The Sphere Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Examples of Manifolds
Examples of Manifolds Example 1 (Open Subset of IRn) Any open subset, O, of IRn is a manifold of dimension n. One possible atlas is A = (O, ϕid) , where ϕid is the identity map. That is, ϕid(x) = x. n Of course one possible choice of O is IR itself. Example 2 (The Circle) The circle S1 = (x,y) ∈ IR2 x2 + y2 = 1 is a manifold of dimension one. One possible atlas is A = {(U , ϕ ), (U , ϕ )} where 1 1 1 2 1 y U1 = S \{(−1, 0)} ϕ1(x,y) = arctan x with − π < ϕ1(x,y) <π ϕ1 1 y U2 = S \{(1, 0)} ϕ2(x,y) = arctan x with 0 < ϕ2(x,y) < 2π U1 n n n+1 2 2 Example 3 (S ) The n–sphere S = x =(x1, ··· ,xn+1) ∈ IR x1 +···+xn+1 =1 n A U , ϕ , V ,ψ i n is a manifold of dimension . One possible atlas is 1 = ( i i) ( i i) 1 ≤ ≤ +1 where, for each 1 ≤ i ≤ n + 1, n Ui = (x1, ··· ,xn+1) ∈ S xi > 0 ϕi(x1, ··· ,xn+1)=(x1, ··· ,xi−1,xi+1, ··· ,xn+1) n Vi = (x1, ··· ,xn+1) ∈ S xi < 0 ψi(x1, ··· ,xn+1)=(x1, ··· ,xi−1,xi+1, ··· ,xn+1) n So both ϕi and ψi project onto IR , viewed as the hyperplane xi = 0. Another possible atlas is n n A2 = S \{(0, ··· , 0, 1)}, ϕ , S \{(0, ··· , 0, −1)},ψ where 2x1 2xn ϕ(x , ··· ,xn ) = , ··· , 1 +1 1−xn+1 1−xn+1 2x1 2xn ψ(x , ··· ,xn ) = , ··· , 1 +1 1+xn+1 1+xn+1 are the stereographic projections from the north and south poles, respectively. -

An Introduction to Topology the Classification Theorem for Surfaces by E
An Introduction to Topology An Introduction to Topology The Classification theorem for Surfaces By E. C. Zeeman Introduction. The classification theorem is a beautiful example of geometric topology. Although it was discovered in the last century*, yet it manages to convey the spirit of present day research. The proof that we give here is elementary, and its is hoped more intuitive than that found in most textbooks, but in none the less rigorous. It is designed for readers who have never done any topology before. It is the sort of mathematics that could be taught in schools both to foster geometric intuition, and to counteract the present day alarming tendency to drop geometry. It is profound, and yet preserves a sense of fun. In Appendix 1 we explain how a deeper result can be proved if one has available the more sophisticated tools of analytic topology and algebraic topology. Examples. Before starting the theorem let us look at a few examples of surfaces. In any branch of mathematics it is always a good thing to start with examples, because they are the source of our intuition. All the following pictures are of surfaces in 3-dimensions. In example 1 by the word “sphere” we mean just the surface of the sphere, and not the inside. In fact in all the examples we mean just the surface and not the solid inside. 1. Sphere. 2. Torus (or inner tube). 3. Knotted torus. 4. Sphere with knotted torus bored through it. * Zeeman wrote this article in the mid-twentieth century. 1 An Introduction to Topology 5. -
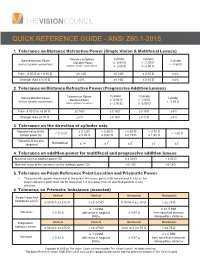
Quick Reference Guide - Ansi Z80.1-2015
QUICK REFERENCE GUIDE - ANSI Z80.1-2015 1. Tolerance on Distance Refractive Power (Single Vision & Multifocal Lenses) Cylinder Cylinder Sphere Meridian Power Tolerance on Sphere Cylinder Meridian Power ≥ 0.00 D > - 2.00 D (minus cylinder convention) > -4.50 D (minus cylinder convention) ≤ -2.00 D ≤ -4.50 D From - 6.50 D to + 6.50 D ± 0.13 D ± 0.13 D ± 0.15 D ± 4% Stronger than ± 6.50 D ± 2% ± 0.13 D ± 0.15 D ± 4% 2. Tolerance on Distance Refractive Power (Progressive Addition Lenses) Cylinder Cylinder Sphere Meridian Power Tolerance on Sphere Cylinder Meridian Power ≥ 0.00 D > - 2.00 D (minus cylinder convention) > -3.50 D (minus cylinder convention) ≤ -2.00 D ≤ -3.50 D From -8.00 D to +8.00 D ± 0.16 D ± 0.16 D ± 0.18 D ± 5% Stronger than ±8.00 D ± 2% ± 0.16 D ± 0.18 D ± 5% 3. Tolerance on the direction of cylinder axis Nominal value of the ≥ 0.12 D > 0.25 D > 0.50 D > 0.75 D < 0.12 D > 1.50 D cylinder power (D) ≤ 0.25 D ≤ 0.50 D ≤ 0.75 D ≤ 1.50 D Tolerance of the axis Not Defined ° ° ° ° ° (degrees) ± 14 ± 7 ± 5 ± 3 ± 2 4. Tolerance on addition power for multifocal and progressive addition lenses Nominal value of addition power (D) ≤ 4.00 D > 4.00 D Nominal value of the tolerance on the addition power (D) ± 0.12 D ± 0.18 D 5. Tolerance on Prism Reference Point Location and Prismatic Power • The prismatic power measured at the prism reference point shall not exceed 0.33Δ or the prism reference point shall not be more than 1.0 mm away from its specified position in any direction. -
