Appendicitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IRRITABLE BOWEL SYNDROME by Michael Sperling MD
IRRITABLE BOWEL SYNDROME By Michael Sperling MD Irritable bowel syndrome (IBS) involves vague symptoms of abdominal pain, diarrhea, constipation, gas and bloating for which there is no understandable cause. Incredibly, IBS affects up to 20% of the population but only three- quarters of those people actually seek medical attention. It is the second most common reason for work absenteeism. Irritable bowel symptoms may also be related to other complaints such as belching, heartburn, swallowing problems, fullness after eating, nausea, frequent urination, painful menstruation and pain during intercourse. Extremely severe cases can sometimes be related to a history of traumatic abuse. Some common associations or factors: Michael Sperling, MD 1. ‘Spastic colon’ is frequently found along with irritable bowel syndrome. Spastic colon consists of painful muscle contractions which can be relieved by bulk agents or anti- spasm drugs. 2. Post-infectious IBS occurs when irritable bowel follows a gastrointestinal infection, such as the stomach flu. These recurrent symptoms can last up to two years. 3. Stress and anxiety can worsen IBS symptoms so occasionally anti-anxiety agents may be helpful. 4. Food intolerances classically worsen symptoms of irritable bowel in some people. Common “offending foods” include lactose, legumes (beans) and cruciferous vegetables like brussel sprouts, cauliflower, broccoli and cabbage. 5. Hypersensitivity of the bowel wall: Normal colon activity is not usually noticed however in “visceral hypersensitivity”, the bowel wall reacts painfully to normal activity. This condition may be helped by the use of low dose antidepressants, which can block these painful stimuli. Careful and selective testing of patients with these symptoms and the development of a long-term doctor/patient relationship is the key to diagnosing and managing these symptoms. -

Print This Article
International Surgery Journal Lew D et al. Int Surg J. 2021 May;8(5):1575-1578 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: https://dx.doi.org/10.18203/2349-2902.isj20211831 Case Report Acute gangrenous appendicitis and acute gangrenous cholecystitis in a pregnant patient, a difficult diagnosis: a case report David Lew, Jane Tian*, Martine A. Louis, Darshak Shah Department of Surgery, Flushing Hospital Medical Center, Flushing, New York, USA Received: 26 February 2021 Accepted: 02 April 2021 *Correspondence: Dr. Jane Tian, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Abdominal pain is a common complaint in pregnancy, especially given the physiological and anatomical changes that occur as the pregnancy progresses. The diagnosis and treatment of common surgical pathologies can therefore be difficult and limited by the special considerations for the fetus. While uncommon in the general population, concurrent or subsequent disease processes should be considered in the pregnant patient. We present the case of a 36 year old, 13 weeks pregnant female who presented with both acute appendicitis and acute cholecystitis. Keywords: Appendicitis, Cholecystitis, Pregnancy, Pregnant INTRODUCTION population is rare.5 Here we report a case of concurrent appendicitis and cholecystitis in a pregnant woman. General surgeons are often called to evaluate patients with abdominal pain. The differential diagnosis list must CASE REPORT be expanded in pregnant woman and the approach to diagnosing and treating certain diseases must also be A 36 year old, 13 weeks pregnant female (G2P1001) adjusted to prevent harm to the fetus. -

Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement
CLINICAL REPORT Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement ÃEdwin F. de Zoeten, zBrad A. Pasternak, §Peter Mattei, ÃRobert E. Kramer, and yHoward A. Kader ABSTRACT disease. The first description connecting regional enteritis with Inflammatory bowel disease is a chronic inflammatory disorder of the perianal disease was by Bissell et al in 1934 (2), and since that time gastrointestinal tract that includes both Crohn disease (CD) and ulcerative perianal disease has become a recognized entity and an important colitis. Abdominal pain, rectal bleeding, diarrhea, and weight loss consideration in the diagnosis and treatment of CD. Perianal characterize both CD and ulcerative colitis. The incidence of IBD in the Crohn disease (PCD) is defined as inflammation at or near the United States is 70 to 150 cases per 100,000 individuals and, as with other anus, including tags, fissures, fistulae, abscesses, or stenosis. autoimmune diseases, is on the rise. CD can affect any part of the The symptoms of PCD include pain, itching, bleeding, purulent gastrointestinal tract from the mouth to the anus and frequently will include discharge, and incontinence of stool. perianal disease. The first description connecting regional enteritis with perianal disease was by Bissell et al in 1934, and since that time perianal INCIDENCE AND NATURAL HISTORY disease has become a recognized entity and an important consideration in the Limited pediatric data describe the incidence and prevalence diagnosis and treatment of CD. Perianal Crohn disease (PCD) is defined as of PCD. The incidence of PCD in the pediatric age group has been inflammation at or near the anus, including tags, fissures, fistulae, abscesses, estimated to be between 13.6% and 62% (3). -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

ACUTE Yellow Atrophy Ofthe Liver Is a Rare Disease; Ac
ACUTE YELLOW ATROPHY OF THE LIVER AS A SEQUELA TO APPENDECTOMY.' BY MAX BALLIN, M.D., OF DETROIT, MICHIGAN. ACUTE yellow atrophy of the liver is a rare disease; ac- cording to Osler about 250 cases are on record. This affection is also called Icterus gravis, Fatal icterus, Pernicious jaundice, Acute diffuse hepatitis, Hepatic insufficiency, etc. Acute yellow atrophy of the liver is characterized by a more or less sudden onset of icterus increasing to the severest form, headaches. insomnia, violent delirium, spasms, and coma. There are often cutaneous and mucous hiemorrhages. The temperature is usually high and irregular. The pulse, first normal, later rapid; urine contains bile pigments, albumen, casts, and products of incomplete metabolism of albumen, leucin, and tyrosin, the pres- ence of which is considered pathognomonic. The affection ends mostly fatally, but there are recoveries on record. The findings of the post-mortem are: liver reduced in size; cut surface mot- tled yellow, sometimes with red spots (red atrophy), the paren- chyma softened and friable; microscopically the liver shows biliary infiltration, cells in all stages of degeneration. Further, we find parenchymatous nephritis, large spleen, degeneration of muscles, haemorrhages in mucous and serous membranes. The etiology of this affection is not quite clear. We find the same changes in phosphorus poisoning; many believe it to be of toxic origin, but others consider it to be of an infectious nature; and we have even findings of specific germs (Klebs, Tomkins), of streptococci (Nepveu), staphylococci (Bourdil- lier), and also the Bacillus coli is found (Mintz) in the affected organs. The disease seems to occur always secondary to some other ailment, and is observed mostly during pregnancy (about one-third of all cases, hence the predominance in women), after Read before the Wayne County Medical Society, January 5, I903. -
The Abnormal Presentation of Complicated Appendicitis Goubeaux C* and Adams J Removed
Open Access Journal of Family Medicine Case Report The Abnormal Presentation of Complicated Appendicitis Goubeaux C* and Adams J removed. Heritage College of Osteopathic Medicine, Ohio University, Dublin, OH 43016, USA Discussion *Corresponding author: Craig Goubeaux, Heritage Acute appendicitis is one of the most common pathologies in College of Osteopathic Medicine, Ohio University, Dublin, medicine with more than 250,000 cases reported per year [5]. The OH 43016, USA lifetime prevalence is reported to be between 7-8% [5,7]. Diagnosis is Received: January 31, 2019; Accepted: March 12, typically based on a careful clinical history and physical examination 2019; Published: March 19, 2019 [1.7]. The signs and symptoms classically associated with appendicitis are periumbilical pain initially that migrates to right lower quadrant, The Case rebound tenderness, low-grade fever, anorexia, and elevated white A 60-year-old white male presented to our family practice with a blood cell count. chief complaint of isolated right upper quadrant (RUQ) abdominal There are pathologies that may mimic appendicitis such as an pain. It began one week prior after suspected food poisoning with anomalous congenital band, Meckel’s diverticulitis, spontaneous one episode of vomiting. The pain was a constant, dull ache ranging urinary extravasation, renal artery thrombosis or renal infarction between 1-5/10. It did not limit his activities as a farmer. He used [3]. Additionally, a mobile cecum is a congenital anomaly that may NSAIDs to help with the pain. During the past week all other review of systems were negative. Vitals signs were within normal lead to abnormal presentation of appendicitis which occurs in about limits. -

The Differences Between ICD-9 and ICD-10
Preparing for the ICD-10 Code Set: Fact Sheet 2 October 1, 2015 Compliance Date Get the Facts to be Compliant Alert: The new ICD-10 compliance date is October 1, 2015. The Differences Between ICD-9 and ICD-10 This is the second fact sheet in a series and is focused on the differences between the ICD-9 and ICD-10 code sets. Collectively, the fact sheets will provide information, guidance, and checklists to assist you with understanding what you need to do to implement the ICD-10 code set. The ICD-10 code sets are not a simple update of the ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and concepts that make them very different from ICD-9. Because of these differences, it is important to develop a preliminary understanding of the changes from ICD-9 to ICD-10. This basic understanding of the differences will then identify more detailed training that will be needed to appropriately use the ICD-10 code sets. In addition, seeing the differences between the code sets will raise awareness of the complexities of converting to the ICD-10 codes. Overall Comparisons of ICD-9 to ICD-10 Issues today with the ICD-9 diagnosis and procedure code sets are addressed in ICD-10. One concern today with ICD-9 is the lack of specificity of the information conveyed in the codes. For example, if a patient is seen for treatment of a burn on the right arm, the ICD-9 diagnosis code does not distinguish that the burn is on the right arm. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Stomach Flu (Viral Gastroenteritis)
Stomach Flu (Viral Gastroenteritis) The stomach flu (also called viral gastroenteritis) is caused by a virus (rotavirus, adenovirus, Norwalk virus to name a few) that affect the stomach and small intestines. It may come on suddenly or over the course of a few hours. The illness is usually brief, lasting 24-72 hours. Symptoms include: Nausea Vomiting Stomach cramps Diarrhea Mild fever Fatigue Body Chills/Sweats Loss of appetite Muscle aches To help take care of yourself: • The best thing to do is to let your stomach rest from solid foods. • Sip on clear liquids (Hi-C, apple, cranberry, and grape juices, Jell-O, Gatorade- type liquids and ginger-ale or ginger tea). There are special properties in ginger that help soothe the stomach. It is extremely important to keep up your hydration. Water is great for hydration but Gatorade-type products are better because they will restore your electrolytes (Sodium, Potassium and Chloride) which are essential for body functions. You may "stir" the bubbles out of the soda if the carbonation is harsh on your stomach. • Once you have not vomited for a few hours and your stomach is feeling better, you may start to eat solid foods. You may try crackers, plain noodles, eggs, broth, pretzels and yogurt. • The BRAT diet (Bananas, Rice, Applesauce & Toast) includes foods that are low in fiber and are easily digested. • Stay away from dairy products, citric (including orange and grapefruit juices), tomato-based & spicy foods. • SLOWLY increase your dietary intake to include fruits, vegetables and meat once symptoms are gone (usually over 2-3 days). -
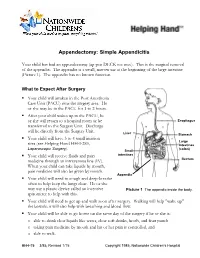
Appendectomy: Simple Appendicitis
Appendectomy: Simple Appendicitis Your child has had an appendectomy (ap pen DECK toe mee). This is the surgical removal of the appendix. The appendix is a small, narrow sac at the beginning of the large intestine (Picture 1). The appendix has no known function. What to Expect After Surgery . Your child will awaken in the Post Anesthesia Care Unit (PACU) near the surgery area. He or she may be in the PACU for 1 to 2 hours. After your child wakes up in the PACU, he or she will return to a hospital room or be Esophagus transferred to the Surgery Unit. Discharge will be directly from the Surgery Unit. Liver Stomach . Your child will have 3 to 4 small incision Large sites (see Helping Hand HH-I-283, Intestines Laparoscopic Surgery (colon) ). Small . Your child will receive fluids and pain intestines medicine through an intravenous line (IV). Rectum When your child can take liquids by mouth, pain medicine will also be given by mouth. Appendix . Your child will need to cough and deep-breathe often to help keep the lungs clear. He or she may use a plastic device called an incentive Picture 1 The appendix inside the body. spirometer to help with this. Your child will need to get up and walk soon after surgery. Walking will help "wake up" the bowels; it will also help with breathing and blood flow. Your child will be able to go home on the same day of the surgery if he or she is: o able to drink clear liquids like water, clear soft drinks, broth, and fruit punch o taking pain medicine by mouth and his or her pain is controlled, and o able to walk. -

Descriptive Study Regarding the Etiological Factors Responsible for Secondary Bacterial Peritonitis in Patients Admitted in a Te
International Journal of Health Sciences and Research Vol.10; Issue: 7; July 2020 Website: www.ijhsr.org Original Research Article ISSN: 2249-9571 Descriptive Study Regarding the Etiological Factors Responsible for Secondary Bacterial Peritonitis in Patients Admitted in a Tertiary Care Hospital in Trans Himalayan Region Raj Kumar1, Rahul Gupta2, Anjali Sharma3, Rajesh Chaudhary4 1MS General Surgery, Civil Hospital Baijnath, Himachal Pradesh 2MD Community Medicine, District Programme Officer, Health and Family Welfare, Himachal Pradesh 3Resident Doctor, Department of Microbiology, DRPGMC Kangra at Tanda, Himachal Pradesh 4MS General Surgery, Civil Hospital Nagrota Bagwan, Himachal Pradesh Corresponding Author: Rahul Gupta ABSTRACT Peritonitis is an inflammation of the peritoneum. Primary peritonitis which is spontaneous bacterial peritonitis, Secondary peritonitis due to infection from intraabdominal source or spillage of its contents and Tertiary peritonitis which is recurrent or reactivation of secondary peritonitis. The present study was aimed to determine the etiology of generalized secondary peritonitis among the patients admitted in Department of General Surgery, Dr RPGMC Kangra at Tanda. This descriptive observational study was conducted in the department of surgery Dr. Rajendra Prasad Government Medical College Kangra at Tanda consisting of patients having acute generalised secondary peritonitis presented in emergency department or Surgery outdoor patient department over a period of one year from December 2016 through November 2017. The most common etiology of generalized secondary peritonitis in our patients was peptic ulcer disease (77.13%) followed by perforated appendicitis (9.8%). Etiological factors of secondary generalised peritonitis have a different pattern in different geographical regions. Peptic ulcer disease remains the commonest etiology of secondary peritonitis in India followed by enteric perforation which is in contrast to the western studies where appendicular and colon perforations are more common.