JAM3 Maintains Leukemia-Initiating Cell Self-Renewal Through LRP5/AKT/Β-Catenin/CCND1 Signaling
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

PARSANA-DISSERTATION-2020.Pdf
DECIPHERING TRANSCRIPTIONAL PATTERNS OF GENE REGULATION: A COMPUTATIONAL APPROACH by Princy Parsana A dissertation submitted to The Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland July, 2020 © 2020 Princy Parsana All rights reserved Abstract With rapid advancements in sequencing technology, we now have the ability to sequence the entire human genome, and to quantify expression of tens of thousands of genes from hundreds of individuals. This provides an extraordinary opportunity to learn phenotype relevant genomic patterns that can improve our understanding of molecular and cellular processes underlying a trait. The high dimensional nature of genomic data presents a range of computational and statistical challenges. This dissertation presents a compilation of projects that were driven by the motivation to efficiently capture gene regulatory patterns in the human transcriptome, while addressing statistical and computational challenges that accompany this data. We attempt to address two major difficulties in this domain: a) artifacts and noise in transcriptomic data, andb) limited statistical power. First, we present our work on investigating the effect of artifactual variation in gene expression data and its impact on trans-eQTL discovery. Here we performed an in-depth analysis of diverse pre-recorded covariates and latent confounders to understand their contribution to heterogeneity in gene expression measurements. Next, we discovered 673 trans-eQTLs across 16 human tissues using v6 data from the Genotype Tissue Expression (GTEx) project. Finally, we characterized two trait-associated trans-eQTLs; one in Skeletal Muscle and another in Thyroid. Second, we present a principal component based residualization method to correct gene expression measurements prior to reconstruction of co-expression networks. -

Structure and Junctional Complexes of Endothelial, Epithelial and Glial Brain Barriers
International Journal of Molecular Sciences Review Structure and Junctional Complexes of Endothelial, Epithelial and Glial Brain Barriers Mariana Castro Dias *, Josephine A. Mapunda, Mykhailo Vladymyrov and Britta Engelhardt * Theodor Kocher Institute, University of Bern, 3012 Bern, Switzerland; [email protected] (J.A.M.); [email protected] (M.V.) * Correspondence: [email protected] (M.C.D.); [email protected] (B.E.) Received: 14 October 2019; Accepted: 26 October 2019; Published: 29 October 2019 Abstract: The homeostasis of the central nervous system (CNS) is ensured by the endothelial, epithelial, mesothelial and glial brain barriers, which strictly control the passage of molecules, solutes and immune cells. While the endothelial blood-brain barrier (BBB) and the epithelial blood-cerebrospinal fluid barrier (BCSFB) have been extensively investigated, less is known about the epithelial and mesothelial arachnoid barrier and the glia limitans. Here, we summarize current knowledge of the cellular composition of the brain barriers with a specific focus on describing the molecular constituents of their junctional complexes. We propose that the brain barriers maintain CNS immune privilege by dividing the CNS into compartments that differ with regard to their role in immune surveillance of the CNS. We close by providing a brief overview on experimental tools allowing for reliable in vivo visualization of the brain barriers and their junctional complexes and thus the respective CNS compartments. Keywords: brain barriers; blood-brain barrier; neurovascular unit; blood-cerebrospinal fluid barrier; arachnoid barrier; glia limitans; tight junctions; adherens junctions 1. Introduction The brain barriers established by the endothelial blood-brain barrier (BBB), the epithelial blood-cerebrospinal fluid barrier (BCSFB), the meningeal brain barriers and the blood spinal cord barrier are essential for maintaining central nervous system (CNS) homeostasis [1]. -