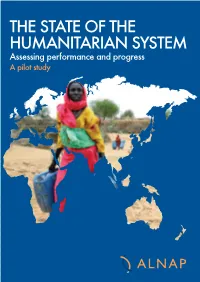
The State of the Humanitarian System Effective, and Predictable
The humanitarian system has a fundamental responsibility to continually assess its ability to save lives and alleviate human suffering. The IFRC, as a global network, shares many of the issues and challenges identified by this initiative. I welcome this report for its ambition to THE STATE OF THE assess overall achievements on a regular basis and believe it will help individual organizations and networks to reflect on and improve their own performance. We have learned from our participation in the initiative and we hope it will continue to grow and strengthen over the HUMANITARIAN SYSTEM years to come. Bekele Geleta, Secretary General of the IFRC Assessing performance and progress I warmly welcome this first State of the Humanitarian System report because it shows deep A pilot study commitment towards self improvement within the humanitarian system. I encourage this effort to be sustained over time so that it can gradually live up to its potential to further improve the quality of services provided by all humanitarian actors. The ICRC remains committed to lead its own self improvement and to contribute to that of the humanitarian system as a whole. Angelo Gnaedinger, Director General of the ICRC Thanks to the collective efforts by members of the humanitarian community over the past five years, the humanitarian system has made significant strides in becoming increasingly rapid, SYSTEM HUMANITARIAN THE OF STATE THE effective, and predictable. That said, much more still needs to be done. ALNAP’s first State of the Humanitarian System report is unique in its scope and well researched. Findings such as these will contribute to the humanitarian community’s collective efforts to take stock of where we stand, face up to global challenges, and to decide how we can make more difference to the lives of people affected by emergencies. -
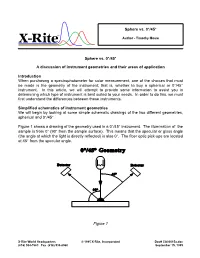
Sphere Vs. 0°/45° a Discussion of Instrument Geometries And
Sphere vs. 0°/45° ® Author - Timothy Mouw Sphere vs. 0°/45° A discussion of instrument geometries and their areas of application Introduction When purchasing a spectrophotometer for color measurement, one of the choices that must be made is the geometry of the instrument; that is, whether to buy a spherical or 0°/45° instrument. In this article, we will attempt to provide some information to assist you in determining which type of instrument is best suited to your needs. In order to do this, we must first understand the differences between these instruments. Simplified schematics of instrument geometries We will begin by looking at some simple schematic drawings of the two different geometries, spherical and 0°/45°. Figure 1 shows a drawing of the geometry used in a 0°/45° instrument. The illumination of the sample is from 0° (90° from the sample surface). This means that the specular or gloss angle (the angle at which the light is directly reflected) is also 0°. The fiber optic pick-ups are located at 45° from the specular angle. Figure 1 X-Rite World Headquarters © 1995 X-Rite, Incorporated Doc# CA00015a.doc (616) 534-7663 Fax (616) 534-8960 September 15, 1995 Figure 2 shows a drawing of the geometry used in an 8° diffuse sphere instrument. The sphere wall is lined with a highly reflective white substance and the light source is located on the rear of the sphere wall. A baffle prevents the light source from directly illuminating the sample, thus providing diffuse illumination. The sample is viewed at 8° from perpendicular which means that the specular or gloss angle is also 8° from perpendicular. -

