PAPS 2016 Kauai Booklet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Changes in Tzu Chi. by Yu-Shuang Yao and Richard Gombrich
Changes in Tzu Chi. By Yu-Shuang Yao and Richard Gombrich, October 2014. Tzu Chi will soon be fifty years old. Since 2010 it has been the subject of almost 300 graduate theses written in Taiwan, and that number will surely have increased before this paper is published.1 There has been widespread criticism of Tzu Chi for its lack of traditional Buddhist ritual and public observance of Buddhist festivals. Indeed, the movement has generally appeared somewhat austere in its lack of ritual and public spectacle, an austerity very much in the spirit of Tai Xu’s criticism of the Chinese Buddhism of his day. This year, on May 11th, Tzu Chi showed a new face to the world. The Buddha’s birthday (according to the Chinese Buddhist calendar) was celebrated in every branch of Tzu Chi worldwide. In Hualien the Master herself presided over a spectacular celebration involving, we estimate, nearly 2000 participants. These participants included the Tzu Chi nuns, who live in Hualien at the Abode, the movement’s headquarters; they normally lead reclusive lives and are not seen in public; so far as we can tell, this is the first time that they have taken part in any public ceremony. A similar ceremony was held on an even larger scale in Taipei at the Chiang Kai Shek Memorial Hall, and was observed by 300 members of the Buddhist Saṅgha who had been invited from around the world. This is the first time that representatives of other Buddhist movements, let alone ordained members of those movements, have been invited by Tzu Chi. -

Wrestling Masks in Chicano and Mexican Performance Art
Studies in 20th Century Literature Volume 25 Issue 2 Article 6 6-1-2001 (Ef)Facing the Face of Nationalism: Wrestling Masks in Chicano and Mexican Performance Art Robert Neustadt Northern Arizona University Follow this and additional works at: https://newprairiepress.org/sttcl Part of the American Literature Commons, Latin American Literature Commons, and the Modern Literature Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Neustadt, Robert (2001) "(Ef)Facing the Face of Nationalism: Wrestling Masks in Chicano and Mexican Performance Art ," Studies in 20th Century Literature: Vol. 25: Iss. 2, Article 6. https://doi.org/10.4148/ 2334-4415.1510 This Article is brought to you for free and open access by New Prairie Press. It has been accepted for inclusion in Studies in 20th Century Literature by an authorized administrator of New Prairie Press. For more information, please contact [email protected]. (Ef)Facing the Face of Nationalism: Wrestling Masks in Chicano and Mexican Performance Art Abstract Masks serve as particularly effective props in contemporary Mexican and Chicano performance art because of a number of deeply rooted traditions in Mexican culture. This essay explores the mask as code of honor in Mexican culture, and foregrounds the manner in which a number of contemporary Mexican and Chicano artists and performers strategically employ wrestling masks to (ef)face the mask- like image of Mexican or U.S. nationalism. I apply the label "performance artist" broadly, to include musicians and political figures that integrate an exaggerated sense of theatricality into their performances. -

Buddhist Revivalist Movements Comparing Zen Buddhism and the Thai Forest Movement Buddhist Revivalist Movements Alan Robert Lopez Buddhist Revivalist Movements
Alan Robert Lopez Buddhist Revivalist Movements Comparing Zen Buddhism and the Thai Forest Movement Buddhist Revivalist Movements Alan Robert Lopez Buddhist Revivalist Movements Comparing Zen Buddhism and the Thai Forest Movement Alan Robert Lopez Chiang Mai , Thailand ISBN 978-1-137-54349-3 ISBN 978-1-137-54086-7 (eBook) DOI 10.1057/978-1-137-54086-7 Library of Congress Control Number: 2016956808 © The Editor(s) (if applicable) and The Author(s) 2016 This work is subject to copyright. All rights are solely and exclusively licensed by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. Cover image © Nickolay Khoroshkov / Alamy Stock Photo Printed on acid-free paper This Palgrave Macmillan imprint is published by Springer Nature The registered company is Nature America Inc. -
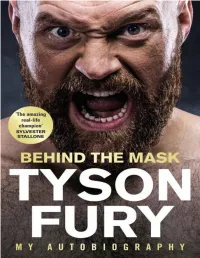
Behind the Mask: My Autobiography
Contents 1. List of Illustrations 2. Prologue 3. Introduction 4. 1 King for a Day 5. 2 Destiny’s Child 6. 3 Paris 7. 4 Vested Interests 8. 5 School of Hard Knocks 9. 6 Rolling with the Punches 10. 7 Finding Klitschko 11. 8 The Dark 12. 9 Into the Light 13. 10 Fat Chance 14. 11 Wild Ambition 15. 12 Drawing Power 16. 13 Family Values 17. 14 A New Dawn 18. 15 Bigger than Boxing 19. Illustrations 20. Useful Mental Health Contacts 21. Professional Boxing Record 22. Index About the Author Tyson Fury is the undefeated lineal heavyweight champion of the world. Born and raised in Manchester, Fury weighed just 1lb at birth after being born three months premature. His father John named him after Mike Tyson. From Irish traveller heritage, the“Gypsy King” is undefeated in 28 professional fights, winning 27 with 19 knockouts, and drawing once. His most famous victory came in 2015, when he stunned longtime champion Wladimir Klitschko to win the WBA, IBF and WBO world heavyweight titles. He was forced to vacate the belts because of issues with drugs, alcohol and mental health, and did not fight again for more than two years. Most thought he was done with boxing forever. Until an amazing comeback fight with Deontay Wilder in December 2018. It was an instant classic, ending in a split decision tie. Outside of the ring, Tyson Fury is a mental health ambassador. He donated his million dollar purse from the Deontay Wilder fight to the homeless. This book is dedicated to the cause of mental health awareness. -

Everybodyâ•Žs Mrs. Fahrenheit
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Digital Commons @ Butler University Booth Volume 6 | Issue 8 Article 3 8-15-2014 Everybody’s Mrs. Fahrenheit Dan Mancilla Follow this and additional works at: http://digitalcommons.butler.edu/booth Recommended Citation Mancilla, Dan (2014) "Everybody’s Mrs. Fahrenheit," Booth: Vol. 6: Iss. 8, Article 3. Available at: http://digitalcommons.butler.edu/booth/vol6/iss8/3 This Article is brought to you for free and open access by Digital Commons @ Butler University. It has been accepted for inclusion in Booth by an authorized administrator of Digital Commons @ Butler University. For more information, please contact [email protected]. Everybody’s Mrs. Fahrenheit Abstract The asl t time they’d seen each other Buddy Frazier Jr. and Paul Runyon were digging thumbtacks and plywood splinters from one another’s tormented skin, the aftermath of their EXPLOSION!!! OF LOVE: BLACK HAWK STREET FIGHT thirteen years ago. “Black Hawk,” because that was where the show had taken place. “Love,” because they had been feuding over Babe the Blue Fox... Cover Page Footnote "Everybody's Mrs. Fahrenheit" was originally published at Booth. This article is available in Booth: http://digitalcommons.butler.edu/booth/vol6/iss8/3 Mancilla: Everybody’s Mrs. Fahrenheit ! ! August 15,! 2014 Everybody’s Mrs. Fahrenheit ! Fiction by Dan Mancilla ! The last time they’d seen each other Buddy Frazier Jr. and Paul Runyon were digging thumbtacks and plywood splinters from one another’s tormented skin, the aftermath of their EXPLOSION!!! OF LOVE: BLACK HAWK STREET FIGHT thirteen years ago. -