1A Multiple Sclerosis Treatment
The Pharmacogenomics Journal (2012) 12, 134–146 & 2012 Macmillan Publishers Limited. All rights reserved 1470-269X/12 www.nature.com/tpj ORIGINAL ARTICLE Network analysis of transcriptional regulation in response to intramuscular interferon-b-1a multiple sclerosis treatment M Hecker1,2, RH Goertsches2,3, Interferon-b (IFN-b) is one of the major drugs for multiple sclerosis (MS) 3 2 treatment. The purpose of this study was to characterize the transcriptional C Fatum , D Koczan , effects induced by intramuscular IFN-b-1a therapy in patients with relapsing– 2 1 H-J Thiesen , R Guthke remitting form of MS. By using Affymetrix DNA microarrays, we obtained and UK Zettl3 genome-wide expression profiles of peripheral blood mononuclear cells of 24 MS patients within the first 4 weeks of IFN-b administration. We identified 1Leibniz Institute for Natural Product Research 121 genes that were significantly up- or downregulated compared with and Infection Biology—Hans-Knoell-Institute, baseline, with stronger changed expression at 1 week after start of therapy. Jena, Germany; 2University of Rostock, Institute of Immunology, Rostock, Germany and Eleven transcription factor-binding sites (TFBS) are overrepresented in the 3University of Rostock, Department of Neurology, regulatory regions of these genes, including those of IFN regulatory factors Rostock, Germany and NF-kB. We then applied TFBS-integrating least angle regression, a novel integrative algorithm for deriving gene regulatory networks from gene Correspondence: M Hecker, Leibniz Institute for Natural Product expression data and TFBS information, to reconstruct the underlying network Research and Infection Biology—Hans-Knoell- of molecular interactions. An NF-kB-centered sub-network of genes was Institute, Beutenbergstr. -

Effect of Cigarette Smoke on DNA Methylation and Lung Function
de Vries et al. Respiratory Research (2018) 19:212 https://doi.org/10.1186/s12931-018-0904-y RESEARCH Open Access From blood to lung tissue: effect of cigarette smoke on DNA methylation and lung function Maaike de Vries1,2* , Diana A van der Plaat1,2, Ivana Nedeljkovic3, Rikst Nynke Verkaik-Schakel4, Wierd Kooistra2,5, Najaf Amin3, Cornelia M van Duijn3, Corry-Anke Brandsma2,5, Cleo C van Diemen6, Judith M Vonk1,2 and H Marike Boezen1,2 Abstract Background: Genetic and environmental factors play a role in the development of COPD. The epigenome, and more specifically DNA methylation, is recognized as important link between these factors. We postulate that DNA methylation is one of the routes by which cigarette smoke influences the development of COPD. In this study, we aim to identify CpG-sites that are associated with cigarette smoke exposure and lung function levels in whole blood and validate these CpG-sites in lung tissue. Methods: The association between pack years and DNA methylation was studied genome-wide in 658 current smokers with >5 pack years using robust linear regression analysis. Using mediation analysis, we subsequently selected the CpG-sites that were also associated with lung function levels. Significant CpG-sites were validated in lung tissue with pyrosequencing and expression quantitative trait methylation (eQTM) analysis was performed to investigate the association between DNA methylation and gene expression. Results: 15 CpG-sites were significantly associated with pack years and 10 of these were additionally associated with lung function levels. We validated 5 CpG-sites in lung tissue and found several associations between DNA methylation and gene expression. -

Junctional Adhesion Molecule C (JAM3) Rabbit Polyclonal Antibody Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA339629 Junctional Adhesion Molecule C (JAM3) Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: WB Reactivity: Human Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: The immunogen for anti-JAM3 antibody: synthetic peptide directed towards the N terminal of human JAM3. Synthetic peptide located within the following region: SSNRTPVVQEFESVELSCIITDSQTSDPRIEWKKIQDEQTTYVFFDNKIQ Formulation: Liquid. Purified antibody supplied in 1x PBS buffer with 0.09% (w/v) sodium azide and 2% sucrose. Note that this product is shipped as lyophilized powder to China customers. Concentration: lot specific Purification: Affinity Purified Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 28 kDa Gene Name: junctional adhesion molecule 3 Database Link: NP_001192258 Entrez Gene 83700 Human Q9BX67 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 Junctional Adhesion Molecule C (JAM3) Rabbit Polyclonal Antibody – TA339629 Background: Tight junctions represent one mode of cell-to-cell adhesion in epithelial or endothelial cell sheets, forming continuous seals around cells and serving as a physical barrier to prevent solutes and water from passing freely through the paracellular space. JAM3, one member of the immunoglobulin superfamily, is localized in the tight junctions between high endothelial cells. Unlike other proteins in this family, this protein is unable to adhere to leukocyte cell lines and only forms weak homotypic interactions. -

