Summary of Product Characteristics 1. Name Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Lacidipine, Ramipril and Valsartan on Serum BNP Levels in Acute and Chronic Periods Following Isoproterenol-Induced Myocardial Infarction in Rats
Original Article Effects of Lacidipine, Ramipril and Valsartan on Serum BNP Levels in Acute and Chronic Periods Following Isoproterenol-Induced Myocardial Infarction in Rats Lasidipin, Ramipril ve Valsartanın Sıçanlarda Isoprotrenol ile Uyarılan Miyokard Infarktüsü Sonrası Akut ve Kronik Periyotta Serum BNP Seviyeleri Üzerine Etkileri Yasin Bayir1, Elif Cadirci2, Halis Suleyman2, Zekai Halici2, Mevlut Sait Keles3 1Ataturk University, Faculty of Pharmacy, Department of Biochemistry, Erzurum, Turkey 2Ataturk University, Faculty of Medicine, Department of Pharmacology, Erzurum, Turkey 3Ataturk University, Faculty of Medicine, Department of Biochemistry, Erzurum, Turkey Correspondence to: Elif Cadirci, Ph.D., Atatürk University, Faculty of Medicine, Department of Pharmacology, 25240, Erzurum, Turkey. Phone: +90.442.2316563, Fax: +90.442.2360968, e-mail: [email protected] Abstract Özet Objective. Myocardial infarction (MI) as a result of cardiovas- Amaç. Miyokard infarktüsü (Mİ) hem gelişmiş hem de cular disease is the principal cause of death in both developed gelişmekte olan ülkelerde kardiyovasküler hastalıklar sonucu and developing countries. Brain natriuretic peptide (BNP) is an oluşan ölümün esas sebebidir. Brain natriuretic peptide (BNP) important marker of cardiac failure. Cardioprotective activities kardiyak hasarın önemli bir göstergesidir. Antihipertansif il- of the antihypertensive drugs lacidipine (LAC), ramipril (RAM) açlar olan lasidipin (LAC), ramipril (RAM) ve valsartanın, izo- and valsartan (VAL), against isoproterenol -

LGM-Pharma-Regulatory-1527671011
Pipeline Products List Specialty Portfolio Updated Q2 2018 Updated Q2 2018 See below list of newly approved API’s, samples are readily available for your R&D requirements: Inhalation Ophthalmic Transdermal Sublingual Abaloparatide Defibrotide Sodium Liraglutide Rituximab Abciximab Deforolimus Lixisenatide Rivastigmine Aclidinium Bromide Azelastine HCl Agomelatine Alprazolam Abemaciclib Delafloxacin Lumacaftor Rivastigmine Hydrogen Tartrate Beclomethasone Dipropionate Azithromycin Amlodipine Aripiprazole Acalabrutinib Denosumab Matuzumab Rizatriptan Benzoate Budesonide Besifloxacin HCl Apomorphine Eletriptan HBr Aclidinium Bromide Desmopressin Acetate Meloxicam Rocuronium Bromide Adalimumab Difluprednate Memantine Hydrochloride Rolapitant Flunisolide Bimatoprost Clonidine Epinephrine Aflibercept Dinoprost Tromethamine Micafungin Romidepsin Fluticasone Furoate Brimonidine Tartrate Dextromethorphan Ergotamine Tartrate Agomelatine Dolasetron Mesylate Mitomycin C Romosozumab Fluticasone Propionate Bromfenac Sodium Diclofenac Levocetrizine DiHCl Albiglutide Donepezil Hydrochloride Mometasone Furoate Rotigotine Formoterol Fumarate Cyclosporine Donepezil Meclizine Alectinib Dorzolamide Hydrochloride Montelukast Sodium Rucaparib Iloprost Dexamethasone Valerate Estradiol Melatonin Alemtuzumab Doxercalciferol Moxifloxacin Hydrochloride Sacubitril Alirocumab Doxorubicin Hydrochloride Mycophenolate Mofetil Salmeterol Xinafoate Indacaterol Maleate Difluprednate Fingolimod Meloxicam Amphotericin B Dulaglutide Naldemedine Secukinumab Levalbuterol Dorzolamide -

