Survival Analysis of Patients with Breast Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Autumn Issue, November 2003
Newsletter Autumn Issue, November 2003 Official Publication of Hong Kong College of Radiologists President’s Jottings Dr. Lilian Leong IN THIS ISSUE President’s Some of us had been engaging during the last few weeks and weekends in activities Jottings…………....1 relating to radiology or our College’s events. We had our Fellowship Part II examination, AGM………………3 our Annual Scientific meetings, the Ho Hung Chiu Lecture delivered by Prof. TSUI Lap Chee and our trip to Guangzhou, to participate in the 11th Annual Scientific Congress of ASM………….……3 Chinese Radiological Society (CCR). For our ASM, we had the highest number of Joint Admission registrants this year, reaching almost 500. Some overseas participants got the information Ceremony and H.C. Ho Lecture…….…5 from our website. They gave us the feedback that we should promote our ASM energetically as there could be a lot of overseas Chinese and non-Chinese professionals Exam Result…......7 interested to take a trip to Hong Kong and to attend some professional meetings. We also FRCR Exam had enthusiastic submissions of proffered papers and posters, more than last year. For our Schedule………......8 delegation to CCR, we had supported almost 20 delegates. It was the “largest” delegation Part 2 Fellowship so far, and we had put up scientific posters for the occasion. Course …………....8 CME ……………....9 11th CCR…………10 I had attended the CCR a number of times and I appreciate the rapid evolution of this PET……………....12 annual function of Chinese Radiological Society. This year, the participants reached almost 2000. There were seven parallel sessions, large number of electronic CME CIRSE ……….....13 demonstration and enthusiastic participation in lectures delivered in English. -

New Territories East Cluster Report 2012/13
1 TABLE OF CONTENTS Hospital Authority Vision, Mission and Values ........................................................................ 5 Message from CCE .................................................................................................................... 6 Messages from HCEs & DHCE ............................................................................................... 8 I. Overview of Cluster Performance ................................................................................ 10 II. Cluster Governance & Organization ........................................................................... 12 III. Key Achievements of Targets 2012/13 A. Allay Staff Shortage and High Turnover .................................................................... 16 B. Better Manage Growing Service Demand ................................................................... 16 C. Ensure Service Quality and Safety ............................................................................ 18 D. Enhance Partnership with Patients and Community .................................................. 20 E. Ensure Adequate Resources for Meeting Service Needs ............................................ 20 IV. Key Achievements of Cluster Functions 2012/13 A. Administrative Services ............................................................................................. 22 B. Communications ....................................................................................................... 25 C. Finance ................................................................................................................... -

North District Hospital Announces a Nurse Tested Preliminarily Positive to COVID-19
North District Hospital announces a nurse tested preliminarily positive to COVID-19 The following is issued on behalf of the Hospital Authority: The spokesperson for the North District Hospital made the following announcement today (January 20) regarding a nurse tested preliminarily positive to COVID-19: A nurse in the medical department started experiencing mild malaise on January 18. She attended a community testing centre for COVID-19 viral test yesterday (January 19) and was notified today that she has tested preliminary positive. She is now being treated under isolation at the Prince of Wales Hospital in stable condition. The nurse had worked in the isolation ward recently. Her daily clinical duties included taking care of COVID-19 patients and she had been wearing appropriate personal protective equipment during work. Her last date of duty was January 14. The hospital infection control team is working with the Centre for Health Protection (CHP) on contact tracing. Four nurses in the medical department who have had social gathering with the confirmed nurse in recent days are classified as close contact and quarantine will be arranged. They have all undergone COVID-19 tests and the results are pending. As the nurse has been wearing appropriate personal protective equipment during work, no patient is classified as close contact. As a precautionary measure, viral tests and medical surveillance are being arranged for relevant staff in the isolation ward and the department of medicine. Thorough cleansing and disinfection of the areas where the nurse has worked and rested has been arranged. The hospital will continue to closely monitor the health condition of the concerned staff members and communicate with the CHP on the latest situation. -

