Anticoagulation Reversal in the Hemorrhagic Stroke Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
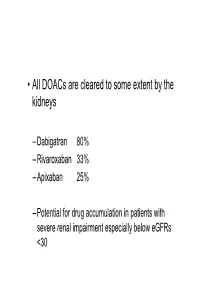
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Spontaneous Epidural Hematoma of the Cervical Spine Following Thrombolysis in a Patient with STEMI—Two Medical Specialties Facing a Rare Dilemma
Published online: 2019-12-05 THIEME Case Report 191 Spontaneous Epidural Hematoma of the Cervical Spine Following Thrombolysis in a Patient with STEMI—Two Medical Specialties Facing a Rare Dilemma Anastasios Tsarouchas1 Dimitrios Mouselimis1 Constantinos Bakogiannis1 Grigorios Gkasdaris2 George Dimitriadis3 Dimitrios Zioutas4 Christodoulos E. Papadopoulos1 13rd Cardiology Department, Hippokrateio University Hospital, Address for correspondence Grigorios Gkasdaris, MD, Department Aristotle University of Thessaloniki, Thessaloniki, Greece of Neurosurgery, KAT General Hospital of Attica, Athens 145 61, 2Department of Neurosurgery, KAT General Hospital of Attica, Greece (e-mail: [email protected]). Athens, Greece 3General Hospital of Katerini, Katerini, Greece 4St. Luke’s Hospital, Thessaloniki, Greece J Neurosci Rural Pract 2020;11:191–195 Abstract Spontaneous spinal epidural hematoma (SSEH) is a rare, albeit well-documented complication following thrombolysis treatment in ST elevation myocardial infarction (STEMI). A SSEH usually manifests with cervical pain and neurologic deficits and may require surgical intervention. In this case report, we present the first reported SSEH to occur following thrombolysis with reteplase. In this case, the SSEH manifested with cervical pain shortly after the patient emerged from his rescue percutaneous coronary intervention (PCI). Although magnetic resonance imaging reported spinal cord com- Keywords pression, the lack of neurologic symptoms prompted the treating clinicians to delay ► spinal epidural surgery. A dangerous dilemma emerged, as the usual antithrombotic regimen that hematoma was necessary to avoid stent thrombosis post-PCI, was also likely to exacerbate the ► spontaneous spinal bleeding. As a compromise, the patient only received aspirin as a single antiplatelet epidural hematoma therapy. Ultimately, the patient responded well to conservative treatment, with the ► cervical spine hematoma stabilizing a week later, without residual neurologic deficits. -

Anticoagulation Reversal Guideline for Adults
Anticoagulation Reversal Guideline for Adults Antithrombotic reversal strategies should be limited to clinical situations (i.e. life-threatening bleeding) where the immediate need for anticoagulant reversal outweighs the risk of thrombosis (either from the reversal agent itself or normalization of coagulation in a patient with underlying thromboembolic risk). These recommendations are meant to serve as general guidelines and should not replace clinical judgment. Always seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible. This document is not meant to guide selection of patients for reversal therapies. Please refer to appropriate national guidelines to aide decision- making regarding need for reversal, if warranted. 1. ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants 2. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine All indications for anticoagulation are considered, including atrial fibrillation, venous thromboembolism, prosthetic cardiac valves, and intracardiac thrombus. Mechanical circulatory support devices, including temporary or permanent ventricular assist devices (i.e. LVADs), are excluded from this document. Whenever possible, anticoagulation should be resumed in a timely manner to avoid thromboembolic complications related to the underlying indication for anticoagulation. This guideline does not provide recommendations on resuming anticoagulation. References: • Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Experts Consensus Decisions Pathways. J Am Coll Cardiol. -

Full Prescribing Information for - Active Internal Bleeding (4) RETAVASE