UNHCR Handbook for Emergencies Emergencies
Handbook for UNHCR Handbook for Emergencies Emergencies United Nations High Commissioner for Refugees Case postale 2500 CH-1211 Genève 2 Dépôt Third Edition Comments on the Handbook for Emergencies and requests for additional Copies should be addressed to: The Emergency Preparedness and Response Section UNHCR Headquarters Case Postale 2500 CH – 1211 Genève 2 Dépôt Switzerland Téléphone: + 41 22 739 83 01 Fax: + 41 22 739 73 01 Email: [email protected] Handbook for Emergencies © United Nations High Commissioner for Refugees, Geneva Third Edition February, 2007 ISBN This document is issued by the Office of the United Nations High Commissioner for Refugees for general distribution. All rights are reserved. Reproduction is authorized, except for commercial purposes, provided UNHCR is acknowledged. I Using the Handbook II Chapters may be located quickly by using the key on the contents page. Particular subjects may be located by using the index. The handbook is structured as follows: Section One summarizes UNHCR’s mandate of international protecdtion and the aim and principles of emergency response; Section Two deals with emergency management; Section Three covers the vital sectors and problem areas in refugee emergencies, including health, food, sanitation and water, as well as key field activities underpinning the operations such as logistics, community services and registration. The chapters in this section start with a summary so that readers, who might not need the full level of detail in each of these chapters, can understand the basic -
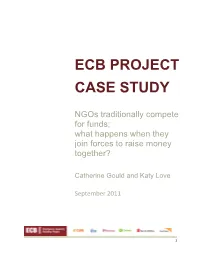
Ecb Project Case Study
ECB PROJECT CASE STUDY NGOs traditionally compete for funds; what happens when they join forces to raise money together? Catherine Gould and Katy Love September 2011 1 The big NGOs traditionally compete for funds; what happens when they join forces to raise money together? 1. Six NGOs began with $5 million in the bank; and $7 million still to find… CARE International, Catholic Relief Services (CRS), Mercy Corps, Oxfam, Save the Children, and World Vision International have come together in a unique collaboration to build field, agency, and sector level emergency preparedness and response capacity. The Emergency Capacity Building (ECB) Project aims to improve the speed, quality, and effectiveness of the humanitarian community in saving lives, improving welfare, and protecting the rights of people in emergency situations. In 2008, following a first phase of the ECB Project, the Bill and Melinda Gates Foundation accepted a proposal from the six NGOs worth $12.3 million for a further five‐year joint programme. Stepping outside their traditional grantmaking strategy to support this innovative project, the Gates Foundation provided $5 million of core funding and the agencies pledged to fundraise together the remaining $7.3 million. While CARE USA manages the contract with the Gates Foundation, the other five agencies signed a memorandum of understanding (MOU) outlining the project’s management structure and ways of working for the five‐year joint venture. This case study recounts the agencies’ attempts to together close the $7.3 million funding gap, while launching and sustaining a $12 million programme. Three years in, the ECB Project is almost fully funded, but it has not always been a smooth journey… 2. -
Simulations in the Humanitarian Sector; the ECB Simulation Initiative
Simulations in the humanitarian sector; the ECB Simulation Initiative Connections UK 4th September 2013 www.ecbproject.org What is the ECB Project? _________________________________________________________________ • The Emergency Capacity Building Project •5 year collaboration amongst six of the worlds largest international non-governmental organisations •Improve the speed, quality and effectiveness of emergency response through targeted staff capacity building initiatives (national level) •Phase II runs from 2008 - 2013 What is capacity building? _________________________________________________________________ • An individual skill or organisational improvement process such as; -A self guided learning process -Training, workshops, meetings or seminars -Coaching or mentoring -Undertaking (and acting on) evaluations / AARs -Joint actions -Recruiting more staff -Simulations How do simulations build capacity? _________________________________________________________________ • Simulations provide an excellent opportunity to -Build relationships, -Test individual competencies -Provide a safe learning space for participants to try out new behaviours or approaches -Lead to organisational or individual improvements •Simulations provide staff a safe space to succeed (and fail) Why do we need to build capacity? _________________________________________________________________ •Disasters are increasing in frequency and intensity (Feinstein Centre and UNEP) •UN estimates by 2025, 50% of the worlds population will live in disaster prone locations -

Recognizing Surfaces
RECOGNIZING SURFACES Ivo Nikolov and Alexandru I. Suciu Mathematics Department College of Arts and Sciences Northeastern University Abstract The subject of this poster is the interplay between the topology and the combinatorics of surfaces. The main problem of Topology is to classify spaces up to continuous deformations, known as homeomorphisms. Under certain conditions, topological invariants that capture qualitative and quantitative properties of spaces lead to the enumeration of homeomorphism types. Surfaces are some of the simplest, yet most interesting topological objects. The poster focuses on the main topological invariants of two-dimensional manifolds—orientability, number of boundary components, genus, and Euler characteristic—and how these invariants solve the classification problem for compact surfaces. The poster introduces a Java applet that was written in Fall, 1998 as a class project for a Topology I course. It implements an algorithm that determines the homeomorphism type of a closed surface from a combinatorial description as a polygon with edges identified in pairs. The input for the applet is a string of integers, encoding the edge identifications. The output of the applet consists of three topological invariants that completely classify the resulting surface. Topology of Surfaces Topology is the abstraction of certain geometrical ideas, such as continuity and closeness. Roughly speaking, topol- ogy is the exploration of manifolds, and of the properties that remain invariant under continuous, invertible transforma- tions, known as homeomorphisms. The basic problem is to classify manifolds according to homeomorphism type. In higher dimensions, this is an impossible task, but, in low di- mensions, it can be done. Surfaces are some of the simplest, yet most interesting topological objects. -

The Real Projective Spaces in Homotopy Type Theory
The real projective spaces in homotopy type theory Ulrik Buchholtz Egbert Rijke Technische Universität Darmstadt Carnegie Mellon University Email: [email protected] Email: [email protected] Abstract—Homotopy type theory is a version of Martin- topology and homotopy theory developed in homotopy Löf type theory taking advantage of its homotopical models. type theory (homotopy groups, including the fundamen- In particular, we can use and construct objects of homotopy tal group of the circle, the Hopf fibration, the Freuden- theory and reason about them using higher inductive types. In this article, we construct the real projective spaces, key thal suspension theorem and the van Kampen theorem, players in homotopy theory, as certain higher inductive types for example). Here we give an elementary construction in homotopy type theory. The classical definition of RPn, in homotopy type theory of the real projective spaces as the quotient space identifying antipodal points of the RPn and we develop some of their basic properties. n-sphere, does not translate directly to homotopy type theory. R n In classical homotopy theory the real projective space Instead, we define P by induction on n simultaneously n with its tautological bundle of 2-element sets. As the base RP is either defined as the space of lines through the + case, we take RP−1 to be the empty type. In the inductive origin in Rn 1 or as the quotient by the antipodal action step, we take RPn+1 to be the mapping cone of the projection of the 2-element group on the sphere Sn [4]. -

The Sphere Packing Problem in Dimension 8 Arxiv:1603.04246V2
The sphere packing problem in dimension 8 Maryna S. Viazovska April 5, 2017 8 In this paper we prove that no packing of unit balls in Euclidean space R has density greater than that of the E8-lattice packing. Keywords: Sphere packing, Modular forms, Fourier analysis AMS subject classification: 52C17, 11F03, 11F30 1 Introduction The sphere packing constant measures which portion of d-dimensional Euclidean space d can be covered by non-overlapping unit balls. More precisely, let R be the Euclidean d vector space equipped with distance k · k and Lebesgue measure Vol(·). For x 2 R and d r 2 R>0 we denote by Bd(x; r) the open ball in R with center x and radius r. Let d X ⊂ R be a discrete set of points such that kx − yk ≥ 2 for any distinct x; y 2 X. Then the union [ P = Bd(x; 1) x2X d is a sphere packing. If X is a lattice in R then we say that P is a lattice sphere packing. The finite density of a packing P is defined as Vol(P\ Bd(0; r)) ∆P (r) := ; r > 0: Vol(Bd(0; r)) We define the density of a packing P as the limit superior ∆P := lim sup ∆P (r): r!1 arXiv:1603.04246v2 [math.NT] 4 Apr 2017 The number be want to know is the supremum over all possible packing densities ∆d := sup ∆P ; d P⊂R sphere packing 1 called the sphere packing constant. For which dimensions do we know the exact value of ∆d? Trivially, in dimension 1 we have ∆1 = 1. -

Hyperbolic Geometry
Flavors of Geometry MSRI Publications Volume 31,1997 Hyperbolic Geometry JAMES W. CANNON, WILLIAM J. FLOYD, RICHARD KENYON, AND WALTER R. PARRY Contents 1. Introduction 59 2. The Origins of Hyperbolic Geometry 60 3. Why Call it Hyperbolic Geometry? 63 4. Understanding the One-Dimensional Case 65 5. Generalizing to Higher Dimensions 67 6. Rudiments of Riemannian Geometry 68 7. Five Models of Hyperbolic Space 69 8. Stereographic Projection 72 9. Geodesics 77 10. Isometries and Distances in the Hyperboloid Model 80 11. The Space at Infinity 84 12. The Geometric Classification of Isometries 84 13. Curious Facts about Hyperbolic Space 86 14. The Sixth Model 95 15. Why Study Hyperbolic Geometry? 98 16. When Does a Manifold Have a Hyperbolic Structure? 103 17. How to Get Analytic Coordinates at Infinity? 106 References 108 Index 110 1. Introduction Hyperbolic geometry was created in the first half of the nineteenth century in the midst of attempts to understand Euclid’s axiomatic basis for geometry. It is one type of non-Euclidean geometry, that is, a geometry that discards one of Euclid’s axioms. Einstein and Minkowski found in non-Euclidean geometry a This work was supported in part by The Geometry Center, University of Minnesota, an STC funded by NSF, DOE, and Minnesota Technology, Inc., by the Mathematical Sciences Research Institute, and by NSF research grants. 59 60 J. W. CANNON, W. J. FLOYD, R. KENYON, AND W. R. PARRY geometric basis for the understanding of physical time and space. In the early part of the twentieth century every serious student of mathematics and physics studied non-Euclidean geometry.