Tenecteplase II-04
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
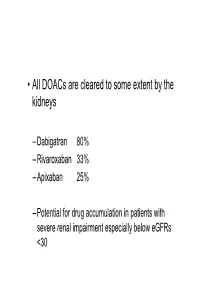
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Anticoagulation Reversal Guideline for Adults
Anticoagulation Reversal Guideline for Adults Antithrombotic reversal strategies should be limited to clinical situations (i.e. life-threatening bleeding) where the immediate need for anticoagulant reversal outweighs the risk of thrombosis (either from the reversal agent itself or normalization of coagulation in a patient with underlying thromboembolic risk). These recommendations are meant to serve as general guidelines and should not replace clinical judgment. Always seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible. This document is not meant to guide selection of patients for reversal therapies. Please refer to appropriate national guidelines to aide decision- making regarding need for reversal, if warranted. 1. ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants 2. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine All indications for anticoagulation are considered, including atrial fibrillation, venous thromboembolism, prosthetic cardiac valves, and intracardiac thrombus. Mechanical circulatory support devices, including temporary or permanent ventricular assist devices (i.e. LVADs), are excluded from this document. Whenever possible, anticoagulation should be resumed in a timely manner to avoid thromboembolic complications related to the underlying indication for anticoagulation. This guideline does not provide recommendations on resuming anticoagulation. References: • Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Experts Consensus Decisions Pathways. J Am Coll Cardiol. -

Predicting Potential Drugs for Breast Cancer Based on Mirna and Tissue Specificity
Int. J. Biol. Sci. 2018, Vol. 14 971 Ivyspring International Publisher International Journal of Biological Sciences 2018; 14(8): 971-982. doi: 10.7150/ijbs.23350 Research Paper Predicting Potential Drugs for Breast Cancer based on miRNA and Tissue Specificity Liang Yu, Jin Zhao and Lin Gao School of Computer Science and Technology, Xidian University, Xi'an, 710071, P.R. China. Corresponding author: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2017.10.16; Accepted: 2017.12.14; Published: 2018.05.22 Abstract Network-based computational method, with the emphasis on biomolecular interactions and biological data integration, has succeeded in drug development and created new directions, such as drug repositioning and drug combination. Drug repositioning, that is finding new uses for existing drugs to treat more patients, offers time, cost and efficiency benefits in drug development, especially when in silico techniques are used. MicroRNAs (miRNAs) play important roles in multiple biological processes and have attracted much scientific attention recently. Moreover, cumulative studies demonstrate that the mature miRNAs as well as their precursors can be targeted by small molecular drugs. At the same time, human diseases result from the disordered interplay of tissue- and cell lineage-specific processes. However, few computational researches predict drug-disease potential relationships based on miRNA data and tissue specificity. Therefore, based on miRNA data and the tissue specificity of diseases, we propose a new method named as miTS to predict the potential treatments for diseases. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set
Form Title ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Form Number CH-0454 © 2018, Alberta Health Services, CKCM This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The license does not apply to content for which the Alberta Health Services is not the copyright owner. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/ Disclaimer: This material is intended for use by clinicians only and is provided on an DVLVZKHUHLVEDVLV$OWKRXJKUHDVRQDEOHHIIRUWVZHUHPDGHWRFRQ¿UPWKHDFFXUDF\RIWKH information, Alberta Health Services does not make any representation or warranty, express, LPSOLHGRUVWDWXWRU\DVWRWKHDFFXUDF\UHOLDELOLW\FRPSOHWHQHVVDSSOLFDELOLW\RU¿WQHVVIRU a particular purpose of such information. This material is not a substitute for the advice of a TXDOL¿HGKHDOWKSURIHVVLRQDO$OEHUWD+HDOWK6HUYLFHVH[SUHVVO\GLVFODLPVDOOOLDELOLW\IRUWKHXVH of these materials, and for any claims, actions, demands or suits arising from such use. Patient label placed here (if applicable) or if labels are not + used, minimum information below is required + Last Name First Name Birthdate (yyyy-Mon-dd) Gender PHN # ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Phone Number Date Time Initial (yyyy-Mon-dd) (hh:mm) 1. Patient Treatment & Monitoring Complete 12 lead ECG Stat if not already completed. Review with Physician. Take initial vital signs (Temp, HR, RR, SpO2, BP both arms) Repeat vital signs with any chest pain or equivalent symptoms. Initiate intravenous (IV) and infuse 0.9% sodium chloride at 30mL/hour (left arm preferred) Provide oxygen to keep SpO2 greater than or equal to 90% or with clinical signs of hypoxemia. Give acetylsalicylic acid 160 mg orally now, chewed or swallowed OR acetylsalicylic acid 160 mg orally administered pre-arrival (Time _______). -