HIGHLIGHTS OF PRESCRIBING INFORMATION CONTRAINDICATIONS These highlights do not include all the information needed to use • Do not use in patients with: RETAVASE safely and effectively. See full prescribing information for - Active internal bleeding (4) RETAVASE. - Recent stroke (4) - Recent intracranial or intraspinal surgery or serious head trauma (4) RETAVASE (reteplase) for injection, for intravenous use - Intracranial neoplasm, arteriovenous malformation, or aneurysm (4) Initial U.S. Approval: 1996 - Known bleeding diathesis (4) - Severe uncontrolled hypertension (4) INDICATIONS AND USAGE RETAVASE is a tissue plasminogen activator (tPA) indicated for treatment of WARNINGS AND PRECAUTIONS acute ST-elevation myocardial infarction (STEMI) to reduce the risk of death • Increases the risk of bleeding. Avoid intramuscular injections. (5.1) and heart failure. (1) • Hypersensitivity (5.2) • Cholesterol embolism (5.3) Limitation of Use: The risk of stroke may outweigh the benefit produced by thrombolytic therapy in patients whose STEMI puts them at low risk for death ADVERSE REACTIONS or heart failure. (1) The most common adverse reaction (>5%) is bleeding. (6.1) DOSAGE AND ADMINISTRATION To report SUSPECTED ADVERSE REACTIONS, contact Chiesi USA, • Two 10 unit intravenous injections, each administered over 2 minutes, Inc. at 1-888-661-9260 or FDA at 1-800-FDA-1088 or 30 minutes apart. (2.1) www.fda.gov/medwatch. • No other medication should be injected or infused simultaneously via the same intravenous line or added to the injection solution. (2.1) USE IN SPECIFIC POPULATIONS • Pediatric Use: Safety and effectiveness have not been established. (8.4) DOSAGE FORMS AND STRENGTHS For Injection: 10 units as a lyophilized powder in single-use vials for Revised: 10/2020 reconstitution co-packaged with Sterile Water for Injection, USP in 10 mL prefilled syringe. -

Predicting Potential Drugs for Breast Cancer Based on Mirna and Tissue Specificity
Int. J. Biol. Sci. 2018, Vol. 14 971 Ivyspring International Publisher International Journal of Biological Sciences 2018; 14(8): 971-982. doi: 10.7150/ijbs.23350 Research Paper Predicting Potential Drugs for Breast Cancer based on miRNA and Tissue Specificity Liang Yu, Jin Zhao and Lin Gao School of Computer Science and Technology, Xidian University, Xi'an, 710071, P.R. China. Corresponding author: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2017.10.16; Accepted: 2017.12.14; Published: 2018.05.22 Abstract Network-based computational method, with the emphasis on biomolecular interactions and biological data integration, has succeeded in drug development and created new directions, such as drug repositioning and drug combination. Drug repositioning, that is finding new uses for existing drugs to treat more patients, offers time, cost and efficiency benefits in drug development, especially when in silico techniques are used. MicroRNAs (miRNAs) play important roles in multiple biological processes and have attracted much scientific attention recently. Moreover, cumulative studies demonstrate that the mature miRNAs as well as their precursors can be targeted by small molecular drugs. At the same time, human diseases result from the disordered interplay of tissue- and cell lineage-specific processes. However, few computational researches predict drug-disease potential relationships based on miRNA data and tissue specificity. Therefore, based on miRNA data and the tissue specificity of diseases, we propose a new method named as miTS to predict the potential treatments for diseases. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set