A General Brief About the Hospital Authority
Mission Statement 4. In keeping with its role, the Mission of the Hospital Authority is: · to meet the different needs of patients for public hospital services, and to improve the hospital environment for the benefit of patients; · to serve the public with care, dedication and efficiency, and to encourage community participation in the system, resulting in better care and more direct accountability to the public; · to provide rewarding, fair and challenging employment to all its staff, in an environment conducive to attracting, motivating and retaining well-qualified staff; · to advise the Government of the needs of the community for public hospital services and of the resources required to meet these needs, in order to provide adequate, efficient, effective and value for money public hospital services of the highest standards recognised internationally within the resources obtainable; and · to collaborate with other agencies and bodies in the healthcare and related fields both locally and overseas to provide the greatest benefit to the local community. Corporate Vision and Strategies 5. To realise its mission, the Hospital Authority has developed the following Corporate Vision: “The Hospital Authority will collaborate with other healthcare providers and carers in the community to create a seamless healthcare environment which will maximise healthcare benefits and meet community expectations.” 6. The Authority achieves this corporate vision by formulating a set of strategic directions every year through an extensive annual planning process, taking into account the funding position, societal expectations, Government’s healthcare policy, and the challenges in the internal and external environment. The 2 corporate vision and mission are turned into operational targets to meet the community needs for healthcare services. -
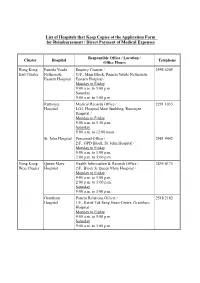
List of Hospitals That Keep Copies of the Application Form for Reimbursement / Direct Payment of Medical Expenses
List of Hospitals that Keep Copies of the Application Form for Reimbursement / Direct Payment of Medical Expenses Responsible Office / Location / Cluster Hospital Telephone Office Hours Hong Kong Pamela Youde Enquiry Counter / 2595 6205 East Cluster Nethersole G/F., Main Block, Pamela Youde Nethersole Eastern Hospital Eastern Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Ruttonjee Medical Records Office / 2291 1035 Hospital LG1, Hospital Main Building, Ruttonjee Hospital / Monday to Friday 9:00 a.m. to 5:30 p.m. Saturday 9:00 a.m. to 12:00 noon St. John Hospital Personnel Office / 2981 9442 2/F., OPD Block, St. John Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Hong Kong Queen Mary Health Information & Records Office / 2855 4175 West Cluster Hospital 2/F., Block S, Queen Mary Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Grantham Patient Relations Officer / 2518 2182 Hospital 1/F., Kwok Tak Seng Heart Centre, Grantham Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. - 2 - Responsible Office / Location / Cluster Hospital Telephone Office Hours Kowloon Kwong Wah Medical Report Office / 3517 5216 West Cluster Hospital 1/F., Central Stack, Kwong Wah Hospital / Monday to Friday 9:00 a.m. -

Department of Anesthesia University of Toronto Annual Report 2005
DEPARTMENT OF ANESTHESIA UNIVERSITY OF TORONTO ANNUAL REPORT 2005 – 2006 http://www.anesthesia.utoronto.ca 150 College Street Room 121 Fitzgerald Building Toronto, Ontario M5S 3E2 UNIVERSITY OF TORONTO – DEPARTMENT OF ANESTHESIA TABLE OF CONTENTS Message from the Chair ..................................................................................................................................................... 1 Anesthesia Fellows (2005-2006) ...................................................................................................................................... 3 Awards and Achievements ................................................................................................................................................ 4 Department Council ........................................................................................................................................................... 7 Undergraduate Education Committee ........................................................................................................................... 8 Postgraduate Education Committee ............................................................................................................................... 12 Anesthesia Residents (2005-2006) .................................................................................................................................. 14 U of T Fellowship Research Seminar Series ................................................................................................................. -

List of Medical Social Services Units Under Social Welfare Department
List of Medical Social Services Units Under Social Welfare Department Hong Kong Name of Hospital/Clinic Tel. No. Email Address 1. Queen Mary Hospital 2255 3762 [email protected] 2255 3764 2. Wong Chuk Hang Hospital 2873 7201 [email protected] 3. Pamela Youde Nethersole Eastern 2595 6262 [email protected] Hospital 4. Pamela Youde Nethersole Eastern 2595 6773 [email protected] Hospital (Psychiatric Department) Kowloon Name of Hospital/Clinic Tel. No. Email Address 5. Tseung Kwan O Hospital 2208 0335 [email protected] 2208 0327 6. United Christian Hospital 3949 5178 [email protected] (Psychiatry) 7. Queen Elizabeth Hospital 3506 7021 [email protected] 3506 7027 3506 5499 3506 4021 8. Hong Kong Eye Hospital 2762 3069 [email protected] 9. Kowloon Hospital Rehabilitation 3129 7857 [email protected] Building 10. Kowloon Hospital 3129 6193 [email protected] 11. Kowloon Hospital 2768 8534 [email protected] (Psychiatric Department) 1 The New Territories Name of Hospital/Clinic Tel. No. Email Address 12. Prince of Wales Hospital 3505 2400 [email protected] 13. Shatin Hospital 3919 7521 [email protected] 14. Tai Po Hospital 2607 6304 [email protected] Sub-office Tai Po Hospital (Child and Adolescent 2689 2486 [email protected] Mental Health Centre) 15. North District Hospital 2683 7750 [email protected] 16. Tin Shui Wai Hospital 3513 5391 [email protected] 17. Castle Peak Hospital 2456 7401 [email protected] 18. Siu Lam Hospital 2456 7186 [email protected] 19. -

Hospital Authority's Planned Projects for 2021-2022
LC Paper No. CB(4)503/20-21(02) Head 708 Subhead 8083MM One-Off Grant to the Hospital Authority for Minor Works Projects 2021-22 Planned Projects Prepared by the Hospital Authority February 2021 Head 708 : Subhead 8083MM One-off Grant to the Hospital Authority for Minor Works Projects for the 2019-20 Financial Year Part A - Previously approved items and other items to commence in 2020-21 with expected expenditure in 2020-21 and/or 2021-22 Actual Approved Cumulative Revised Estimated cash flow in subsequent years Expenditure Estimate Priority / Project Expenditure Estimate Project Title (1.4.2020 to 2021-22 Post Item No. Estimate to 31.3.2020 2020-21 31.10.2020) 2022-23 2023-24 2024-25 2024-25 ($'000) (I) Previously approved items (up to 31.10.2020) with expected expenditure in 2020-21 and/or 2021-22 EMR15-604 Modernisation of lifts in Day Treatment Block and Special Block in Prince of Wales Hospital 16,794 16,540 254 254 - - - - - EMR16-104 Replacement of the local central control and monitoring system for Wong Chuk Hang Hospital 1,280 1,150 39 101 - 30 - - - EMR16-401 Replacement of fire alarm and detection system at Hospital Main Block in Tseung Kwan O 6,500 6,500 (1,371) (1,371) - - - - - Hospital EMR16-504 Replacement of 1 no. main switch board for Block A in Yan Chai Hospital 2,345 2,202 142 142 - - - - - EMR16-505 Replacement of building management system at Multi Services Complex in Yan Chai Hospital 3,500 3,148 55 55 297 - - - - EMR16-506 Replacement of the air handling unit for Department of Central Supporting Services at 1/F, 502 526 (24) (24) - - - - - Block B in Yan Chai Hospital EMR17-102 Replacement of emergency generators for Hospital Block at St. -

Anaesthesia Related Mortality 2003-2005
Anaesthesia Related Mortality 2003-2005 Quality Subcommittee Co-ordinating Committee in Anaesthesiology Hospital Authority 1 8 May 2007 Anaesthesia Related Mortality 2003-2005 Introduction: • A territory wide audit in anaesthesia has not been conducted • Quality Assurance (QA) Subcommittee of the Co-ordinating Committee in Anaesthesiology of the Hospital Authority, conducted a HA wide audit on anaesthesia related mortality • Incidence of anaesthesia related mortality between the years 2003 and 2005 • Analysed the factors leading to death associated with anesthesia 2 8 May 2007 Anaesthesia Related Mortality 2003-2005 Methodology (1): • The primary endpoint of this audit, death within 30 days after surgery, was detected by comparing this list of patients with the Hong Kong Government Births and Death Registry • Since we used the criterion of death within 30 days after surgery, the search was extended to include deaths occurred before 30th January 2006 • The HA Health Informatics Section, together with the assistance of in-house statisticians also facilitated the search process 3 8 May 2007 Anaesthesia Related Mortality 2003-2005 Methodology (2): • The list of patients who received anaesthesia in one of the 20 HA hospitals between 1st January, 2003 and 31st December, 2005, was initially identified by the Clinical Data Analysis and Reporting System (CDARS) • The CDARS is a powerful tool developed by HA in 2002, it can be considered as a mega data warehouse with inputs from a number of source systems 4 8 May 2007 Anaesthesia Related Mortality -

(16 January 2018) List of Hospitals/Clinics Under the Hospital Authority
Social Welfare Department List of Medical Social Services Units (16 January 2018) List of Hospitals/Clinics under the Hospital Authority Hong Kong Name of Hospital/Clinic Address Tel. No. Fax. No. Opening Hours 1. Queen Mary Hospital J122, 1/F, Block J, 2255 3762 2872 8565 Mon – Fri: 8:45 am – 5:15 pm Queen Mary Hospital, 2255 3764 Lunch break: 1:00 pm to 2:00 pm Pokfulam Road, Hong Kong Sat: 9:00 am – 12:00 noon 2. Wong Chuk Hang Hospital G/F, Wong Chuk Hang Hospital, 2873 7201 2554 7318 Mon – Fri: 8:45 am – 5:15 pm 2 Wong Chuk Hang Path, Lunch break: 12:30 pm to 1:30 pm Wong Chuk Hang, Hong Kong Sat: 9:00 am – 12:00 noon 3. Western Psychiatric Centre G/F, South Wing, David Trench 2517 8141 2559 9464 Mon – Fri: 8:30 am – 6:00 pm Rehabilitation Centre, Lunch break: 1:00 pm to 2:00 pm 1F High Street, Hong Kong 4. Pamela Youde Nethersole Eastern Room 081, 1/F, Main Block, Pamela 2595 6262 2558 6023 Mon – Fri:8:45 am – 5:15 pm Hospital Youde Nethersole Eastern Hospital, Lunch break: 1:00 pm to 2:00 pm 3 Lok Man Road, Chai Wan, Sat: 9:00 am – 1:00 pm Hong Kong 5. Pamela Youde Nethersole Eastern 7/F, East Block, Pamela Youde 2595 6773 2557 4231 Mon – Fri: 8:45 am – 5:15 pm Hospital (Psychiatric Department) Nethersole Eastern Hospital, Lunch break: 1:00 pm to 2:00 pm 3 Lok Man Road, Sat: 9:00 am – 1:00 pm Chai Wan, Hong Kong Kowloon Name of Hospital/Clinic Address Tel. -

