Case Report: a Patient with Severe Peritonitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Audit on Management of Hematemesis in Children Admitted to Pediatric Gastroenterology and Hepatology Unit of Assiut
Med. J. Cairo Univ., Vol. 86, No. 8, December: 4531-4536, 2018 www.medicaljournalofcairouniversity.net Clinical Audit on Management of Hematemesis in Children Admitted to Pediatric Gastroenterology and Hepatology Unit of Assiut University Children Hospital ESRAA T. AHMED, M.Sc.; FATMA A. ALI, M.D. and NAGLA H. ABU FADDAN, M.D. The Department of Pediatrics, Faculty of Medicine, Assiut University, Assiut, Egypt Abstract Hematemesis: Indicates that the bleeding origin is above the Treitz angle, i.e., that it constitutes an Background: Hematemesis is an uncommon but potentially Upper Gastrointestinal Bleeding (UGIB) [3] . serious and life-threatening clinical condition in children. It indicates that the bleeding origin is above the Treitz angle, The etiology of upper GI bleeding varies by i.e., that it constitutes an Upper Gastrointestinal Bleeding (UGIB). age. The pathophysiology of upper GI bleeding is related to the source of the bleeding. Most clinically Aim of Study: To assess for how much the adopted proto- significant causes of upper GI bleeds are associated cols of management of children with upper gastrointestinal bleeding were applied at Gastroenterology & Hepatology Unit with ulcers, erosive esophagitis, gastritis, varices, of Assiut University Children Hospital. and/or Mallory-Weiss tears. While Physiologic Patients and Methods: This study is a an audit on man- stress, NSAIDs such as aspirin and ibuprofen, and agement of children with upper gastrointestinal bleeding infection with Helicobacter pylori are few of the admitted to pediatric Gastroenterology and Hepatology Unit, factors contributing to the imbalance leading to Assiut University Children Hospital during the period from ulcers and erosions in the GI tract [4] . -

Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement
CLINICAL REPORT Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement ÃEdwin F. de Zoeten, zBrad A. Pasternak, §Peter Mattei, ÃRobert E. Kramer, and yHoward A. Kader ABSTRACT disease. The first description connecting regional enteritis with Inflammatory bowel disease is a chronic inflammatory disorder of the perianal disease was by Bissell et al in 1934 (2), and since that time gastrointestinal tract that includes both Crohn disease (CD) and ulcerative perianal disease has become a recognized entity and an important colitis. Abdominal pain, rectal bleeding, diarrhea, and weight loss consideration in the diagnosis and treatment of CD. Perianal characterize both CD and ulcerative colitis. The incidence of IBD in the Crohn disease (PCD) is defined as inflammation at or near the United States is 70 to 150 cases per 100,000 individuals and, as with other anus, including tags, fissures, fistulae, abscesses, or stenosis. autoimmune diseases, is on the rise. CD can affect any part of the The symptoms of PCD include pain, itching, bleeding, purulent gastrointestinal tract from the mouth to the anus and frequently will include discharge, and incontinence of stool. perianal disease. The first description connecting regional enteritis with perianal disease was by Bissell et al in 1934, and since that time perianal INCIDENCE AND NATURAL HISTORY disease has become a recognized entity and an important consideration in the Limited pediatric data describe the incidence and prevalence diagnosis and treatment of CD. Perianal Crohn disease (PCD) is defined as of PCD. The incidence of PCD in the pediatric age group has been inflammation at or near the anus, including tags, fissures, fistulae, abscesses, estimated to be between 13.6% and 62% (3). -

Acute Pancreatitis Associated with Rotavirus Infection and Review Of
Case Report/Olgu Sunumu İstanbul Med J 2020; 21(1): 78-81 DO I: 10.4274/imj.galenos.2020.88319 Acute Pancreatitis Associated with Rotavirus Infection and Review of The Literature Rotavirüs Enfeksiyonuna Bağlı Akut Pankreatit Olguları ve Literatürün Gözden Geçirilmesi Kamil Şahin, Güzide Doğan University of Health Sciences, Haseki Training and Research Hospital, Department of Pediatrics, İstanbul, Turkey ABSTRACT ÖZ Agents causing acute gastroenteritis are not common causes of Çocuklarda pankreatit etiyolojisinde akut gastroenterit etkenleri pancreatitis etiology in children. Pancreatitis associated with sık görülen sebeplerden değildir. Rotavirüs enfeksiyonuna rotavirus infection is very rare. Cases with acute pancreatitis bağlı görülen pankreatit ise oldukça nadirdir. Rotavirüs during rotavirus gastroenteritis are reported due to rare gastroenteriti sırasında akut pankreatit gelişen olgular, associations. In this article, the causes of acute pancreatitis rotavirüs enfeksiyonuna bağlı akut pankreatitin nadir olması and cases of acute pancreatitis due to rotavirus infection were nedeniyle sunulmuştur. Bu yazıda, akut pankreatit sebepleri ve investigated. Clinical findings were mild, and complications rotavirüse bağlı gelişen akut pankreatit olguları incelenmiştir. were not observed in both of our patients, including a two- İki yaş kız ve üç yaşındaki erkek iki olgumuzda ve literatürde year-old female and a three-year-old male, and other cases değerlendirilen diğer olgularda klinik bulgular hafif seyretmiş, evaluated in the literature. The -