Form Title ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Form Number CH-0454 © 2018, Alberta Health Services, CKCM This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The license does not apply to content for which the Alberta Health Services is not the copyright owner. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/ Disclaimer: This material is intended for use by clinicians only and is provided on an DVLVZKHUHLVEDVLV$OWKRXJKUHDVRQDEOHHIIRUWVZHUHPDGHWRFRQ¿UPWKHDFFXUDF\RIWKH information, Alberta Health Services does not make any representation or warranty, express, LPSOLHGRUVWDWXWRU\DVWRWKHDFFXUDF\UHOLDELOLW\FRPSOHWHQHVVDSSOLFDELOLW\RU¿WQHVVIRU a particular purpose of such information. This material is not a substitute for the advice of a TXDOL¿HGKHDOWKSURIHVVLRQDO$OEHUWD+HDOWK6HUYLFHVH[SUHVVO\GLVFODLPVDOOOLDELOLW\IRUWKHXVH of these materials, and for any claims, actions, demands or suits arising from such use. Patient label placed here (if applicable) or if labels are not + used, minimum information below is required + Last Name First Name Birthdate (yyyy-Mon-dd) Gender PHN # ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Phone Number Date Time Initial (yyyy-Mon-dd) (hh:mm) 1. Patient Treatment & Monitoring Complete 12 lead ECG Stat if not already completed. Review with Physician. Take initial vital signs (Temp, HR, RR, SpO2, BP both arms) Repeat vital signs with any chest pain or equivalent symptoms. Initiate intravenous (IV) and infuse 0.9% sodium chloride at 30mL/hour (left arm preferred) Provide oxygen to keep SpO2 greater than or equal to 90% or with clinical signs of hypoxemia. Give acetylsalicylic acid 160 mg orally now, chewed or swallowed OR acetylsalicylic acid 160 mg orally administered pre-arrival (Time _______). -

Dosing and Administration Guide for RETAVASE® (Reteplase) for Injection1
RETAVASE® (reteplase) is a recombinant plasminogen activator which catalyzes the cleavage of endogenous plasminogen to generate plasmin. Plasmin degrades the fibrin matrix of the thrombus, exerting its thrombolytic action. Dosing and administration guide for RETAVASE® (reteplase) for injection1 RETAVASE is a tissue plasminogen activator (tPA) with the convenience of fixed dosing for your fibrinolytic needs in acute STEMI Administration with zero dose calculations As soon as possible after the 30 minutes later, administer onset of STEMI, administer 10 units 30min a second dose of 10 units intravenously over 2 minutes. intravenously. Each single-use vial contains 10 units of RETAVASE as lyophilized powder. Reconstitute RETAVASE immediately before administration using only the co-packaged Sterile Water for Injection, USP (see instructions on back). Indication and Usage Important Safety Information RETAVASE is a tissue plasminogen activator (tPA) Heparin and RETAVASE are incompatible. Do not administer indicated for treatment of acute ST-elevation RETAVASE through an intravenous line containing heparin. myocardial infarction (STEMI) to reduce the risk of death and heart failure. The most common adverse reaction (>5%) is bleeding. Limitation of Use: The risk of stroke may outweigh Please see Full Important Safety the benefit produced by thrombolytic therapy in Information on back. patients whose STEMI puts them at low risk for death or heart failure. Reconstitution instructions for RETAVASE® (reteplase) — the only fixed-dose fibrinolytic for acute STEMI1 Indication and Usage STEP 1 STEP 2 RETAVASE is a tissue plasminogen activator (tPA) indicated Uncap Clean vial for treatment of acute ST-elevation myocardial infarction spike, vial membrane (STEMI) to reduce the risk of death and heart failure. -
Best Evidence for Antithrombotic Agent Reversal in Bleeding
3/16/2021 1 JAMES H. PAXTON, MD • DIRECTOR OF CLINICAL RESEARCH • DETROIT RECEIVING HOSPITAL (DRH), DEPARTMENT OF EMERGENCY MEDICINE, WAYNE STATE UNIVERSITY • ATTENDING PHYSICIAN • SINAI-GRACE HOSPITAL (SGH) • DETROIT RECEIVING HOSPITAL (DRH) 2 1 3/16/2021 DISCLOSURES • FUNDED RESEARCH SPONSORED BY: TELEFLEX INC, 410 MEDICAL, HOSPI CORP. 3 OBJECTIVES •AT THE CONCLUSION OF THIS LECTURE, THE LEARNER WILL: • RECOGNIZE COMMON ANTITHROMBOTIC MEDICATIONS ASSOCIATED WITH BLEEDING EMERGENCIES • BE ABLE TO EXPLAIN THE MECHANISMS OF ACTION FOR COMMON ANTITHROMBOTIC MEDICATIONS • UNDERSTAND THE EVIDENCE FOR RAPID REVERSAL OF ANTITHROMBOTIC MEDICATIONS, INCLUDING CONTROVERSIES AND BEST PRACTICES HAVE FEWER NIGHTMARES ABOUT SCENES LIKE THE ONE ON THE NEXT SLIDE? 