Hypoxia-Induced Microrna-212/132 Alter Blood-Brain Barrier Integrity
Translational Stroke Research (2019) 10:672–683 https://doi.org/10.1007/s12975-018-0683-2 ORIGINAL ARTICLE Hypoxia-Induced MicroRNA-212/132 Alter Blood-Brain Barrier Integrity Through Inhibition of Tight Junction-Associated Proteins in Human and Mouse Brain Microvascular Endothelial Cells Malgorzata Burek1 & Anna König1 & Mareike Lang1 & Jan Fiedler2 & Sabrina Oerter3 & Norbert Roewer1 & Michael Bohnert3 & Serge C. Thal4 & Kinga G. Blecharz-Lang5 & Johannes Woitzik6 & Thomas Thum2 & Carola Y. Förster1 Received: 11 June 2018 /Revised: 26 November 2018 /Accepted: 21 December 2018 /Published online: 8 January 2019 # The Author(s) 2019 Abstract Blood-brain barrier (BBB) integrity is one of the important elements of central nervous system (CNS) homeostasis. MicroRNAs (miRs) have been demonstrated to play a role in many CNS disorders such as stroke and traumatic brain injury. MiR-212/132 are highly expressed in the CNS but their role at the BBB has not been characterized yet. Thus, we analyzed the expression of miR- 212/132 in hypoxic mouse and human brain microvascular endothelial cells (BMEC) as well as in posttraumatic mouse and human brain tissue and serum exosomes. MiR-212/132 expression was detected in brain capillaries by in situ hybridization and was increased up to ten times in hypoxic BMEC. Over-expression of pre-miR-212/132 in BMEC decreased barrier properties and reduced migration of BMEC in the wound healing assay. We identified and validated tight junction proteins claudin-1 (Cldn1), junctional adhesion molecule 3 (Jam3), and tight junction-associated protein 1 (Tjap1) as potential miR-212/132 targets. Over- expression of miRs led to a decrease in mRNA and protein expression of Cldn1, Jam3, and Tjap1, which could be rescued by a respective anti-miR. -

Regulation of Intestinal Epithelial Permeability by Tight Junctions
Cell. Mol. Life Sci. (2013) 70:631–659 DOI 10.1007/s00018-012-1070-x Cellular and Molecular Life Sciences REVIEW Regulation of intestinal epithelial permeability by tight junctions Takuya Suzuki Received: 3 April 2012 / Revised: 19 June 2012 / Accepted: 21 June 2012 / Published online: 11 July 2012 Ó Springer Basel AG 2012 Abstract The gastrointestinal epithelium forms the BT-IgSF Brain- and testis-specific immunoglobulin boundary between the body and external environment. It superfamily effectively provides a selective permeable barrier that C10 Capric acid limits the permeation of luminal noxious molecules, such C12 Lauric acid as pathogens, toxins, and antigens, while allowing the CAR Coxsacki and adenovirus receptor appropriate absorption of nutrients and water. This selec- CD Crohn’s disease tive permeable barrier is achieved by intercellular tight CHO Chinese hamster ovary junction (TJ) structures, which regulate paracellular per- CPE Clostridium perfringen enterotoxin meability. Disruption of the intestinal TJ barrier, followed DHA Docosahexaenoic acid by permeation of luminal noxious molecules, induces a DSS Dextran sodium sulfate perturbation of the mucosal immune system and inflam- ECN Escherichia coli Nissle1917 mation, and can act as a trigger for the development of EGF Epidermal growth factor intestinal and systemic diseases. In this context, much EHEC Enterohemorrhagic Escherichia coli effort has been taken to understand the roles of extracel- EPA Eicosapentaenoic acid lular factors, including cytokines, pathogens, and food EPEC Enteropathogenic Escherichia coli factors, for the regulation of the intestinal TJ barrier. Here, ERK Extracellular signal-regulated kinase I discuss the regulation of the intestinal TJ barrier together ESAM Endothelial selective adhesion molecule with its implications for the pathogenesis of diseases. -