2 Total Pharmaceutical Sales
OECD Health Statistics 2021 Definitions, Sources and Methods Total pharmaceutical sales Total sales of pharmaceutical products on the domestic market, in total and by selected Anatomical Therapeutic Chemical (ATC) classification groups, based on retail prices (which means the final price paid by the customer). The ATC codes below are based on the 2021 version of the ATC Index. All alterations implemented from January 2021 are available on the WHO Collaborating Centre for Drug Statistics Methodology website at http://www.whocc.no/atc/lists_of_new_atc_ddds_and_altera/alterations_in_atc_ddd/. Note: There are at least three possible sources of under-reporting of drug sales in different countries: 1) sales data may only cover those drugs that are reimbursed by public insurance schemes; 2) they may be based on ex-factory or wholesale prices rather than retail prices; and 3) sales data may exclude drug consumption in hospitals. Data for the following countries under-estimate pharmaceutical sales reported in this section because of one of these limitations: Australia, Austria, France, Germany, Greece, Japan, Luxembourg, the Netherlands, the Slovak Republic (before 2016) and Spain. (For further information, see the country-specific information below). Please also note that depending on the allocation of pharmaceutical products with more than one use, differences in reporting of specific drugs may occur across countries, thereby affecting the relative size of specific ATC groups. Data should reflect total sales for each drug category, based on -

Summary of Product Characteristics
Proposed var 24 psusa cilazapril SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [Fosinopril sodium 10 mg, tablets] [Fosinopril sodium 20 mg, tablets] 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 10 or 20 mg fosinopril sodium. Excipient with known effect: Each tablet fosinopril sodium 10 mg contains 87 mg of lactose, anhydrous. Each tablet fosinopril sodium 20 mg contains 174 mg of lactose, anhydrous. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet. The 10 mg tablets are white and shaped like a capsule with indents. On one side they are engraved with the letters “APO” and on the other side with “FOS-10”. The 20 mg tablets are white and their shape is oval. On one side they are engraved with the letters “APO” and on the other side with “FOS-20”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications - Treatment of hypertension. - Treatment of symptomatic heart failure. 4.2 Posology and method of administration Posology Fosinopril sodium should be administered orally in a single daily dose. As with all other medicinal products taken once daily, it should be taken at approximately the same time each day. The absorption of fosinopril sodium is not affected by food. The dose should be individualised according to patient profile and blood pressure response (see section 4.4). Hypertension: Fosinopril sodium may be used as a monotherapy or in combination with other classes of antihypertensive medicinal products (see section 4.3, 4.4, 4.5 and 5.1). Hypertensive patients not being treated with diuretics: Starting dose The initial recommended dose is 10 mg once a day. -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -

ENTRESTO (Sacubitril and Valsartan) Is a Combination of a Neprilysin Inhibitor and an Angiotensin II Receptor Blocker
HIGHLIGHTS OF PRESCRIBING INFORMATION • Adjust adult doses every 2 to 4 weeks and pediatric doses every 2 weeks These highlights do not include all the information needed to use to the target maintenance dose, as tolerated by the patient. (2.2, 2.3) ENTRESTO safely and effectively. See full prescribing information for • Reduce starting dose to half the usually recommended starting dosage for: ENTRESTO. – patients not currently taking an ACE inhibitor or ARB or previously ENTRESTO® (sacubitril and valsartan) tablets, for oral use taking a low dose of these agents (2.5) Initial U.S. Approval: 2015 – patients with severe renal impairment (2.6) – patients with moderate hepatic impairment (2.7) WARNING: FETAL TOXICITY See full prescribing information for complete boxed warning. ----------------------DOSAGE FORMS AND STRENGTHS-------------------- • When pregnancy is detected, discontinue ENTRESTO as soon as • Film-coated tablets: 24/26 mg; 49/51 mg; 97/103 mg (3) possible. (5.1) --------------------------------CONTRAINDICATIONS---------------------------- • Drugs that act directly on the renin-angiotensin system can cause • Hypersensitivity to any component. (4) injury and death to the developing fetus. (5.1) • History of angioedema related to previous ACEi or ARB therapy. (4) • ----------------------------RECENT MAJOR CHANGES------------------------- Concomitant use with ACE inhibitors. (4, 7.1) • • Indications and Usage, Adult Heart Failure (1.1) 2/2021 Concomitant use with aliskiren in patients with diabetes. (4, 7.1) ----------------------------INDICATIONS AND USAGE-------------------------- ------------------------WARNINGS AND PRECAUTIONS---------------------- ENTRESTO is indicated: • Observe for signs and symptoms of angioedema and hypotension. (5.2, 5.3) • to reduce the risk of cardiovascular death and hospitalization for heart • Monitor renal function and potassium in susceptible patients. -

Minutes of PRAC Meeting on 09-12 July 2018
6 September 2018 EMA/PRAC/576790/2018 Inspections, Human Medicines Pharmacovigilance and Committees Division Pharmacovigilance Risk Assessment Committee (PRAC) Minutes of the meeting on 09-12 July 2018 Chair: June Raine – Vice-Chair: Almath Spooner Health and safety information In accordance with the Agency’s health and safety policy, delegates were briefed on health, safety and emergency information and procedures prior to the start of the meeting. Disclaimers Some of the information contained in the minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scope listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also change during the course of the review. Additional details on some of these procedures will be published in the PRAC meeting highlights once the procedures are finalised. Of note, the minutes are a working document primarily designed for PRAC members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006, Rev. 1). 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. -

Medication Risks in Older Patients with Cancer
Medication risks in older patients with cancer 1 Medication risks in older patients (70+) with cancer and their association with therapy-related toxicity Imke Ortland1, Monique Mendel Ott1, Michael Kowar2, Christoph Sippel3, Yon-Dschun Ko3#, Andreas H. Jacobs2#, Ulrich Jaehde1# 1 Institute of Pharmacy, Department of Clinical Pharmacy, University of Bonn, An der Immenburg 4, 53121 Bonn, Germany 2 Department of Geriatrics and Neurology, Johanniter Hospital Bonn, Johanniterstr. 1-3, 53113 Bonn, Germany 3 Department of Oncology and Hematology, Johanniter Hospital Bonn, Johanniterstr. 1-3, 53113 Bonn, Germany # equal contribution Corresponding author Ulrich Jaehde Institute of Pharmacy University of Bonn An der Immenburg 4 53121 Bonn, Germany Phone: +49 228-73-5252 Fax: +49-228-73-9757 [email protected] Medication risks in older patients with cancer 2 Abstract Objectives To evaluate medication-related risks in older patients with cancer and their association with severe toxicity during antineoplastic therapy. Methods This is a secondary analysis of two prospective, single-center observational studies which included patients ≥ 70 years with cancer. The patients’ medication was investigated regarding possible risks: polymedication (defined as the use of ≥ 5 drugs), potentially inadequate medication (PIM; defined by the EU(7)-PIM list), and relevant potential drug- drug interactions (rPDDI; analyzed by the ABDA interaction database). The risks were analyzed at two different time points: before and after start of cancer therapy. Severe toxicity during antineoplastic therapy was captured from medical records according to the Common Terminology Criteria for Adverse Events (CTCAE). The association between Grade ≥ 3 toxicity and medication risks was evaluated by univariate regression. -