Buddhist Bibio
Recommended Books Revised March 30, 2013 The books listed below represent a small selection of some of the key texts in each category. The name(s) provided below each title designate either the primary author, editor, or translator. Introductions Buddhism: A Very Short Introduction Damien Keown Taking the Path of Zen !!!!!!!! Robert Aitken Everyday Zen !!!!!!!!! Charlotte Joko Beck Start Where You Are !!!!!!!! Pema Chodron The Eight Gates of Zen !!!!!!!! John Daido Loori Zen Mind, Beginner’s Mind !!!!!!! Shunryu Suzuki Buddhism Without Beliefs: A Contemporary Guide to Awakening ! Stephen Batchelor The Heart of the Buddha's Teaching: Transforming Suffering into Peace, Joy, and Liberation!!!!!!!!! Thich Nhat Hanh Buddhism For Beginners !!!!!!! Thubten Chodron The Buddha and His Teachings !!!!!! Sherab Chödzin Kohn and Samuel Bercholz The Spirit of the Buddha !!!!!!! Martine Batchelor 1 Meditation and Zen Practice Mindfulness in Plain English ! ! ! ! Bhante Henepola Gunaratana The Four Foundations of Mindfulness in Plain English !!! Bhante Henepola Gunaratana Change Your Mind: A Practical Guide to Buddhist Meditation ! Paramananda Making Space: Creating a Home Meditation Practice !!!! Thich Nhat Hanh The Heart of Buddhist Meditation !!!!!! Thera Nyanaponika Meditation for Beginners !!!!!!! Jack Kornfield Being Nobody, Going Nowhere: Meditations on the Buddhist Path !! Ayya Khema The Miracle of Mindfulness: An Introduction to the Practice of Meditation Thich Nhat Hanh Zen Meditation in Plain English !!!!!!! John Daishin Buksbazen and Peter -

Religions of the World
Religions of the World This encyclopedia series provides comprehensive coverage of “world reli- gions.” Cohesive and objective in its treatment, the series covers a wide spectrum of academic disciplines and religious traditions. It lays bare similar- ities and differences that naturally emerge within and across disciplines and religions today. The series includes the academic field of multidisciplinary, secular study of religious beliefs, behaviors, and institutions. It offers descrip- tions, comparisons, interpretations, and explanations on religions in many different regions of the world. The series emphasizes systematic, historically based, and cross-cultural perspectives. Each volume offers a “state of play” perspective regarding the specific area of the world being considered, looking both at the current situation and at likely further developments within that area. More information about this series at https://www.springer.com/series/15065 Henri Gooren Editor Encyclopedia of Latin American Religions With 19 Figures and 17 Tables Editor Henri Gooren Sociology, Anthropology, Social Work and Criminal Justice Oakland University Rochester, MI, USA ISBN 978-3-319-27077-7 ISBN 978-3-319-27078-4 (eBook) ISBN 978-3-319-28571-9 (print and electronic bundle) https://doi.org/10.1007/978-3-319-27078-4 Library of Congress Control Number: 2019933396 © Springer Nature Switzerland AG 2019 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. -

Taiwan's Tzu Chi As Engaged Buddhism
BSRV 30.1 (2013) 137–139 Buddhist Studies Review ISSN (print) 0256-2897 doi: 10.1558/bsrv.v30i1.137 Buddhist Studies Review ISSN (online) 1747-9681 Taiwan’s Tzu Chi as Engaged Buddhism: Origins, Organization, Appeal and Social Impact, by Yu-Shuang Yao. Global Oriental, Brill, 2012. 243pp., hb., £59.09/65€/$90, ISBN-13: 9789004217478. Reviewed by Ann Heirman, Oriental Languages and Cultures, Ghent University, Belgium. Keywords Tzu Chi, Taiwanese Buddhism, Engaged Buddhism Taiwan’s Tzu Chi as Engaged Buddhism is a well-written book that addresses a most interesting topic in Taiwanese Buddhism, namely the way in which Engaged Buddhism found its way into Taiwan in, and through, the Tzu Chi Foundation (the Buddhist Compassion Relief Tzu Chi Foundation). Founded in 1966, the Foundation expanded in the 1990s, and so became the largest lay organiza- tion in a contemporary Chinese context. The overwhelming involvement of the laity introduced a new aspect, and has triggered major changes in Taiwanese Buddhism. The present book offers a most welcome comprehensive study of the Foundation, discussing its context, development, structure, teaching and prac- tices. With its focus on both the history and the social context, the work devel- ops an interesting interdisciplinary approach, offering valuable insights into the appeal of the movement to a Taiwanese public. Nevertheless, some remarks still need to be made. The work is based on research that was completed in 2001, and research updates have not been pro- duced since, apart from a small Afterword (pp. 228-230). Yet not publishing the present work would have been a loss to the scientific community. -

Bridging Worlds: Buddhist Women's Voices Across Generations
BRIDGING WORLDS Buddhist Women’s Voices Across Generations EDITED BY Karma Lekshe Tsomo First Edition: Yuan Chuan Press 2004 Second Edition: Sakyadhita 2018 Copyright © 2018 Karma Lekshe Tsomo All rights reserved No part of this book may not be reproduced or utilized in any form or by any means, electronic or mechanical, or by any information storage or retreival system, without the prior written permission from the publisher, except in the case of brief quotations. Cover Illustration, "Woman on Bridge" © 1982 Shig Hiu Wan. All rights reserved. "Buddha" calligraphy ©1978 Il Ta Sunim. All rights reserved. Chapter Illustrations © 2012 Dr. Helen H. Hu. All rights reserved. Book design and layout by Lillian Barnes Bridging Worlds Buddhist Women’s Voices Across Generations EDITED BY Karma Lekshe Tsomo 7th Sakyadhita International Conference on Buddhist Women With a Message from His Holiness the XIVth Dalai Lama SAKYADHITA | HONOLULU, HAWAI‘I iv | Bridging Worlds Contents | v CONTENTS MESSAGE His Holiness the XIVth Dalai Lama xi ACKNOWLEDGMENTS xiii INTRODUCTION 1 Karma Lekshe Tsomo UNDERSTANDING BUDDHIST WOMEN AROUND THE WORLD Thus Have I Heard: The Emerging Female Voice in Buddhism Tenzin Palmo 21 Sakyadhita: Empowering the Daughters of the Buddha Thea Mohr 27 Buddhist Women of Bhutan Tenzin Dadon (Sonam Wangmo) 43 Buddhist Laywomen of Nepal Nivedita Kumari Mishra 45 Himalayan Buddhist Nuns Pacha Lobzang Chhodon 59 Great Women Practitioners of Buddhadharma: Inspiration in Modern Times Sherab Sangmo 63 Buddhist Nuns of Vietnam Thich Nu Dien Van Hue 67 A Survey of the Bhikkhunī Saṅgha in Vietnam Thich Nu Dong Anh (Nguyen Thi Kim Loan) 71 Nuns of the Mendicant Tradition in Vietnam Thich Nu Tri Lien (Nguyen Thi Tuyet) 77 vi | Bridging Worlds UNDERSTANDING BUDDHIST WOMEN OF TAIWAN Buddhist Women in Taiwan Chuandao Shih 85 A Perspective on Buddhist Women in Taiwan Yikong Shi 91 The Inspiration ofVen. -
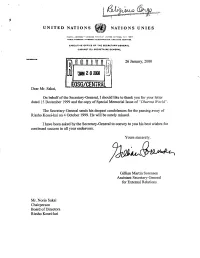
EOSG/CENTRAL Dear Mr
UNITED NATIONS NATIONS UNIES POSTAL ADDRESS ADRESSE POST ALE- UNITED NATIONS, N.V. 1OO17 CABLE AODflCSS ADRESSE TELEGRAPHIQUE: I/NATIONS NEWYORK EXECUTIVE OFFICE OF THE SECRETARY-GENERAL CABINET OU SECRETAIRE GENERAL REFERENCE: 26 January, 2000 EOSG/CENTRAL Dear Mr. Sakai, On behalf of the Secretary-General, I should like to thank you for your letter dated 15 December 1999 and the copy of Special Memorial Issue of "Dharma World". The Secretary-General sends his deepest condolences for the passing away of Rissho Kosei-kai on 4 October 1999. He will be surely missed. I have been asked by the Secretary-General to convey to you his best wishes for continued success hi all your endeavors. Yours sincerely, Gillian Martin Sorensen Assistant Secretary-General for External Relations Mr. Norio Sakai Chairperson Board of Directors Rissho Kosei-kai RISSHO KOSEI-KAI C, A BUDDHIST ORGANIZATION 2-11-1 Wada, Suginami-ku, Tokyo 166-8537, Japan, Tel: 03-3383-1111 lilJLU DEC 2 9 I999 December 15, 1999 Dear Sir/Madam, Special Memorial Issue of Dharrna World I would like to express my heartfelt gratitude for your friendship with Rissho Kosei-kai. As you may know, Founder Nikkyo Niwano peacefully passed away on October 4, 1999 at the age of 92. The enclosed Special Memorial Issue of Dharma World carries full details of the Founder's funeral ceremonies and a complete review of his life and work. I am very pleased to present this issue to you as a token of our wholehearted appreciation. Founder's posthumous name is "If^JLEIifc—SfbfcfiirlJ" (Kaiso Nikkyo Ichijo Daishi) in Japanese and "The Founder Nikkyo, Great Teacher of the One Vehicle" in English. -

Overview of Actions Taken by Buddhist Tzu Chi Foundation (BTCF)
Buddhist Tzu Chi Foundation COVID-19 Relief Action Report #4 Overview of Actions taken by Buddhist Tzu Chi Foundation (BTCF) As of 12 May, BTCF has: ● Distributed relief aid in 53 countries/regions (blue) with more distributions on the way for another 28 countries/regions (orange) ● A total of 14,466,805 items have been distributed with a further 7,440,677 items scheduled to be distributed ● Mid-term COVID-19 relief action plans have been initiated by BTCF chapters around the world including financial aid, material supplies and caring social support Buddhist Tzu Chi Foundation COVID-19 Relief Action Report #4 Highlights by Region: Asia The Asia region, consisting of around 60% of the world’s population, is the most populated and diverse region in the world. Being the epicentre of the COVID-19 pandemic, most countries/regions in Asia experienced or are still experiencing severe lockdown restrictions. The cascading decline on local and national economy, along with lack of income and steep inflation of daily costs, have left our vulnerable communities struggling, wondering where their next meal may be. BTCF, founded in this region, has been supporting local Region Highlights communities for over half a century. Immediately, in early February, BTCF disaster management protocols were initiated and teams from different regions were dispatched to contact families Malaysia and individuals in our care. Understanding their needs, BTCF ● Care assistance for vulnerable communities. chapters quickly established suitable action plans and began the ● Long term partnerships paving the way for procurement of food supplies, necessities and personal protective COVID-19 co-operation. -

2019 Annual Report
TZU CHI USA Buddhist Tzu Chi Foundation 2019 ANNUAL REPORT LETTER FROM THE CEO Wish All Living Beings Happiness and provided free medical care internationally, for 15,877 patients Freedom From Suffering in need in Ecuador and Mexico. As part of our long-term relief, we also rebuilt a church destroyed by the 2016 earthquake Tzu Chi USA, established in 1989, reached a major milestone in Ecuador and began reconstruction of the Morelos Institute in 2019, marking 30 years of service. Today, we have 66 offi ces destroyed in the 2017 earthquake in Mexico. in 25 states, with volunteers offering relief with compassion through Tzu Chi’s missions. Tzu Chi USA’s character education program continued to thrive in California and Texas. Implemented in eight schools, Addressing the needs of underserved populations and it provided 33,853 classes that reached 2,264 students. And, underprivileged families was at the forefront of our charity with the grand opening of the Tzu Chi Center in New York City mission in 2019. Our food pantry program helped families in in October, we now have a new home from which to inspire need across America, benefi ting 16,811 households, comprising care and compassion through exhibits that document Tzu Chi’s 109,688 individuals. In addition, our winter distributions humanitarian activities around the world. provided care to 2,608 individuals, offering $21,550 in cash cards, 1,116 eco-blankets & eco-scarves, and other essentials. We express our gratitude to all who supported Tzu Chi, and to all the agencies and organizations that partnered with us.