Planell N Et Al. Supplementary Material Supplementary Table 2. Biological Pathways Analysis by IPA. Pathway Analysis Was Perform
Planell N et al. Supplementary Material Supplementary Table 2. Biological pathways analysis by IPA. Pathway analysis was performed for those genes significantly perturbed in affected colonic biopsies from UC active and UC-in-remission samples compared to non-IBD controls (Supplementary Table 2A) or in UC active involved compared to non-IBD controls (Supplementary Table 2B), using Ingenuity Pathways Analysis (Ingenuity™ Systems, www.ingenuity.com). In bold are shown those genes that were included in the real-time RT-PCR validation set. Supplementary Table 2A. Main biological functions significantly perturbed in deregulated genes in both active and inactive UC versus non-IBD controls (patterns 2 and 3 of gene expression, Figure 2). Biological functions Genes Cell communication: SERPINB5, SLC4A2, TGFB1, TGFBI, VCAM1, attachment of cells, DSG2, ICAM2, ITGA2, ITGA6, PTEN, PTGER2, cell-cell contact, disassembly of focal adhesions, TFPI2, TGFA, TGM2, VCAN, DSP, JAM2, JAM3, adhesion of connective GJA1, OCLN, PARD3, TJP1, TJP3 tissue cells, formation of tight junctions Cell death: FAS, FOXO3, GATA6, HGF, ITSN1, KLF5, LUM, cell death of epithelial cell lines, MAP3K5, MAPK14, PARP1, SERPINA1, cytotoxicity of tumor cell lines, apoptosis of endothelial cells, SERPINB5, TGFB1, THBS1, TLR3, TNFRSF10A, apoptosis of vascular TNFRSF10B, TNFRSF11B, TNFSF10, ABCG2, JUN, endothelial cells, apoptosis of microvascular MAP2K6, MET, PEA15, TCF3, TCF4, TGFA, endothelial cells TGFB1I1, TICAM1, TICAM2, TNFRSF1B, TRIM27, SMAD7, TGFBR2 ABCD3, AKAP1, AKAP2/PALM2-AKAP2, -

Thousands of Cpgs Show DNA Methylation Differences in ACPA-Positive Individuals
G C A T T A C G G C A T genes Article Thousands of CpGs Show DNA Methylation Differences in ACPA-Positive Individuals Yixiao Zeng 1,2, Kaiqiong Zhao 2,3, Kathleen Oros Klein 2, Xiaojian Shao 4, Marvin J. Fritzler 5, Marie Hudson 2,6,7, Inés Colmegna 6,8, Tomi Pastinen 9,10, Sasha Bernatsky 6,8 and Celia M. T. Greenwood 1,2,3,9,11,* 1 PhD Program in Quantitative Life Sciences, Interfaculty Studies, McGill University, Montréal, QC H3A 1E3, Canada; [email protected] 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montréal, QC H3T 1E2, Canada; [email protected] (K.Z.); [email protected] (K.O.K.); [email protected] (M.H.) 3 Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montréal, QC H3A 1A2, Canada 4 Digital Technologies Research Centre, National Research Council Canada, Ottawa, ON K1A 0R6, Canada; [email protected] 5 Cumming School of Medicine, University of Calgary, Calgary, AB T2N 1N4, Canada; [email protected] 6 Department of Medicine, McGill University, Montréal, QC H4A 3J1, Canada; [email protected] (I.C.); [email protected] (S.B.) 7 Division of Rheumatology, Jewish General Hospital, Montréal, QC H3T 1E2, Canada 8 Division of Rheumatology, McGill University, Montréal, QC H3G 1A4, Canada 9 Department of Human Genetics, McGill University, Montréal, QC H3A 0C7, Canada; [email protected] 10 Center for Pediatric Genomic Medicine, Children’s Mercy, Kansas City, MO 64108, USA 11 Gerald Bronfman Department of Oncology, McGill University, Montréal, QC H4A 3T2, Canada * Correspondence: [email protected] Citation: Zeng, Y.; Zhao, K.; Oros Abstract: High levels of anti-citrullinated protein antibodies (ACPA) are often observed prior to Klein, K.; Shao, X.; Fritzler, M.J.; Hudson, M.; Colmegna, I.; Pastinen, a diagnosis of rheumatoid arthritis (RA). -

