"Radial-Paralysis" Syndrome in the Dog John G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications
diagnostics Article The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications F. Kip Sawyer 1,2,* , Joshua J. Stefanik 3 and Rebecca S. Lufler 1 1 Department of Medical Education, Tufts University School of Medicine, Boston, MA 02111, USA; rebecca.lufl[email protected] 2 Department of Anesthesiology, Stanford University School of Medicine, Stanford, CA 94305, USA 3 Department of Physical Therapy, Movement and Rehabilitation Science, Bouve College of Health Sciences, Northeastern University, Boston, MA 02115, USA; [email protected] * Correspondence: [email protected] Received: 20 May 2020; Accepted: 29 May 2020; Published: 2 June 2020 Abstract: Background: This study attempted to clarify the innervation pattern of the muscles of the distal arm and posterior forearm through cadaveric dissection. Methods: Thirty-five cadavers were dissected to expose the radial nerve in the forearm. Each muscular branch of the nerve was identified and their length and distance along the nerve were recorded. These values were used to determine the typical branching and motor entry orders. Results: The typical branching order was brachialis, brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, supinator, extensor digitorum, extensor carpi ulnaris, abductor pollicis longus, extensor digiti minimi, extensor pollicis brevis, extensor pollicis longus and extensor indicis. Notably, the radial nerve often innervated brachialis (60%), and its superficial branch often innervated extensor carpi radialis brevis (25.7%). Conclusions: The radial nerve exhibits significant variability in the posterior forearm. However, there is enough consistency to identify an archetypal pattern and order of innervation. These findings may also need to be considered when planning surgical approaches to the distal arm, elbow and proximal forearm to prevent an undue loss of motor function. -
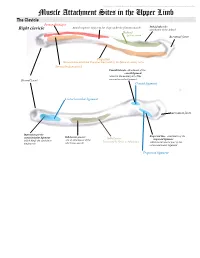
Muscle Attachment Sites in the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Muscle Attachment Sites in the Upper Limb The Clavicle Pectoralis major Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: Right clavicle attachment of the deltoid Deltoid Axillary nerve Acromial facet Trapezius Sternocleidomastoid and Trapezius innervated by the Spinal Accessory nerve Sternocleidomastoid Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Conoid ligament Costoclavicular ligament Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Subclavian groove: Subclavius trapezoid ligament which binds the clavicle to site of attachment of the Innervated by Nerve to Subclavius which is the lateral part of the the first rib subclavius muscle coracoclavicular ligament Trapezoid ligament This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. The Scapula Trapezius Right scapula: posterior Levator scapulae Supraspinatus Deltoid Deltoid and Teres Minor are innervated by the Axillary nerve Rhomboid minor Levator Scapulae, Rhomboid minor and Rhomboid Major are innervated by the Dorsal Scapular Nerve Supraspinatus and Infraspinatus innervated by the Suprascapular nerve Infraspinatus Long head of triceps Rhomboid major Teres Minor Teres Major Teres Major -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

Examination of the Shoulder Bruce S
Examination of the Shoulder Bruce S. Wolock, MD Towson Orthopaedic Associates 3 Joints, 1 Articulation 1. Sternoclavicular 2. Acromioclavicular 3. Glenohumeral 4. Scapulothoracic AC Separation Bony Landmarks 1. Suprasternal notch 2. Sternoclavicular joint 3. Coracoid 4. Acromioclavicular joint 5. Acromion 6. Greater tuberosity of the humerus 7. Bicipital groove 8. Scapular spine 9. Scapular borders-vertebral and lateral Sternoclavicular Dislocation Soft Tissues 1. Rotator Cuff 2. Subacromial bursa 3. Axilla 4. Muscles: a. Sternocleidomastoid b. Pectoralis major c. Biceps d. Deltoid Congenital Absence of Pectoralis Major Pectoralis Major Rupture Soft Tissues (con’t) e. Trapezius f. Rhomboid major and minor g. Latissimus dorsi h. Serratus anterior Range of Motion: Active and Passive 1. Abduction - 90 degrees 2. Adduction - 45 degrees 3. Extension - 45 degrees 4. Flexion - 180 degrees 5. Internal rotation – 90 degrees 6. External rotation – 45 degrees Muscle Testing 1. Flexion a. Primary - Anterior deltoid (axillary nerve, C5) - Coracobrachialis (musculocutaneous nerve, C5/6 b. Secondary - Pectoralis major - Biceps Biceps Rupture- Longhead Muscle Testing 2. Extension a. Primary - Latissimus dorsi (thoracodorsal nerve, C6/8) - Teres major (lower subscapular nerve, C5/6) - Posterior deltoid (axillary nerve, C5/6) b. Secondary - Teres minor - Triceps Abduction Primary a. Middle deltoid (axillary nerve, C5/6) b. Supraspinatus (suprascapular nerve, C5/6) Secondary a. Anterior and posterior deltoid b. Serratus anterior Deltoid Ruputure Axillary Nerve Palsy Adduction Primary a. Pectoralis major (medial and lateral pectoral nerves, C5-T1 b. Latissimus dorsi (thoracodorsal nerve, C6/8) Secondary a. Teres major b. Anterior deltoid External Rotation Primary a. Infraspinatus (suprascapular nerve, C5/6) b. Teres minor (axillary nerve, C5) Secondary a. -