Use of Antithrombotic Medications in the Presence of Neuraxial Anesthesia
Guideline: Use of Antithrombotic Medications In The Presence of Neuraxial Anesthesia Use of Antithrombotic Medications In The Presence of Neuraxial Anesthesia Purpose of Guidelines: To establish appropriate administration and timing of antithrombotic medications before, during, and after the use of neuraxial anesthesia to minimize the risk of bleeding. Definitions: Neuraxial Anesthesia = Delivery of anesthetic medication requiring placement of catheters or needles into the epidural or spinal space Antithrombotic Medications = Anticoagulant, antiplatelet, and thrombolytic medications Background1-3: Spinal (or epidural) hematomas are a rare but catastrophic complication of neuraxial anesthesia. The risk of hematoma development is increased in the presence of antithrombotic medication. Patients undergoing neuraxial anesthesia must have the risks of bleeding from neuraxial interventions balanced with the underlying and ongoing risk of thromboembolism necessitating anticoagulation. Recommendations for the management of specific antithrombotics in patients undergoing neuraxial anesthesia are provided in the following Tables: o Table 1. Management of Intravenous and Subcutaneous Anticoagulation Therapy in Patients Undergoing Neuraxial Anesthesia o Table 2. Management of ORAL Anticoagulation Therapy in Patients Undergoing Neuraxial Anesthesia o Table 3. Management of ORAL and Intravenous Antiplatelet and Thrombolytic Therapy in Patients Undergoing Neuraxial Anesthesia Workflow if a Contradicted Medication is Prescribed: Providers will have -

Tnkase® (Tenecteplase)
TNKase® (Tenecteplase) DESCRIPTION TNKase® (Tenecteplase) is a tissue plasminogen activator (tPA) produced by recombinant DNA technology using an established mammalian cell line (Chinese Hamster Ovary cells). Tenecteplase is a 527 amino acid glycoprotein developed by introducing the following modifications to the complementary DNA (cDNA) for natural human tPA: a substitution of threonine 103 with asparagine, and a substitution of asparagine 117 with glutamine, both within the kringle 1 domain, and a tetra-alanine substitution at amino acids 296–299 in the protease domain. TNKase is a sterile, white to off-white, lyophilized powder for single intravenous (IV) bolus administration after reconstitution with Sterile Water for Injection (SWFI), USP. Each vial of TNKase nominally contains 52.5 mg Tenecteplase, 0.55 g L-arginine, 0.17 g phosphoric acid, and 4.3 mg polysorbate 20, which includes a 5% overfill. Each vial will deliver 50 mg of Tenecteplase. CLINICAL PHARMACOLOGY General Tenecteplase is a modified form of human tissue plasminogen activator (tPA) that binds to fibrin and converts plasminogen to plasmin. In the presence of fibrin, in vitro studies demonstrate that Tenecteplase conversion of plasminogen to plasmin is increased relative to its conversion in the absence of fibrin. This fibrin specificity decreases systemic activation of plasminogen and the resulting degradation of circulating fibrinogen as compared to a molecule lacking this property. Following administration of 30, 40, or 50 mg of TNKase, there are decreases in circulating fibrinogen (4%–15%) and plasminogen (11%−24%). The clinical significance of fibrin- specificity on safety (e.g., bleeding) or efficacy has not been established. Biological potency is determined by an in vitro clot lysis assay and is expressed in Tenecteplase-specific units. -

Tenecteplase - Drugbank
10/30/2018 Tenecteplase - DrugBank Tenecteplase Targets (11) Biointeractions (1) IDENTIFICATION Name Tenecteplase Accession Number DB00031 (BTD00019, BIOD00019) Type Biotech Groups Approved Biologic Classification Protein Based Therapies Thrombolytic agents Description Tissue plasminogen activator (tPA). Tenecteplase is a 527 amino acid glycoprotein developed by introducing the following modifications to the complementary DNA (cDNA) for natural human tPA: a substitution of threonine 103 with asparagine, and a substitution of asparagine 117 with glutamine, both within the kringle 1 domain, and a tetra-alanine substitution at amino acids 296- 299 in the protease domain. Protein structure https://www.drugbank.ca/drugs/DB00031 1/23 10/30/2018 Tenecteplase - DrugBank Protein chemical formula C2561H3919N747O781S40 Protein average weight 58951.2 Da Sequences >DB00031 sequence SYQVICRDEKTQMIYQQHQSWLRPVLRSNRVEYCWCNSGRAQCHSVPVKSCSEPRCFNGG TCQQALYFSDFVCQCPEGFAGKCCEIDTRATCYEDQGISYRGNWSTAESGAECTNWQSSA LAQKPYSGRRPDAIRLGLGNHNYCRNPDRDSKPWCYVFKAGKYSSEFCSTPACSEGNSDC YFGNGSAYRGTHSLTESGASCLPWNSMILIGKVYTAQNPSAQALGLGKHNYCRNPDGDAK PWCHVLKNRRLTWEYCDVPSCSTCGLRQYSQPQFRIKGGLFADIASHPWQAAIFAAAAAS PGERFLCGGILISSCWILSAAHCFQERFPPHHLTVILGRTYRVVPGEEEQKFEVEKYIVH KEFDDDTYDNDIALLQLKSDSSRCAQESSVVRTVCLPPADLQLPDWTECELSGYGKHEAL SPFYSERLKEAHVRLYPSSRCTSQHLLNRTVTDNMLCAGDTRSGGPQANLHDACQGDSGG PLVCLNDGRMTLVGIISWGLGCGQKDVPGVYTKVTNYLDWIRDNMRP Download FASTA Format Synonyms TNK-tPA Prescription Products Search MARKETING MARKETING NAME ↑↓ DOSAGE ↑↓ STRENGTH ↑↓ ROUTE ↑↓ LABELLER ↑↓ START -