Genome-Scale Analysis of DNA Methylation in Lung Adenocarcinoma and Integration with Mrna Expression
Downloaded from genome.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press Research Genome-scale analysis of DNA methylation in lung adenocarcinoma and integration with mRNA expression Suhaida A. Selamat,1 Brian S. Chung,1 Luc Girard,2 Wei Zhang,2 Ying Zhang,3 Mihaela Campan,1 Kimberly D. Siegmund,3 Michael N. Koss,4 Jeffrey A. Hagen,5 Wan L. Lam,6 Stephen Lam,6 Adi F. Gazdar,2 and Ite A. Laird-Offringa1,7 1Department of Surgery, Department of Biochemistry and Molecular Biology, Norris Comprehensive Cancer Center, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 2The Hamon Center for Therapeutic Oncology Research and Department of Pathology, University of Texas Southwestern Medical Center, Dallas, Texas 75390, USA; 3Department of Preventive Medicine, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 4Department of Pathology, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 5Department of Surgery, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 6BC Cancer Research Center, BC Cancer Agency, Vancouver, BC V521L3, Canada Lung cancer is the leading cause of cancer death worldwide, and adenocarcinoma is its most common histological subtype. Clinical and molecular evidence indicates that lung adenocarcinoma is a heterogeneous disease, which has important implications for treatment. Here we performed genome-scale DNA methylation profiling using the Illumina Infinium HumanMethylation27 platform on 59 matched lung adenocarcinoma/non-tumor lung pairs, with genome-scale verifi- cation on an independent set of tissues. -

Developmental Retardation Due to Paternal 5Q/11Q Translocation in a Chinese Infant: Clinical, Chromosomal and Microarray Characterization
Journal of Genetics (2019) 98:77 © Indian Academy of Sciences https://doi.org/10.1007/s12041-019-1120-3 RESEARCH ARTICLE Developmental retardation due to paternal 5q/11q translocation in a Chinese infant: clinical, chromosomal and microarray characterization XIANGYU ZHAO1 , HONGYAN XU1, CHEN ZHAO2 and LIN LI1∗ 1Department of Medical Genetics, Linyi People’s Hospital, Linyi 276003, Shandong, People’s Republic of China 2Department of Neurology, Weifang People’s Hospital, Weifang 261000, Shandong, People’s Republic of China *For correspondence. E-mail: [email protected]. Received 12 June 2018; revised 18 April 2019; accepted 19 May 2019 Abstract. Although it is known that the parental carriers of chromosomal translocation are considered to be at high risk for spontaneous abortion and embryonic death, normal gestation and delivery remain possible. This study aims to investigate the genetic factors of a Chinese infant with multiple malformations and severe postnatal development retardation. In this study, the routine cytogenetic analysis, chromosomal microarray analysis (CMA) and fluorescence in situ hybridization (FISH) analysis were performed. Conventional karyotype analyses revealed normal karyotypes of all family members. CMA of the DNA of the proband revealed a 8.3 Mb duplication of 5q35.1-qter and a 6.9 Mb deletion of 11q24.3-qter. FISH analyses verified a paternal tiny translocation between the long arm of chromosomes 5 and 11. Our investigation serves to provide important information on genetic counselling for the patient and future pregnancies in this family. Moreover, the combined use of CMA and FISH is effective for clarifying pathogenically submicroscopic copy number variants. Keywords. 5q/11q translocation; karyotyping; chromosomal microarray analysis; fluorescence in situ hybridization; growth retardation. -
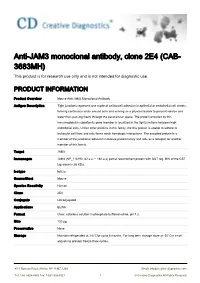
Anti-JAM3 Monoclonal Antibody, Clone 2E4 (CAB- 3683MH) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-JAM3 monoclonal antibody, clone 2E4 (CAB- 3683MH) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse Anti-JAM3 Monoclonal Antibody Antigen Description Tight junctions represent one mode of cell-to-cell adhesion in epithelial or endothelial cell sheets, forming continuous seals around cells and serving as a physical barrier to prevent solutes and water from passing freely through the paracellular space. The protein encoded by this immunoglobulin superfamily gene member is localized in the tight junctions between high endothelial cells. Unlike other proteins in this family, the this protein is unable to adhere to leukocyte cell lines and only forms weak homotypic interactions. The encoded protein is a member of the junctional adhesion molecule protein family and acts as a receptor for another member of this family. Target JAM3 Immunogen JAM3 (NP_116190, 82 a.a. ~ 180 a.a) partial recombinant protein with GST tag. MW of the GST tag alone is 26 KDa. Isotype IgG2a Source/Host Mouse Species Reactivity Human Clone 2E4 Conjugate Unconjugated Applications ELISA Format Clear, colorless solution in phosphate buffered saline, pH 7.2. Size 100 μg Preservative None Storage Maintain refrigerated at 2-8°Cfor up to 6 months. For long term storage store at -20°Cin small aliquots to prevent freeze-thaw cycles. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved GENE INFORMATION