Reimbursement Forms in Designated Site
List of Hospitals that Keep Copies of Application FORM A and Application FORM B Responsible Office / Location / Cluster Hospital Telephone Office Hours Hong Kong Pamela Youde Enquiry Counter / 2595 6205 East Cluster Nethersole G/F., Main Block, Pamela Youde Nethersole Eastern Hospital Eastern Hospital / Monday to Friday 8:30 a.m. to 6:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Ruttonjee & Tang Medical Records Office / 2291 1035 Shiu Kin LG1, Hospital Main Building, Ruttonjee Hospitals Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. St. John Hospital Medical Records Office / Human Resources 2986 2246 Department/ 2/F., Out-Patients Block, St. John Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:30 p.m. Hong Kong Queen Mary Health Information & Records Office / 2255 4175 West Cluster Hospital 2/F., Block S, Queen Mary Hospital / (Monday to Monday to Friday Friday) 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Saturday 2255 3660 9:00 a.m. to 1:00 p.m. (Saturday) Grantham Health Information & Records Office / 2518 2201 Hospital G/F., Main Block, Grantham Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. - 2 - Responsible Office / Location / Cluster Hospital Telephone Office Hours Kowloon Kwong Wah Medical Report Office / 3517 5216 West Cluster Hospital 12/F., Central Stack, Kwong Wah Hospital / Monday to Friday 8:45 a.m. -

Full Paper In
S U P P L E M E N T 6 Volume 19 # Number 6 # DECEMBER 2013 Editor-in-Chief 3rd Hong Kong Neurological Congress cum 26th Annual Scientific Ignatius TS Yu 余德新 Meeting of The Hong Kong Neurological Society Senior Editors Council of The Hong Kong Neurological Society 4 PT Cheung 張璧濤 CB Chow 周鎮邦 Organising Committee 4 Albert KK Chui 徐家強 Michael G Irwin List of Speakers 5 TW Wong 黃大偉 Scientific Programme 6 Editors KL Chan 陳廣亮 SESSION ABSTRACT PAGE KS Chan 陳健生 Henry LY Chan 陳力元 FREE PAPER PRESENTATIONS David VK Chao 周偉強 Pilot Study for Subgroup Classification for Autism Spectrum FP 1 9 TW Chiu 趙多和 Disorder Based on Dysmorphology and Physical Stanley ST Choi 蔡兆堂 LW Chu 朱亮榮 Measurements in Chinese Paediatric and Adolescent WK Hung 熊維嘉 Population Bonnie CH Kwan 關清霞 Polly TY Wong, Virginia CN Wong Alvin KH Kwok 郭坤豪 Paul BS Lai 賴寶山 Promotion of Physical Activity and Fitness in the Parki-Fit & FP 2 10 Eric CH Lai 賴俊雄 Walk Program Addressing the Non-motor Symptom ‘Fatigue’ Stephen TS Lam 林德深 for Idiopathic Parkinson’s Disease Patrick CP Lau 劉志斌 CM Kwok, HT Lui, LF Hui, KY Wong Arthur CW Lau 劉俊穎 Nelson LS Lee 李禮舜 Cryptococcal Meningitis FP 3 11 Danny WH Lee 李偉雄 Helen Yip, MC Kwan, WK Cheng, WY Lau, KF Ko KY Leung 梁國賢 Danny TN Leung 梁子昂 A Young Lady with Artery of Percheron Infarction and Patent FP 4 12 Thomas WH Leung 梁慧康 Foramen Ovale WK Leung 梁惠強 SH Li, TY Wai, MF Ip, KK Ma Kenneth KW Li 李啟煌 David TL Liu 劉大立 Clinical and Genetic Evaluation of 23 Children with Infantile- FP 5 13 Janice YC Lo 羅懿之 onset Epileptic Encephalopathy Herbert HF Loong 龍浩鋒 Alvin