Predicting Potential Treatments for Complex Diseases Based on Mirna and Tissue Specificity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Restoration of Temozolomide Sensitivity by PARP Inhibitors In
Published OnlineFirst January 3, 2020; DOI: 10.1158/1078-0432.CCR-19-2000 CLINICAL CANCER RESEARCH | TRANSLATIONAL CANCER MECHANISMS AND THERAPY Restoration of Temozolomide Sensitivity by PARP Inhibitors in Mismatch Repair Deficient Glioblastoma is Independent of Base Excision Repair Fumi Higuchi1,2, Hiroaki Nagashima1, Jianfang Ning1,3, Mara V.A. Koerner1, Hiroaki Wakimoto1, and Daniel P. Cahill1 ABSTRACT ◥ Purpose: Emergence of mismatch repair (MMR) deficiency is a Results: While having no detectable effect in MSH6 wild-type frequent mechanism of acquired resistance to the alkylating che- GBMs, PARPi selectively restored TMZ sensitivity in MSH6- motherapeutic temozolomide (TMZ) in gliomas. Poly(ADP-ribose) deficient GBM cells. This genotype-specific restoration of activity polymerase inhibitors (PARPi) have been shown to potentiate TMZ translated in vivo, where combination treatment of veliparib cytotoxicity in several cancer types, including gliomas. We tested and TMZ showed potent suppression of tumor growth of whether PARP inhibition could re-sensitize MSH6-null MMR- MSH6-inactivated orthotopic xenografts, compared with TMZ deficient gliomas to TMZ, and assessed the role of the base excision monotherapy. Unlike PARPi, genetic and pharmacological block- repair (BER) DNA damage repair pathway in PARPi-mediated age of BER pathway did not re-sensitize MSH6-inactivated GBM effects. cells to TMZ. Similarly, CRISPR PARP1 knockout did not re- Methods: Isogenic pairs of MSH6 wild-type and MSH6-inacti- sensitize MSH6-inactivated GBM cells to TMZ. vated human glioblastoma (GBM) cells (including both IDH1/2 Conclusions: PARPi restoration of TMZ chemosensitivity in wild-type and IDH1 mutant), as well as MSH6-null cells derived MSH6-inactivated glioma represents a promising strategy to from a patient with recurrent GBM were treated with TMZ, the overcome acquired chemoresistance caused by MMR deficiency. -
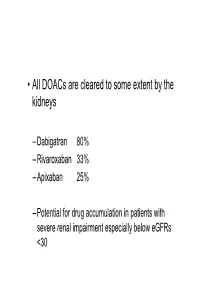
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Table of Contents
NTICANCER ESEARCH InternationalA Journal of Cancer ResearchR and Treatment ISSN: 0250-7005 Volume 24, Number 4, July-August 2004 Contents Experimental Studies Inhibition of the Human Apurinic/Apyrimidinic Endonuclease (Ape1) Repair Activity and Sensitization of Breast Cancer Cells to DNA Alkylating Agents with Lucanthone. M. LUO, M.R. KELLEY (Indianapolis, Indiana, USA)........................................................................................................................................................... 2127 Androgen Withdrawal Inhibits Tumor Growth and is Associated with Decrease in Angiogenesis and VEGF Expression in Androgen-Independent CWR22Rv1 Human Prostate Cancer Model. L. CHENG, S. ZHANG, C.J. SWEENEY, C. KAO, T.A GARDNER, J.N. EBLE (Indianapolis, Indiana, USA) .................................. 2135 In Vitro Generation of Cytolytic T Cells Against Human Melanoma Cells Overexpressing HDM2. A. SORURI, A. FAYYAZI, S. GANGL, C. GRIESINGER, C.A. ALBRECHT, T. SCHLOTT (Goettingen; Langen, Germany) .................................................................................................................................................... 2141 Artemisinin: An Alternative Treatment for Oral Squamous Cell Carcinoma. E. YAMACHIKA, T. HABTE, D. ODA (Seattle, WA, USA; Okayama City, Japan).............................................................................................. 2153 S19-mRNA Expression in Squamous Cell Carcinomas of the Upper Aerodigestive Tract. V. SENGPIEL, T. ROST, T. GÖRÖGH, I.O. RATHCKE, J.A. -

Anticoagulation Reversal Guideline for Adults
Anticoagulation Reversal Guideline for Adults Antithrombotic reversal strategies should be limited to clinical situations (i.e. life-threatening bleeding) where the immediate need for anticoagulant reversal outweighs the risk of thrombosis (either from the reversal agent itself or normalization of coagulation in a patient with underlying thromboembolic risk). These recommendations are meant to serve as general guidelines and should not replace clinical judgment. Always seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible. This document is not meant to guide selection of patients for reversal therapies. Please refer to appropriate national guidelines to aide decision- making regarding need for reversal, if warranted. 1. ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants 2. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine All indications for anticoagulation are considered, including atrial fibrillation, venous thromboembolism, prosthetic cardiac valves, and intracardiac thrombus. Mechanical circulatory support devices, including temporary or permanent ventricular assist devices (i.e. LVADs), are excluded from this document. Whenever possible, anticoagulation should be resumed in a timely manner to avoid thromboembolic complications related to the underlying indication for anticoagulation. This guideline does not provide recommendations on resuming anticoagulation. References: • Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Experts Consensus Decisions Pathways. J Am Coll Cardiol. -

Induction of Concentration-Dependent Blockade in the G2 Phase of the Cell Cycle by Cancer Chemotherapeutic Agents1
[CANCER RESEARCH 38, 809-814, March 1978] Induction of Concentration-dependent Blockade in the G2 Phase of the Cell Cycle by Cancer Chemotherapeutic Agents1 Bruce F. Kimler,2 Martin H. Schneiderman,3 and Dennis B. Leeper Laboratory of Experimental Radiation Oncology, Department of Radiation Therapy and Nuclear Medicine, Thomas Jefferson University Hospital, Philadelphia, Pennsylvania ABSTRACT for detailed analysis. Thus, results have been limited to describing the location of a block in terms of general The mitotic cell selection procedure for cell cycle anal phases of the cell cycle, i.e., G,, S, G,,, M, or at the ysis was utilized with Chinese hamster ovary fibroblasts boundary between 2 phases. Even when greater precision to determine the transition points in G,, i.e., the age in G, was attained, seldom was a concentration dependence of at which cells become refractory to drug-induced progres the location of the block observed (29). sion blockade, for several cancer Chemotherapeutic Using the mitotic cell selection procedure for cell cycle agents and antimetabolites over a 1000-fold concentration analysis (26), we have determined the number of cells range. refractory to drug-induced G-,blockade after treatment with The G transition points for five anticancer drugs (acti- various concentrations of several cancer Chemotherapeutic nomycin D, Adriamycin, lucanthone, mitomycin C, and agents and antimetabolites. We were able to calculate the bleomycin) varied linearly as a function of the logarithm time in G2 at which a particular concentration of drug of the drug concentration between the S-G_,boundary at inhibited progression or induced a delay. low concentrations and prometaphase (45 min prior to the end of karyokinesis) at high concentrations. -

WO 2013/061161 A2 2 May 2013 (02.05.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/061161 A2 2 May 2013 (02.05.2013) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/337 (2006.01) A61K 31/48 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/395 (2006.01) A61K 31/51 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/4174 (2006.01) A61K 31/549 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A61K 31/428 (2006.01) A61K 31/663 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (21) International Application Number: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, PCT/IB20 12/002768 ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (22) International Filing Date: NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, 25 October 2012 (25.10.2012) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (25) Filing Language: English ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/552,922 28 October 201 1 (28. -

Predicting Potential Drugs for Breast Cancer Based on Mirna and Tissue Specificity
Int. J. Biol. Sci. 2018, Vol. 14 971 Ivyspring International Publisher International Journal of Biological Sciences 2018; 14(8): 971-982. doi: 10.7150/ijbs.23350 Research Paper Predicting Potential Drugs for Breast Cancer based on miRNA and Tissue Specificity Liang Yu, Jin Zhao and Lin Gao School of Computer Science and Technology, Xidian University, Xi'an, 710071, P.R. China. Corresponding author: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2017.10.16; Accepted: 2017.12.14; Published: 2018.05.22 Abstract Network-based computational method, with the emphasis on biomolecular interactions and biological data integration, has succeeded in drug development and created new directions, such as drug repositioning and drug combination. Drug repositioning, that is