Metalyse, INN-Tenecteplase
SCIENTIFIC DISCUSSION This module reflects the initial scientific discussion and scientific discussion on procedures, which have been finalised before 1 February 2004. For scientific information on procedures after this date please refer to module 8B. 1. Introduction Metalyse is a new thrombolytic agent containing the active substance tenecteplase (TNK tPA). It is intended for fibrinolytic treatment in the acute phase of myocardial infarction, and should be administered as an intravenous bolus over approximately 10 seconds in a weight-adjusted dose range from 30 to 50 mg. The clinical benefits of fibrinolytic therapy in patients with acute myocardial infarction (AMI) are well documented, and a close correlation between early treatment and survival is established. The rationale for the development of TNK-tPA was to find a fibrinolytic substance close to the native t-PA, which can be administered as a rapid, single bolus injection. TNK-tPA is an enzyme (serine protease) that converts plasminogen to plasmin, primarily in the presence of fibrin. TNK-tPA also binds to fibrin in a thrombus and selectively converts thrombus- bound plasminogen to plasmin. This initiates local proteolysis of the fibrin matrix of the thrombus. Tenecteplase is a glycoprotein produced by recombinant DNA technique using Chinese Hamster Ovary (CHO) cells. It is a modified form of the naturally occurring human plasminogen activator. The molecule exhibits a well-known pronounced domain structure. Three sites of the molecule have been modified using site directed mutagenesis, thus tenecteplase has different pharmacokinetic properties from those of r-tPA. Metalyse is presented as a lyophilised powder in a 20-ml glass vial with a rubber stopper and a vial cap with an integrated reconstitution device. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Pharmacology of Recombinant Or Genetically Engineered Drugs
Pharmacology Pharmacology of Recombinant or Genetically Engineered Drugs Kamal Kishore, Pawan Krishan1 Departments of Pharmacy, M.J.P. Rohilkhand University, Bareilly-243 006, Uttar Pradesh, 1Pharmaceutical Sciences and Drug Research, Punjabi University, Patiala-147 002, Punjab, India Address for correspondence: Dr. Kamal Kishore; E-mail: [email protected] ABSTRACT Recombinant technology or genetic engineering is a modern method used for the synthesis of therapeutic agents. The central theme of recombinant technology is the process of “gene cloning” which consists of the production of a deÞ ned fragment of DNA and its propagation and ampliÞ cation in a suitable host cell. Drugs developed by recombinant technology or genetic engineering are known as biologics, biopharmaceuticals, recombinant DNA expressed products, bioengineered, or genetically engineered drugs. A current list of various products developed by recombinant technology includes erythropoietin, coagulation modulators, enzymes, hormones, interferons, interleukins, granulocyte colony-stimulating factors, anti-rheumatoid drugs, and various other agents like TNF, becaplermin, hepatitis-B vaccine, antibodies etc. This article provides general as well as recent pharmacological information on different aspects of recombinant drugs that may be useful for their better understanding by users and health care professionals. Key words: Biologics, erythropoietin, interferon, interleukins, insulin, thrombolytic enzymes DOI: 10.4103/0975-1483.55747 INTRODUCTION fragment of DNA and its propagation and ampliÞ cation in a suitable host cell. Recombinant technology was only Drugs developed using living organisms with the help of possible after the discovery of restriction endonucleases, biotechnology or genetic engineering are known as biologics, the enzymes used as cutters for a desired segment[3] of biopharmaceuticals, recombinant DNA expressed genes known as recognition sequences.