Summary of Product Characteristics 1. NAME of the MEDICINAL
Summary of product characteristics 1. NAME OF THE MEDICINAL PRODUCT Losartan Potassium 50 mg Film-coated Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 50 mg of losartan potassium, equivalent to 45.8mg of Losartan. Excipient: 52mg of lactose/film-coated tablet. For the full list of excipients see section 6.1 3. PHARMACEUTICAL FORM Film-coated tablet White to off white, round, biconvex, film-coated tablets with breakline on one side and “50” debossing on other side. The break line is only to facilitate breaking for ease of swallowing and not to divide into equal doses 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of essential hypertension in adults and in children and adolescents 6-18 years of age. Treatment of renal disease in adult patients with hypertension and type 2 diabetes mellitus with proteinuria 0.5 g/day as part of an antihypertensive treatment (see sections 4.3, 4.4, 4.5 and 5.1). Treatment of chronic heart failure in adult patients when treatment with Angiotensin converting enzyme (ACE) inhibitors is not considered suitable due to incompatibility, especially cough, or contraindication. Patients with heart failure who have been stabilised with an ACE inhibitor should not be switched to losartan. The patients should have a left ventricular ejection fraction ≤ 40% and should be clinically stable and on an established treatment regimen for chronic heart failure. Reduction in the risk of stroke in adult hypertensive patients with left ventricular hypertrophy documented by ECG (see section 5.1 LIFE study, Race). 4.2 Posology and method of administration Posology Hypertension The usual starting and maintenance dose is 50 mg once daily for most patients. -
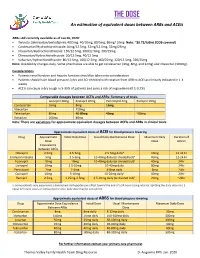
THE DOSE an Estimation of Equivalent Doses Between Arbs and Aceis
THE DOSE An estimation of equivalent doses between ARBs and ACEIs ARBs still currently available as of Jan 26, 2020: Twynsta (telmisartan/amlodipine): 40/5mg. 40/10mg, 80/5mg, 80mg/ 10mg Note: ~$0.73/tablet (ODB covered) Candesartan/Hydrochlorothiazide:16mg/12.5mg, 32mg/12.5mg, 32mg/25mg Irbesartan/Hydrochlorothiazide: 150/12.5mg, 300/12.5mg, 300/25mg Olmesartan/Hydrochlorothiaizde: 20/12.5mg, 40/12.5mg Valsartan/Hydrochlorothiazide: 80/12.5mg, 160/12.5mg, 160/25mg, 320/12.5mg, 320/25mg Note: Availability changes daily. Some pharmacies are able to get candesartan (4mg, 8mg, and 32mg) and irbesartan (300mg). Considerations Patients renal function and hepatic function should be taken into consideration Patients should have blood pressure, lytes and SCr checked with rotation from ARB to ACEI as clinically indicated in 1-4 weeks ACEIs can cause a dry cough in 5-35% of patients and carry a risk of angioedema (0.1-0.2%) Comparable dosages between ACEIs and ARBs- Summary of trials Lisinopril 20mg Enalapril 20mg Perindopril 4mg Ramipril 10mg Candesartan 16mg 8mg 16mg Irbesartan 150mg Telmisartan 80mg 40-80mg 40mg ~80mg Valsartan 160mg 80mg Note: There are variations for approximate equivalent dosages between ACEIs and ARBs in clinical trials. Approximate equivalent doses of ACEI for blood pressure lowering Drug Approximate Initial Daily Dose Usual Daily Maintenance Dose Maximum Daily Duration of Dose Dose Action Equivalence Between ACEIs Cilazapril 2.5mg 2.5-5mg 2.5-5mg dailya 10mg 12-24 hr Enalapril maleate 5mg 2.5-5mg 10-40mg daily (or divided bid)a 40mg 12-24 hr Fosinopril 10mg 10mg 10-40mg daily (or divided bid)a 40mg 24hr Lisinopril 10mg 2.5-10mg 10-40mg daily 80mg 24hr Perindopril 2mg 2-4mg 4-8mg daily 8mg 24hr Quinapril 10mg 5-10mg 10-20mg dailya 40mg 24hr Ramipril 2.5mg 1.25mg-2.5mg 2.5-10mg daily (or divided bid)a 20mg ~24hr a: Some patients may experience a diminished antihypertensive effect toward the end of a 24-hour dosing interval. -