finding new uses for existing drugs to treat more patients, offers time, cost and efficiency benefits in drug development, especially when in silico techniques are used. MicroRNAs (miRNAs) play important roles in multiple biological processes and have attracted much scientific attention recently. Moreover, cumulative studies demonstrate that the mature miRNAs as well as their precursors can be targeted by small molecular drugs. At the same time, human diseases result from the disordered interplay of tissue- and cell lineage-specific processes. However, few computational researches predict drug-disease potential relationships based on miRNA data and tissue specificity. Therefore, based on miRNA data and the tissue specificity of diseases, we propose a new method named as miTS to predict the potential treatments for diseases. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set
Form Title ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Form Number CH-0454 © 2018, Alberta Health Services, CKCM This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The license does not apply to content for which the Alberta Health Services is not the copyright owner. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/ Disclaimer: This material is intended for use by clinicians only and is provided on an DVLVZKHUHLVEDVLV$OWKRXJKUHDVRQDEOHHIIRUWVZHUHPDGHWRFRQ¿UPWKHDFFXUDF\RIWKH information, Alberta Health Services does not make any representation or warranty, express, LPSOLHGRUVWDWXWRU\DVWRWKHDFFXUDF\UHOLDELOLW\FRPSOHWHQHVVDSSOLFDELOLW\RU¿WQHVVIRU a particular purpose of such information. This material is not a substitute for the advice of a TXDOL¿HGKHDOWKSURIHVVLRQDO$OEHUWD+HDOWK6HUYLFHVH[SUHVVO\GLVFODLPVDOOOLDELOLW\IRUWKHXVH of these materials, and for any claims, actions, demands or suits arising from such use. Patient label placed here (if applicable) or if labels are not + used, minimum information below is required + Last Name First Name Birthdate (yyyy-Mon-dd) Gender PHN # ST Elevation Myocardial Infarction (STEMI) Reperfusion Order Set Phone Number Date Time Initial (yyyy-Mon-dd) (hh:mm) 1. Patient Treatment & Monitoring Complete 12 lead ECG Stat if not already completed. Review with Physician. Take initial vital signs (Temp, HR, RR, SpO2, BP both arms) Repeat vital signs with any chest pain or equivalent symptoms. Initiate intravenous (IV) and infuse 0.9% sodium chloride at 30mL/hour (left arm preferred) Provide oxygen to keep SpO2 greater than or equal to 90% or with clinical signs of hypoxemia. Give acetylsalicylic acid 160 mg orally now, chewed or swallowed OR acetylsalicylic acid 160 mg orally administered pre-arrival (Time _______). -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Quinolizidine-Derived Lucanthone and Amitriptyline Analogues Endowed with Potent Antileishmanial Activity
pharmaceuticals Article Quinolizidine-Derived Lucanthone and Amitriptyline Analogues Endowed with Potent Antileishmanial Activity Michele Tonelli 1,* , Anna Sparatore 2,* , Nicoletta Basilico 3,* , Loredana Cavicchini 3, Silvia Parapini 4 , Bruno Tasso 1 , Erik Laurini 5 , Sabrina Pricl 5,6 , Vito Boido 1 and Fabio Sparatore 1 1 Dipartimento di Farmacia, Università degli Studi di Genova, Viale Benedetto XV, 3, 16132 Genova, Italy; [email protected] (B.T.); [email protected] (V.B.); [email protected] (F.S.) 2 Dipartimento di Scienze Farmaceutiche, Università degli Studi di Milano, Via Mangiagalli 25, 20133 Milano, Italy 3 Dipartimento di Scienze Biomediche Chirurgiche e Odontoiatriche, Università degli Studi di Milano, Via Pascal 36, 20133 Milano, Italy; [email protected] 4 Dipartimento di Scienze Biomediche per la Salute, Università degli Studi di Milano, Via Mangiagalli 31, 20133 Milano, Italy; [email protected] 5 Molecular Biology and Nanotechnology Laboratory (MolBNL@UniTS), DEA, Piazzale Europa 1, 34127 Trieste, Italy; [email protected] (E.L.); [email protected] (S.P.) 6 Department of General Biophysics, Faculty of Biology and Environmental Protection, University of Lodz, 90-236 Lodz, Poland * Correspondence: [email protected] (M.T.); [email protected] (A.S.); [email protected] (N.B.) Received: 4 October 2020; Accepted: 21 October 2020; Published: 25 October 2020 Abstract: Leishmaniases are neglected diseases that are endemic in many tropical and sub-tropical Countries. Therapy is based on different classes of drugs which are burdened by severe side effects, occurrence of resistance and high costs, thereby creating the need for more efficacious, safer and inexpensive drugs.