USC 7 min later. Primary survey anuria due to ureteric obstruction secondary to bilater- revealed agonal respirations, a faintly palpable carotid al infected false iliac artery aneurysms. Reoperation pulse, and Glasgow Coma Score of 4. There was no visi- with ligation of the arteries and extra-anatomic ble active bleeding from a single wound to the left flank. axillofemoral and femorofemoral bypass was success- The patient was intubated by rapid sequence induction ful. The patient survived with weakness of the lower and was taken directly to the operating room (OR) extremities. without any investigation. He lost pulses during trans- port and a resuscitative left thoracotomy simultaneous Key Words with a midline laparotomy were performed in the OR 15 Iliac vessels · Damage control · False aneurysms min after initial arrival to the hospital.