4 2 3/16/2021 BLEEDING IS BAD 5 WHEN TO REVERSE? • WHEN RISK OF BLEEDING OUTWEIGHS RISK OF REVERSAL: • INTRACRANIAL HEMORRHAGE (ICH) • OTHER CNS HEMATOMA (E.G., INTRAOCULAR, SPINAL) • EXSANGUINATING GASTROINTESTINAL (GI) BLEED • UNCONTROLLED RETROPERITONEAL BLEED • HEMORRHAGE INTO EXTREMITY WITH COMPARTMENT SYNDROME • CONSIDER IN POSTERIOR EPISTAXIS, HEMOTHORAX, PERICARDIAL TAMPONADE 6 3 3/16/2021 ANTITHROMBOTIC AGENTS •ANTI-PLATELET DRUGS •ANTI-COAGULANTS •FIBRINOLYTICS 7 THROMBOGENESIS • Primary component in arterial thrombosis (“white clot”) • Target for antiplatelet drugs • Primary component in venous thrombosis (“red clot”) • Aggregated platelets + • Target for anticoagulants fibrin mesh • Target for fibrinolytics 8 4 3/16/2021 PLATELET AGGREGATION Antiplatelet Drugs Mechanism Aspirin* -

In Vivo Effects of Contrast Media on Coronary Thrombolysis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 1102 JACC Vol. 32, No. 4 October 1998:1102–8 In Vivo Effects of Contrast Media on Coronary Thrombolysis SORIN PISLARU, MD, PHD,*† CRISTINA PISLARU, MD,* MONIKA SZILARD, MD,* JEF ARNOUT, PHD,‡ FRANS VAN DE WERF, MD, PHD, FACC* Leuven, Belgium and Bucharest, Romania Objectives. The aim of the present study was to evaluate the associated with longer reperfusion delays (time to optimal reper- influence of radiographic contrast media (CM) on alteplase- fusion: 67 6 48 min and 65 6 49 min, respectively, vs. 21 6 11 min induced coronary thrombolysis. after placebo; p < 0.05) and shorter periods of coronary perfusion Background. Contrast media inhibit fibrinolysis in vitro and (optimal perfusion time: 21 6 26 min and 21 6 28 min, respec- interact with endothelial cells, platelets and the coagulation tively, vs. 58 6 40 min after placebo; p < 0.05). No significant system. The in vivo effects of CM on thrombolysis are not known. differences were observed between groups with regard to activated Methods. Occlusive coronary artery thrombosis was induced in partial thromboplastin times, circulating thrombin-antithrombin 4 groups of 10 dogs by the copper coil technique. After 70 min of III complex concentrations and fibrinogen. occlusion the dogs were randomized to intracoronary injection of Conclusions. In this animal model administration of iohexol 2 2mlkg 1 of either saline, a low-osmolar ionic CM (ioxaglate), a and amidotrizoate before thrombolysis significantly delayed low-osmolar nonionic CM (iohexol) or a high-osmolar ionic CM reperfusion. -

Use of Antithrombotic Medications in the Presence of Neuraxial Anesthesia
Guideline: Use of Antithrombotic Medications In The Presence of Neuraxial Anesthesia Use of Antithrombotic Medications In The Presence of Neuraxial Anesthesia Purpose of Guidelines: To establish appropriate administration and timing of antithrombotic medications before, during, and after the use of neuraxial anesthesia to minimize the risk of bleeding. Definitions: Neuraxial Anesthesia = Delivery of anesthetic medication requiring placement of catheters or needles into the epidural or spinal space Antithrombotic Medications = Anticoagulant, antiplatelet, and thrombolytic medications Background1-3: Spinal (or epidural) hematomas are a rare but catastrophic complication of neuraxial anesthesia. The risk of hematoma development is increased in the presence of antithrombotic medication. Patients undergoing neuraxial anesthesia must have the risks of bleeding from neuraxial interventions balanced with the underlying and ongoing risk of thromboembolism necessitating anticoagulation. Recommendations for the management of specific antithrombotics in patients undergoing neuraxial anesthesia are provided in the following Tables: o Table 1. Management of Intravenous and Subcutaneous Anticoagulation Therapy in Patients Undergoing Neuraxial Anesthesia o Table 2. Management of ORAL Anticoagulation Therapy in Patients Undergoing Neuraxial Anesthesia o Table 3. Management of ORAL and Intravenous Antiplatelet and Thrombolytic Therapy in Patients Undergoing Neuraxial Anesthesia Workflow if a Contradicted Medication is Prescribed: Providers will have