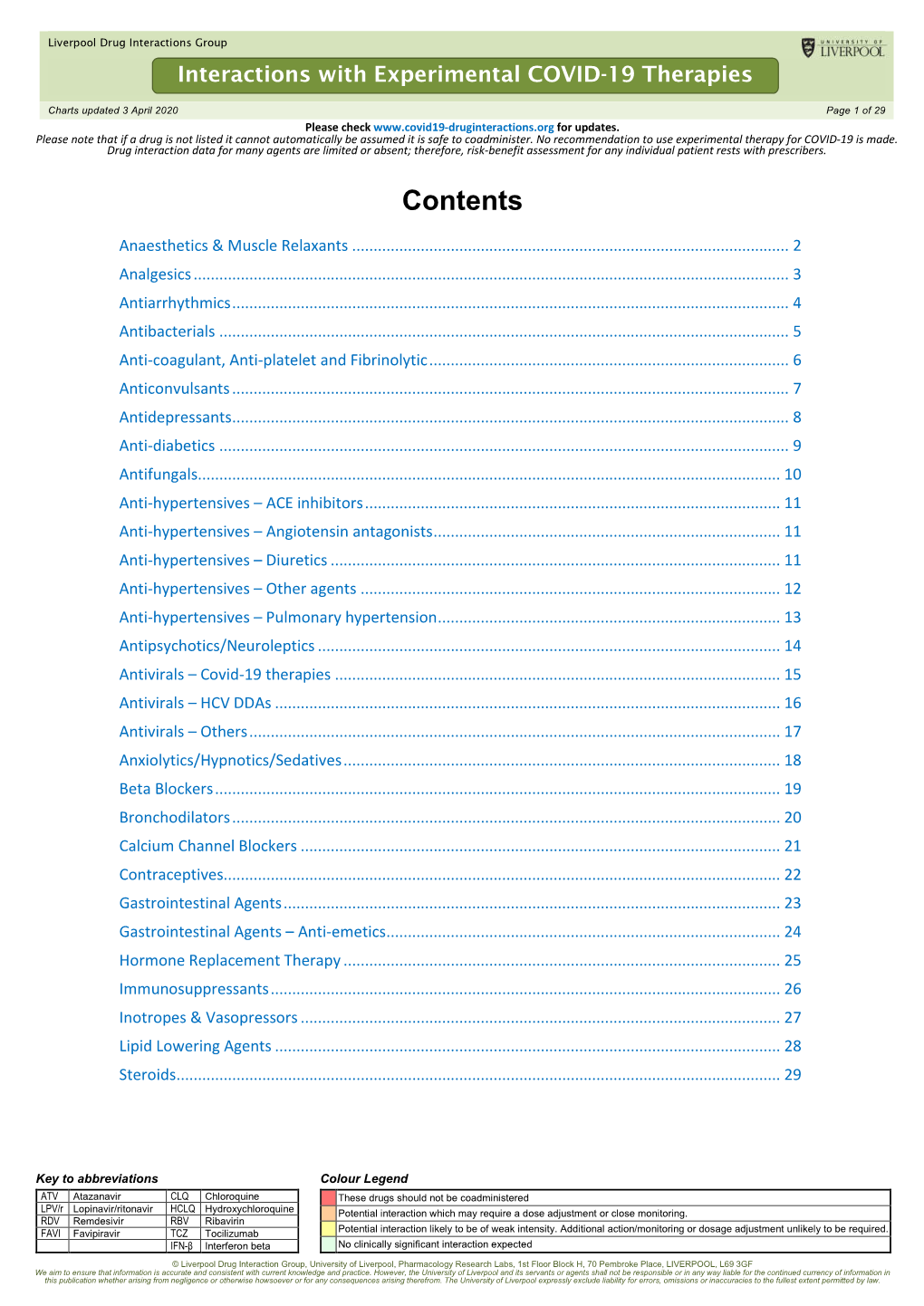
Interactions with Experimental COVID-19 Therapies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quarterly Review
Tropical Gastroenterology 2008.29;4:187–193 Quarterly Have hematopoietic growth factors made an Review impact on the management of liver disease? Pankaj Tyagi and Kaushal Madan ABSTRACT Department of Gastroenterology, It is clear that the major indication for the use of hematopoietic growth factors in hepatology GB Pant Hospital & Department of is to counteract the adverse effects of interferons (neutropenia and thrombocytopenia) and Medical Hepatology, ribavirin (hemolytic anaemia) during the treatment of hepatitis C infection. This is important Institute of Liver and Biliary Sciences, because the probability of SVR depends on proper adherence to therapy (at least 80% of the New Delhi requisite dose maintained for at least 80% of the requisite duration) and proper adherence can only be achieved if the side effects are reduced to a minimum. Even though the studies Correspondence: Dr. Kaushal Madan have demonstrated beyond doubt that the use of hematopoietic growth factors does indeed Email: [email protected] reduce the incidence and severity of these adverse effects and helps the patients to complete the course of therapy, the data on improvement of SVR is still limited. There is only one study of darbepoetin and filgrastim showing the beneficial effect on SVR. Even among the hematological side effects, possibly the only significant effect which limits the use of optimal HCV therapy is the hemolytic anaemia induced by ribavirin. The other two main side effects, i.e. neutropenia and thrombocytopenia are not clinically problematic. The use of such growth factors would be particularly effective if patients who have advanced liver disease or cirrhosis are able to receive adequate anti-viral therapy as has been demonstrated in the study of eltrombopag among HCV cirrhotics. -

Antipsychotics and Seizures: Higher Risk with Atypicals?
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Seizure 22 (2013) 141–143 Contents lists available at SciVerse ScienceDirect Seizure jou rnal homepage: www.elsevier.com/locate/yseiz Short communication Antipsychotics and seizures: Higher risk with atypicals? a, b c d e Unax Lertxundi *, Rafael Hernandez , Juan Medrano , Saioa Domingo-Echaburu , Monserrat Garcı´a , e Carmelo Aguirre a Pharmacy Service, Red de Salud Mental de Araba, C/alava 43, 01006 Vitoria-Gasteiz, Alava, Spain b Internal Medicine Service, Red de Salud Mental de Araba, Spain c Psychiatry Service, Red de Salud Mental de Araba, Spain d Pharmacy Service, OSI Alto Deba, Spain e Basque Pharmacovigilance Unit, Hospital de Galdakao-Usa´nsolo, Spain A R T I C L E I N F O A B S T R A C T Article history: Purpose: Almost all antipsychotics have been associated with a risk of epileptic seizure provocation. Received 29 May 2012 Among the first-generation antipsychotics (FGA) chlorpromazine appears to be associated with the Received in revised form 17 October 2012 greatest risk of seizures among the second-generation antipsychotics (SGA) clozapine is thought to be Accepted 18 October 2012 most likely to cause convulsions. This information is largely based on studies that are not sufficiently controlled. Besides, information about the seizure risk associated with newer antipsychotics is scarce. Keywords: Method: The Pharmacovigilance Unit of the Basque Country (network of centers of the Spanish Antipsychotics Pharmacovigilance System, SEFV) provided reporting data for adverse reactions (AR) from the whole Seizures SEFV to estimate the reporting odds ratio (ROR) for antipsychotics and seizures (‘‘convulsions’’ as Single Pharmacovigilance MedDra Query). -