Angiotensin-Converting Enzyme (ACE) Inhibitors
Angiotensin-Converting Enzyme (ACE) Inhibitors Summary Blood pressure reduction is similar for the ACE inhibitors class, with no clinically meaningful differences between agents. Side effects are infrequent with ACE inhibitors, and are usually mild in severity; the most commonly occurring include cough and hypotension. Captopril and lisinopril do not require hepatic conversion to active metabolites and may be preferred in patients with severe hepatic impairment. Captopril differs from other oral ACE inhibitors in its rapid onset and shorter duration of action, which requires it to be given 2-3 times per day; enalaprilat, an injectable ACE inhibitor also has a rapid onset and shorter duration of action. Pharmacology Angiotensin Converting Enzyme Inhibitors (ACE inhibitors) block the conversion of angiotensin I to angiotensin II through competitive inhibition of the angiotensin converting enzyme. Angiotensin is formed via the renin-angiotensin-aldosterone system (RAAS), an enzymatic cascade that leads to the proteolytic cleavage of angiotensin I by ACEs to angiotensin II. RAAS impacts cardiovascular, renal and adrenal functions via the regulation of systemic blood pressure and electrolyte and fluid balance. Reduction in plasma levels of angiotensin II, a potent vasoconstrictor and negative feedback mediator for renin activity, by ACE inhibitors leads to increased plasma renin activity and decreased blood pressure, vasopressin secretion, sympathetic activation and cell growth. Decreases in plasma angiotensin II levels also results in a reduction in aldosterone secretion, with a subsequent decrease in sodium and water retention.[51035][51036][50907][51037][24005] ACE is found in both the plasma and tissue, but the concentration appears to be greater in tissue (primarily vascular endothelial cells, but also present in other organs including the heart). -

Hyponatremia Induced by Angiotensin Converting Enzyme Inhibitors and Angiotensin
DOI: 10.7860/JCDR/2018/31983.11754 Original Article Hyponatremia Induced by Angiotensin Converting Enzyme Inhibitors and Angiotensin Pharmacology Section Receptor Blockers-A Pilot Study S BHUVANESHWARI1, PRAKASH VEL SANKHYA SAROJ2, D VIJAYA3, M SABARI SOWMYA4, R SENTHIL KUMAR5 ABSTRACT Results: Among all, 48% (24 out of 50) of the study population Introduction: Hyponatremia, serum sodium <135 mmol/L, can administered with ACEI and ARB developed hyponatremia. result in neurological manifestation in acute cases, may lead Predisposition to develop hyponatremia was high in males to seizures and coma. Angiotensin Converting Enzyme Inhibitor compared to females. Incidence of hyponatremia was 62.5% (10 (ACEI) and Angiotensin II Receptor Blockers (ARB) are drugs out of 16) in the age group of 56-75 years. Though, incidence of that have been commonly prescribed for the treatment of hyponatremia was 54.5% (18 out of 33) in ACEI group compared hypertension and cardiac diseases. It has become important to 35.2% (6 out of 17) in ARB group, but it was not statistically to evaluate and investigate the incidence of hyponatremia on significant. The study also revealed that metosartan had a higher consumption of these drugs. association with hyponatremia compared to other drugs. Aim: To determine the susceptibility of patients on ACEI and Conclusion: Hyponatremia was induced in nearly 50% of ARB to hyponatremia and to ascertain the drug producing patients taking ACEI and ARB. The incidence of hyponatremia notable hyponatremia among ACEI and ARB. among patients on these two drugs did not show statistical variation. Metosartan showed a higher incidence of Materials and Methods: The study was conducted in a tertiary hyponatremia compared to enalapril, ramipril, captopril, care hospital.