Brachial Plexus Posterior Cord Variability: a Case Report and Review
CASE REPORT Brachial plexus posterior cord variability: a case report and review Edward O, Arachchi A, Christopher B Edward O, Arachchi A, Christopher B. Brachial plexus posterior cord anatomical variability. This case report details the anatomical variants discovered variability: a case report and review. Int J Anat Var. 2017;10(3):49-50. in the posterior cord of the brachial plexus in a routine cadaveric dissection at the University of Melbourne, Australia. Similar findings in the literature are reviewed ABSTRACT and the clinical significance of these findings is discussed. The formation and distribution of the brachial plexus is a source of great Key Words: Brachial plexus; Posterior cord; Axillary nerve; Anatomical variation INTRODUCTION he brachial plexus is the neural network that supplies motor and sensory Tinnervation to the upper limb. It is typically composed of anterior rami from C5 to T1 spinal segments, which subsequently unite to form superior, middle and inferior trunks. These trunks divide and reunite to form cords 1 surrounding the axillary artery, which terminate in branches of the plexus. The posterior cord is classically described as a union of the posterior divisions from the superior, middle and inferior trunks of the brachial plexus, with fibres from all five spinal segments. The upper subscapular, thoracodorsal and lower subscapular nerves propagate from the cord prior to the axillary and radial nerves forming terminal branches. Variability in the brachial plexus is frequently reported in the literature. It is C5 nerve root Suprascapular nerve important for clinicians to be aware of possible variations when considering Posterior division of C5-C6 injuries or disease of the upper limb. -

Variations in the Branching Pattern of the Radial Nerve Branches to Triceps Brachii
Review Article Clinician’s corner Images in Medicine Experimental Research Case Report Miscellaneous Letter to Editor DOI: 10.7860/JCDR/2019/39912.12533 Original Article Postgraduate Education Variations in the Branching Pattern Case Series of the Radial Nerve Branches to Anatomy Section Triceps Brachii Muscle Short Communication MYTHRAEYEE PRASAD1, BINA ISAAC2 ABSTRACT Results: The branching patterns seen were types A 1 (3.6%), Introduction: The axillary nerve arises from the posterior cord B1 (1st pattern) 1 (3.6%), B2 (2nd pattern) 1 (3.6%), and C3 of the brachial plexus and supplies the deltoid and teres minor 22 (78.6%). Two new patterns observed were: type B2 muscles. Axillary nerve injuries lead to abduction and external (6th pattern) 1 (3.6%) and type D (2nd pattern) 2 (7.1%). The long rotation weakness. In such cases, branches to the heads of head had single innervation in 89.3% cases and the lateral and triceps brachii muscle have been transferred to the axillary nerve medial heads had dual innervation in 10.7% and 7.1% cases to establish reinnervation of the deltoid muscle. In addition, the respectively. triceps nerve branches can be nerve recipients to reinstitute Conclusion: The knowledge of the different branching patterns elbow extension. that are present will help surgeons to identify the most suitable Aim: To study the different branching patterns of the radial radial nerve branch to triceps brachii that can be used for nerve nerve branches to triceps brachii muscle. transfer to restore the motor function of the deltoid muscle or to reanimate the triceps brachii muscle. -