Management of Chronic Problems
MANAGEMENT OF CHRONIC PROBLEMS INTERACTIONS BETWEEN ALCOHOL AND DRUGS A. Leary,* T. MacDonald† SUMMARY concerned. Alcohol may alter the effects of the drug; drug In western society alcohol consumption is common as is may change the effects of alcohol; or both may occur. the use of therapeutic drugs. It is not surprising therefore The interaction between alcohol and drug may be that concomitant use of these should occur frequently. The pharmacokinetic, with altered absorption, metabolism or consequences of this combination vary with the dose of elimination of the drug, alcohol or both.2 Alcohol may drug, the amount of alcohol taken, the mode of affect drug pharmacokinetics by altering gastric emptying administration and the pharmacological effects of the drug or liver metabolism. Drugs may affect alcohol kinetics by concerned. Interactions may be pharmacokinetic or altering gastric emptying or inhibiting gastric alcohol pharmacodynamic, and while coincidental use of alcohol dehydrogenase (ADH).3 This may lead to altered tissue may affect the metabolism or action of a drug, a drug may concentrations of one or both agents, with resultant toxicity. equally affect the metabolism or action of alcohol. Alcohol- The results of concomitant use may also be principally drug interactions may differ with acute and chronic alcohol pharmacodynamic, with combined alcohol and drug effects ingestion, particularly where toxicity is due to a metabolite occurring at the receptor level without important changes rather than the parent drug. There is both inter- and intra- in plasma concentration of either. Some interactions have individual variation in the response to concomitant drug both kinetic and dynamic components and, where this is and alcohol use. -

Sofosbuvir/Ledipasvir for HIV •
Hepatitis C: Drugs and Combinations Melissa Osborn MD Associate Professor MetroHealth Medical Center Case Western Reserve University Cleveland, OH Faculty and Planning Committee Disclosures Please consult your program book. Off-Label Disclosure The following off-label/investigational uses will be discussed in this presentation: • Sofosbuvir/ledipasvir for HIV •. Investigational agents for hepatitis C will be mentioned – Asunaprevir – Daclatasvir – Beclabuvir – Grazoprevir – Elbasvir – GS-5816 Learning Objectives Upon completion of this presentation, learners should be better able to: • apply clinical trial data on new hepatitis C therapies to their patient population. • select which new hepatitis C therapies are appropriate to use with common antiretrovirals. Evolution of interferon-based therapy in HCV-monoinfected genotype 1 patients Sustained Virologic Response 100% 90% 80% 80% 75% 67% 60% 42% 46% 40% 28% 20% 7% 0% Std interferon-alfa IFN + RBV Peg-alfa-2b+RBV Peg-alfa-2a +RBV P/R/Telaprevir P/R/Boceprevir P/R/Simeprevir P/R/Sofosbuvir