Hemosuccus Pancreaticus: a Rare Cause of Upper Gastrointestinal Bleeding During Pregnancy Rani Akhil Bhat,1 Vani Ramkumar,1 K
Hemosuccus Pancreaticus: A Rare Cause Of Upper Gastrointestinal Bleeding During Pregnancy Rani Akhil Bhat,1 Vani Ramkumar,1 K. Akhil Krishnanand Bhat, 2 Rajgopal Shenoy2 Abstract Upper gastrointestinal bleeding is most commonly caused by From the 1Department of Department of Obstetrics and Gynaecology, Oman Medical 2 lesions in the esophagus, stomach or duodenum. Bleeding which College, Sohar, Sultanate of Oman, Department of Surgery, Oman Medical College, Sohar, Sultanate of Oma. originates from the pancreatic duct is known as hemosuccus pancreaticus. Only a few scattered case reports of hemosuccus Received: 06 Nov 2009 pancreaticus during pregnancy have been recorded in literature. Accepted: 31 Dec 2009 This is a case of a primigravida with 37 weeks of gestation Address correspondence and reprint request to: Dr. Rani A. Bhat,Department of with hemosuccus pancreaticus and silent chronic pancreatitis. Obstetrics and Gynaecology, Oman Medical College, P. O. Box 391, P. C. 321, Al- Evaluating pregnant women with upper gastrointestinal Tareef, Sohar, Sultanate of Oman. bleeding differs from that of non pregnant women as diagnostic E-mail: [email protected] modalities using radiation cannot be used. Therefore, Esophagogastroduodenoscopy should be performed at the time of active bleeding to diagnose hemosuccus pancreaticus. Bhat RA, et al. OMJ. 25 (2010); doi:10.5001/omj.2010.21 Introduction examination showed a combination of dark red blood and melena. Laboratory investigations revealed hemoglobin of 6.3 grams/dL, Hemosuccus pancreaticus is the term used to describe the liver function tests, serum amylase, glucose and prothrombin time syndrome of gastrointestinal bleeding into the pancreatic duct were within the normal range. -

Descriptive Study Regarding the Etiological Factors Responsible for Secondary Bacterial Peritonitis in Patients Admitted in a Te
International Journal of Health Sciences and Research Vol.10; Issue: 7; July 2020 Website: www.ijhsr.org Original Research Article ISSN: 2249-9571 Descriptive Study Regarding the Etiological Factors Responsible for Secondary Bacterial Peritonitis in Patients Admitted in a Tertiary Care Hospital in Trans Himalayan Region Raj Kumar1, Rahul Gupta2, Anjali Sharma3, Rajesh Chaudhary4 1MS General Surgery, Civil Hospital Baijnath, Himachal Pradesh 2MD Community Medicine, District Programme Officer, Health and Family Welfare, Himachal Pradesh 3Resident Doctor, Department of Microbiology, DRPGMC Kangra at Tanda, Himachal Pradesh 4MS General Surgery, Civil Hospital Nagrota Bagwan, Himachal Pradesh Corresponding Author: Rahul Gupta ABSTRACT Peritonitis is an inflammation of the peritoneum. Primary peritonitis which is spontaneous bacterial peritonitis, Secondary peritonitis due to infection from intraabdominal source or spillage of its contents and Tertiary peritonitis which is recurrent or reactivation of secondary peritonitis. The present study was aimed to determine the etiology of generalized secondary peritonitis among the patients admitted in Department of General Surgery, Dr RPGMC Kangra at Tanda. This descriptive observational study was conducted in the department of surgery Dr. Rajendra Prasad Government Medical College Kangra at Tanda consisting of patients having acute generalised secondary peritonitis presented in emergency department or Surgery outdoor patient department over a period of one year from December 2016 through November 2017. The most common etiology of generalized secondary peritonitis in our patients was peptic ulcer disease (77.13%) followed by perforated appendicitis (9.8%). Etiological factors of secondary generalised peritonitis have a different pattern in different geographical regions. Peptic ulcer disease remains the commonest etiology of secondary peritonitis in India followed by enteric perforation which is in contrast to the western studies where appendicular and colon perforations are more common. -