Posterior Interosseous Neuropathy Supinator Syndrome Vs Fascicular Radial Neuropathy
Posterior interosseous neuropathy Supinator syndrome vs fascicular radial neuropathy Philipp Bäumer, MD ABSTRACT Henrich Kele, MD Objective: To investigate the spatial pattern of lesion dispersion in posterior interosseous neurop- Annie Xia, BSc athy syndrome (PINS) by high-resolution magnetic resonance neurography. Markus Weiler, MD Methods: This prospective study was approved by the local ethics committee and written Daniel Schwarz, MD informed consent was obtained from all patients. In 19 patients with PINS and 20 healthy con- Martin Bendszus, MD trols, a standardized magnetic resonance neurography protocol at 3-tesla was performed with Mirko Pham, MD coverage of the upper arm and elbow (T2-weighted fat-saturated: echo time/repetition time 52/7,020 milliseconds, in-plane resolution 0.27 3 0.27 mm2). Lesion classification of the radial nerve trunk and its deep branch (which becomes the posterior interosseous nerve) was performed Correspondence to Dr. Bäumer: by visual rating and additional quantitative analysis of normalized T2 signal of radial nerve voxels. [email protected] Results: Of 19 patients with PINS, only 3 (16%) had a focal neuropathy at the entry of the radial nerve deep branch into the supinator muscle at elbow/forearm level. The other 16 (84%) had proximal radial nerve lesions at the upper arm level with a predominant lesion focus 8.3 6 4.6 cm proximal to the humeroradial joint. Most of these lesions (75%) followed a specific somato- topic pattern, involving only those fascicles that would form the posterior interosseous nerve more distally. Conclusions: PINS is not necessarily caused by focal compression at the supinator muscle but is instead frequently a consequence of partial fascicular lesions of the radial nerve trunk at the upper arm level. -

Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies
Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies Zachary Simmons, MD* KEYWORDS Brachial plexus Brachial plexopathy Axillary nerve Musculocutaneous nerve Suprascapular nerve Nerve conduction studies Electromyography KEY POINTS The brachial plexus provides all motor and sensory innervation of the upper extremity. The plexus is usually derived from the C5 through T1 anterior primary rami, which divide in various ways to form the upper, middle, and lower trunks; the lateral, posterior, and medial cords; and multiple terminal branches. Traction is the most common cause of brachial plexopathy, although compression, lacer- ations, ischemia, neoplasms, radiation, thoracic outlet syndrome, and neuralgic amyotro- phy may all produce brachial plexus lesions. Upper extremity mononeuropathies affecting the musculocutaneous, axillary, and supra- scapular motor nerves and the medial and lateral antebrachial cutaneous sensory nerves often occur in the context of more widespread brachial plexus damage, often from trauma or neuralgic amyotrophy but may occur in isolation. Extensive electrodiagnostic testing often is needed to properly localize lesions of the brachial plexus, frequently requiring testing of sensory nerves, which are not commonly used in the assessment of other types of lesions. INTRODUCTION Few anatomic structures are as daunting to medical students, residents, and prac- ticing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, Conflicts of Interest: None. Neuromuscular Program and ALS Center, Penn State Hershey Medical Center, Penn State College of Medicine, PA, USA * Department of Neurology, Penn State Hershey Medical Center, EC 037 30 Hope Drive, PO Box 859, Hershey, PA 17033. -

The Course of the Radial Nerve in Relation to the Humerus: a Cadaveric Study in a Kenyan Adult Population
Research article East African Orthopaedic Journal THE COURSE OF THE RADIAL NERVE IN RELATION TO THE HUMERUS: A CADAVERIC STUDY IN A KENYAN ADULT POPULATION V. Lusweti, MBChB, MMed (Ortho Surg), R. Oluoch, MBChB, MMed (Ortho Surg Registrar), B. R. Ayumba, MMed (Gen Surg), MMed (Ortho), Department of Orthopaedics and Rehabilitation, Moi University, A.Njoroge, MBChB, MMed (Ortho Surg), AO Trauma Fellow and M.G.Y. Elbadawi, MBChB, PhD (Clin Anatomy), Department of Human Anatomy, Moi University, P. O. Box 4606 – 30100, Eldoret, Kenya Correspondence to: Dr. Victor Lusweti, Department of Orthopaedic Surgery and Rehabilitation, College of Health Sciences, School of Medicine, Moi University, P.O. Box 4606–30100, Eldoret, Kenya. Email: luswetibaraza@ gmail.com ABSTRACT Background: The radial nerve arises from the posterior cord of the brachial plexus. It descends distally to the spiral groove of the humerus. The upper and lower margins of this groove form important landmarks relative to the acromion process, medial and lateral epicondyles of the humerus. Objective: To describe the course of the radial nerve in relation to the humerus in a Kenyan adult population. Methods: Dissections were done on fifty-nine left sided formalin fixed adult upper extremities obtained from the Human Anatomy Laboratory of Moi University. Data was recorded and analysed using SPSS version 21. Results: The average humeral length was 314.4 ± 21.4mm. The radial nerve was located 140.8 ± 17.2 mm from the tip of the acromion. It exited the spiral groove 185.1 ± 21.7mm from the tip of the acromion and 132.1 ± 19.4 mm from the lateral epicondyle. -

Tricks and Techniques to Maximize Success with Nerve Transfers
IC12-L: Tricks and Techniques to Maximize Success with Nerve Transfers Moderator(s): Susan E. Mackinnon, MD Faculty: Christine B. Novak, PT, PhD and J. Megan Patterson, MD Session Handouts Friday, October 02, 2020 75TH VIRTUAL ANNUAL MEETING OF THE ASSH OCTOBER 1-3, 2020 822 West Washington Blvd Chicago, IL 60607 Phone: (312) 880-1900 Web: www.assh.org Email: [email protected] All property rights in the material presented, including common-law copyright, are expressly reserved to the speaker or the ASSH. No statement or presentation made is to be regarded as dedicated to the public domain. IC12 – Tricks and Techniques to Maximize Success with Nerve Transfers American Society for Surgery of the Hand Annual Meeting, October 2, 2020 Susan E. Mackinnon, MD, St. Louis, Missouri J. Megan M. Patterson, Chapel Hill, North Carolina Christine B. Novak, PT, PhD, Toronto, Ontario Andrew Yee, BS, St. Louis, Missouri Overview: Following complex nerve injury, motor and sensory recovery can be less than optimal. For high median, ulnar and radial nerve injuries, nerve transfers can provide a distal source of motor and/or sensory innervation closer to the target end organ allowing for faster recovery and improved outcome. This course will focus on techniques to maximize success with upper extremity motor and sensory nerve transfers. Classification of Nerve Injury: Degree of Injury Tinel’s Sign Recovery Rate of Surgical Procedure Present Recovery I Neurapraxia No Complete Up to 12 weeks None II Axonotmesis Yes Complete 1” per month None III Yes Varies * -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

Upper and Lower Extremity Nerve Conduction Studies Kelly G
2019 Upper and Lower Extremity Nerve Conduction Studies Kelly G. Gwathmey October 18, 2019 Virginia Commonwealth University 2019 Financial Disclosure I have received speaking and consulting honoraria from Alexion Pharmaceuticals. 2019 Warning Videotaping or taking pictures of the slides associated with this presentation is prohibited. The information on the slides is copyrighted and cannot be used without permission and author attribution. 2019 Outline for Today’s talk • Upper extremity nerve conduction studies o Median nerve o Ulnar nerve o Radial nerve o Median comparison studies o Medial antebrachial cutaneous nerve o Lateral antebrachial cutaneous nerve • Lower extremity nerve conduction studies o Fibular nerve o Tibial nerve o Sural nerve o Femoral nerve • Saphenous • Lateral femoral cutaneous • Phrenic nerve • Facial nerve • Anomalous Innervations 2019 Median nerve anatomy • Median nerve is formed by a combination of: o Lateral cord (C6-7) supplies the sensory fibers to the thumb, index, middle finger, proximal median forearm, and thenar eminence. o Medial cord (C8-T1) provides motor fibers to the distal forearm and hand. • The median nerve innervates the pronator teres, then gives branches to the flexor carpi radialis, flexor digitorum superficialis, and palmaris longus. • Anterior Interosseus Nerve (AIN)- innervates the flexor pollicis longus, flexor digitorum profundus (FDP) (digits 2 and 3), and pronator quadratus. Preston, David C., MD; Shapiro, Barbara E., MD, PhD. Published January 1, 2013. Pages 267-288. © 2013. 2019 Median nerve anatomy • Proximal to the wrist- the palmar cutaneous sensory branch (sensation over the thenar eminence) • Through the carpal tunnel- Motor division goes to first and second lumbricals o Recurrent thenar motor branch the thenar eminence (opponens, abductor pollicis brevis, and superficial head of flexor pollicis brevis) • Sensory branch that goes through the carpal tunnel supplies the medial thumb, index finger, middle finger and lateral half of the ring finger.