McHutchison, NEJM 1998; 339: 1485-92 Jacobson, NEJM 2011; 364:2405-16 Fried, NEJM 2002; 347: 975-82 Poordad, NEJM 2011; 364: 1195-206 Manns, Lancet 2001; 358:958-65 Jacobson, AASLD 2013 #1122 Lawitz, NEJM 2013 Evolution of HCV Therapy: Genotype 1 Patients Naïve to Therapy: HIV-HCV coinfection Sustained Virologic Response 80% 75% 74% 67% 61% 60% 46% 42% 40% 28% 29% 20% 17% 7% 7% 0% Std interferon-alfa IFN + RBV Peg-alfa-2b+RBV Peg-alfa-2a +RBV P/R/Telaprevir P/R/Boceprevir Torriani, NEJM, 2004 351:438-50 -

Hepatitis C Agents Therapeutic Class Review
Hepatitis C Agents Therapeutic Class Review (TCR) November 2, 2018 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. Proprietary Information. Restricted Access – Do not disseminate or copy without approval. © 2004–2018 Magellan Rx Management. All Rights Reserved. FDA-APPROVED INDICATIONS Drug Mfr FDA-Approved Indications Interferons peginterferon alfa-2a Genentech Chronic hepatitis C (CHC) 1 (Pegasys®) . -

Managing Adverse Effects and Complications in Completing Treatment for Hepatitis C Virus Infection
HCV Treatment Complications Volume 20 Issue 4 October/November 2012 Perspective Managing Adverse Effects and Complications in Completing Treatment for Hepatitis C Virus Infection The addition of direct-acting antivirals (DAAs) to hepatitis C virus (HCV) Psychiatric Complications treatment regimens has made treatment more effective and patient Depression is the most common psy- management more complex. Shepherding patients through a full course of chiatric complication encountered in HCV therapy requires motivation and involvement on the part of the patient HCV patients, with mild to moderate and the physician. Indeed, physician inexperience and lack of confidence in depression found in as much as 80% of guiding patients through the challenges of treatment appears to be a primary patients. Bipolar disorder and schizo- reason for early discontinuation of therapy. Among the many complications phrenia are also not infrequently en- of HCV treatment that must be managed efficiently and effectively are countered. depression and other psychiatric disorders; hematologic abnormalities There is little evidence to support including DAA- and ribavirin-associated anemia and peginterferon alfa- a benefit of preemptive antidepres- associated neutropenia and thrombocytopenia; rash and drug eruptions, sant therapy in all patients undergo- including telaprevir-associated rash; and weight loss. Practical considerations ing HCV treatment, though a recent in management of these common complications are offered. This article randomized trial of HCV patients -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

Comparative Efficacy and Safety of Antipsychotic Drugs for Tic Disorders: a Systematic Review and Bayesian Network Meta-Analysis
Published online: 2018-03-05 Review Thieme Yang Chunsong et al. Comparative Efficacy and Safety … Phar- macopsychiatry 2017; 00: 00–00 Comparative Efficacy and Safety of Antipsychotic Drugs for Tic Disorders: A Systematic Review and Bayesian Network Meta-Analysis Authors Chunsong Yang1,2 * , Zilong Hao3 * , Ling-Li Zhang1,2, Cai-Rong Zhu4, Ping Zhu4, Qin Guo5 Affiliations Supporting Information for this article is available 1 Department of Pharmacy, Evidence-Based Pharmacy online at http:// doi.org/10.1055/s-0043-124872 Center, West China Second Hospital, Sichuan University 2 Key Laboratory of Birth Defects and Related Diseases of ABSTracT Women and Children (Sichuan University), Ministry of Objective The purpose of this study was to evaluate the ef- Education ficacy and safety of antipsychotic drugs for tic disorders (TDs) 3 Department of Neurology, West China Hospital, Sichuan in a network meta-analysis. University, Chengdu, China Methods PubMed, Embase, Cochrane Library, and 4 Chinese 4 West China School of Public Health, Sichuan University databases were searched. Randomized controlled trials (RCTs) 5 Department of Pediatrics, West China Second Hospital, evaluating the efficacy of antipsychotic drugs for TDs were in- Sichuan University cluded. Results Sixty RCTs were included. In terms of tic symptom Key words score, compared with placebo, haloperidol, risperidone, ari- tic disorder, antipsychotic drug, systematic review, network piprazole, quetiapine, olanzapine, and ziprasidone can sig- meta-analysis nificantly improve tic symptom score (standardized mean received 02.09.2017 differences [SMD] ranged from − 12.32 to − 3.20). Quetiapine revised 04.12.2017 was superior to haloperidol, pimozide, risperidone, tiapride, accepted 10.12.2017 aripiprazole, and penfluridol for improving tic symptom score (SMD ranged from − 28.24 to − 7.59). -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -
THE HARD TRUTH ABOUT PROKINETIC MEDICATION USE in PETS Introduction Pathophysiology/Etiology to That Observed in Dogs
VETTALK Volume 15, Number 04 American College of Veterinary Pharmacists THE HARD TRUTH ABOUT PROKINETIC MEDICATION USE IN PETS Introduction Pathophysiology/Etiology to that observed in dogs. It can be The moving topic of this Vet Talk As with most diseases in the veteri- due to a trichobezoar, dehydration, newsletter will be prokinetic medica- nary world, the etiology and patho- obesity, old age, diabetes, immobility, tions. The availability of information physiology of constipation are varied pain from trauma to the low back, on the many prokinetic agents is var- depending on the species being dis- bladder infection, or an anal sac infec- ied at best so an overall consensus of cussed, where in their gastrointestinal tion. In cases that are more chronic, prokinetic medications will be as- tract the problem is occurring, and underlying disease such as colitis or sessed in this article, hopefully giving any accompanying comorbid condi- Irritable Bowel Syndrome (IBS) may better insight to practitioners about tions. be the culprit. On the other hand, the which agents to use in their patients. cause may be idiopathic which is Canines: In man’s best friend, consti- frustrating for both veterinarian and Prevalence pation has many origins. A dog’s patient since this form is most diffi- Chronic constipation and gastroin- digestive tract itself is complex but cult to treat. testinal stasis are highly debilitating ultimately the mass movements and conditions that not only affect human haustral contractions from the large Equines: Despite their large size, patients but our four legged patients intestine (colon), propel feces into the horses have incredibly delicate diges- as well! Though this condition is rectum stimulating the internal anal tive systems.