Treatment Recommendations for Feline Pancreatitis
Treatment recommendations for feline pancreatitis Background is recommended. Fentanyl transdermal patches have become Pancreatitis is an elusive disease in cats and consequently has popular for pain relief because they provide a longer duration of been underdiagnosed. This is owing to several factors. Cats with analgesia. It takes at least 6 hours to achieve adequate fentanyl pancreatitis present with vague signs of illness, including lethargy, levels for pain control; therefore, one recommended protocol is to decreased appetite, dehydration, and weight loss. Physical administer another analgesic, such as intravenous buprenorphine, examination and routine laboratory findings are nonspecific, and at the time the fentanyl patch is placed. The cat is then monitored until recently, there have been limited diagnostic tools available closely to see if additional pain medication is required. Cats with to the practitioner for noninvasively diagnosing pancreatitis. As a chronic pancreatitis may also benefit from pain management, and consequence of the difficulty in diagnosing the disease, therapy options for outpatient treatment include a fentanyl patch, sublingual options are not well understood. buprenorphine, oral butorphanol, or tramadol. Now available, the SNAP® fPL™ and Spec fPL® tests can help rule Antiemetic therapy in or rule out pancreatitis in cats presenting with nonspecific signs Vomiting, a hallmark of pancreatitis in dogs, may be absent or of illness. As our understanding of this disease improves, new intermittent in cats. When present, vomiting should be controlled; specific treatment modalities may emerge. For now, the focus is and if absent, treatment with an antiemetic should still be on managing cats with this disease, and we now have the tools considered to treat nausea. -
PERFORATED PEPTIC ULCER. Patient Usually Experiences
Postgrad Med J: first published as 10.1136/pgmj.12.134.470 on 1 December 1936. Downloaded from 470 POST-GRADUATE MEDICAL JOURNAL December, 1936 PERFORATED PEPTIC ULCER. By RONALD W. RAVEN, F.R.C.S. (Assistant Surgeon to T'he French Hospital, Assistant Surgeon to The Gordon Hospital for Rectal Diseases and Swrgical Registrar to The Royal Cancer Hospital.) INTRODUCTION. Peptic ulceration is a crippling disease judged from the stand-point of morbidity, and is also dangerous to life on account of serious complications, such as haemorrhage or perforation which may supervene during the course of the disease. These complications may occur in any patient and there are no criteria which will indicate whether or not an ulcer will bleed or perforate. When the treatment of peptic ulceration is under review it must be remembered that from 20 to 30 per cent. of these ulcers perforate. In a large series of cases I found that the incidence of perforation was 27 per cent. It is thus essential that patients suffering with peptic ulcer should be kept under continuous careful observation. Unfortunately, however, a small percentage of patients give no previous history of the peptic ulcer syndrome and perforation of the ulcer is the first indication of its presence. Recently, when considering the role of surgery in the treatment of chronic peptic ulcer, Joll stated that there has been a rise in the incidence of perforation as a complication of peptic ulcer since medical treatment has become systematized in the treatment of this disease. It must also be remembered that medical treat- Protected by copyright. -

Esophageal Varices
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Hindawi Publishing Corporation Case Reports in Critical Care Volume 2016, Article ID 2370109, 4 pages http://dx.doi.org/10.1155/2016/2370109 Case Report A Rare but Reversible Cause of Hematemesis: (Downhill) Esophageal Varices Lam-Phuong Nguyen,1,2,3 Narin Sriratanaviriyakul,1,2,3 and Christian Sandrock1,2,3 1 Division of Pulmonary, Critical Care, and Sleep Medicine, University of California, Davis, Suite #3400, 4150 V Street, Sacramento, CA 95817, USA 2Department of Internal Medicine, University of California, Davis, Sacramento, USA 3VA Northern California Health Care System, Mather, USA Correspondence should be addressed to Lam-Phuong Nguyen; [email protected] Received 12 December 2015; Accepted 1 February 2016 Academic Editor: Kurt Lenz Copyright © 2016 Lam-Phuong Nguyen et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. “Downhill” varices are a rare cause of acute upper gastrointestinal bleeding and are generally due to obstruction of the superior vena cava (SVC). Often these cases of “downhill” varices are missed diagnoses as portal hypertension but fail to improve with medical treatment to reduce portal pressure. We report a similar case where recurrent variceal bleeding was initially diagnosed as portal hypertension but later found to have SVC thrombosis presenting with recurrent hematemesis. A 39-year-old female with history of end-stage renal disease presented with recurrent hematemesis. Esophagogastroduodenoscopy (EGD) revealed multiple varices. -

Digestive Tract Tuberculosis
World Gastroenterology Organisation Global Guidelines Digestive tract tuberculosis March 2021 WGO Review Team Mohamed Tahiri (Chair, Morocco), K.L. Goh (Co-Chair, Malaysia), Zaigham Abbas (Pakistan), David Epstein (South Africa), Chen Min-Hu (China), Chris Mulder (Netherlands), Amarender Puri (India), Michael Schultz (New Zealand), Anton LeMair (Netherlands) Funding and conflict of interest statement All of the authors have stated that there were no conflicts of interest in relation to their authorship of this paper. Anton LeMair acts as guideline development consultant for WGO. WGO Global Guidelines Digestive tract tuberculosis 2 Contents 1 Introduction .............................................................................................................................. 4 1.1 About WGO cascades ................................................................................................................. 5 1.2 Definitions .................................................................................................................................. 5 1.3 Epidemiology .............................................................................................................................. 6 1.3.1 WHO 2018 global tuberculosis report .............................................................................. 6 1.4 Etiopathogenesis and risk factors .............................................................................................. 7 2 Clinical features ....................................................................................................................... -

Research Article Nonalcoholic Fatty Liver Disease Aggravated the Severity of Acute Pancreatitis in Patients
Hindawi BioMed Research International Volume 2019, Article ID 9583790, 7 pages https://doi.org/10.1155/2019/9583790 Research Article Nonalcoholic Fatty Liver Disease Aggravated the Severity of Acute Pancreatitis in Patients Dacheng Wu,1 Min Zhang,1 Songxin Xu,1 Keyan Wu,1 Ningzhi Wang,1 Yuanzhi Wang,1 Jian Wu,1 Guotao Lu ,1 Weijuan Gong,1,2 Yanbing Ding ,1 and Weiming Xiao 1 Department of Gastroenterology, Affiliated Hospital of Yangzhou University, Yangzhou University, No. Hanjiang Media Road, Yangzhou ,Jiangsu,China Department of Immunology, School of Medicine, Yangzhou University, Yangzhou, China Correspondence should be addressed to Yanbing Ding; [email protected] and Weiming Xiao; [email protected] Received 17 October 2018; Accepted 3 January 2019; Published 22 January 2019 Guest Editor: Marina Berenguer Copyright © 2019 Dacheng Wu et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background and Aim. Te incidence of nonalcoholic fatty liver disease (NAFLD) as a metabolic disease is increasing annually. In the present study, we aimed to explore the infuence of NAFLD on the severity of acute pancreatitis (AP). Methods.Teseverity of AP was diagnosed and analyzed according to the 2012 revised Atlanta Classifcation. Outcome variables, including the severity of AP, organ failure (all types of organ failure), and systemic infammatory response syndrome (SIRS), were compared for patients with and without NAFLD. Results. Six hundred and ffy-six patients were enrolled in the study and were divided into two groups according to the presence or absence of NAFLD. -

A Case Series on Intussusceptions in Infants Presenting with Listlessness
ABDOMINAL CONDITIONS © 2010 SNL All rights reserved A case series on intussusceptions in infants presenting with listlessness Intussusception is characterised by abdominal pain, vomiting and blood in stools. However, in younger infants it may present with non-classical symptoms such as listlessness, pallor, decreased feeding, and being non-specifically unwell. Three cases of intussusception in young infants who presented with being listless and had some or no features to suggest a clinical diagnosis of intussusception are described which are designed to highlight the non-classical features of intussusception likely to be encountered in very young infants. Siba P. Paul1 ntussusception is one of the most tachycardia and prolonged capillary refill MBBS, DCH Icommon surgical emergencies time he was given a fluid bolus of 20mL/kg Paediatric Trust Registrar encountered in infancy and early with 0.9% sodium chloride. He was [email protected] childhood. This is a condition where the intermittently responding to his parents proximal segment of the bowel telescopes but was not irritable. His cardiovascular 1 David C. A. Candy into the distal segment causing and respiratory examination was MBBS, MSc, MD, FRCP, FRCPCH, FCU obstruction1. The classic triad of symptoms otherwise normal. Consultant Paediatric Gastroenterologist consists of abdominal pain, vomiting and He was distressed by an abdominal blood in stools1. It is often seen in children Nikila Pandya2 examination and was found to be drawing aged four months to two years, with a peak up his legs and crying while being MD, DCH, FRCPCH incidence during four to nine months of Consultant Paediatrician examined. The provisional diagnosis at age2. -
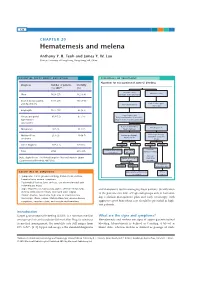
Hematemesis and Melena Chapter
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients.