Current Insights Into Collagen Type I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Characterization of Collagen Fibers (I, III, IV) and Elastin of Normal and Neoplastic Canine Prostatic Tissues
veterinary sciences Article Characterization of Collagen Fibers (I, III, IV) and Elastin of Normal and Neoplastic Canine Prostatic Tissues Luis Gabriel Rivera Calderón 1, Priscila Emiko Kobayashi 2, Rosemeri Oliveira Vasconcelos 1, Carlos Eduardo Fonseca-Alves 3 and Renée Laufer-Amorim 2,* 1 Department of Veterinary Pathology, School of Agricultural and Veterinarian Sciences, São Paulo State University (Unesp), Jaboticabal, São Paulo 14884-900, Brazil; [email protected] (L.G.R.C.); [email protected] (R.O.V.) 2 Department of Veterinary Clinic, School of Veterinary Medicine and Animal Science, São Paulo State University (Unesp), Botucatu, São Paulo 18618-681, Brazil; [email protected] 3 Department of Veterinary Surgery and Anesthesiology, School of Veterinary Medicine and Animal Science, São Paulo State University (Unesp), Botucatu, São Paulo 18618-681, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-14-3880-2076 Received: 7 January 2019; Accepted: 25 February 2019; Published: 2 March 2019 Abstract: This study aimed to investigate collagen (Coll-I, III, IV) and elastin in canine normal prostate and prostate cancer (PC) using Picrosirius red (PSR) and Immunohistochemical (IHC) analysis. Eight normal prostates and 10 PC from formalin-fixed, paraffin-embedded samples were used. Collagen fibers area was analyzed with ImageJ software. The distribution of Coll-I and Coll-III was approximately 80% around prostatic ducts and acini, 15% among smooth muscle, and 5% surrounding blood vessels, in both normal prostate and PC. There was a higher median area of Coll-III in PC when compared to normal prostatic tissue (p = 0.001 for PSR and p = 0.05 for IHC). -

Collagen Type I and Decorin Expression in Tenocytes Depend On
Wagenhäuser et al. BMC Musculoskeletal Disorders 2012, 13:140 http://www.biomedcentral.com/1471-2474/13/140 RESEARCH ARTICLE Open Access Collagen type I and decorin expression in tenocytes depend on the cell isolation method Markus U Wagenhäuser1†, Matthias F Pietschmann1*†, Birte Sievers1, Denitsa Docheva2, Matthias Schieker2, Volkmar Jansson1 and Peter E Müller1 Abstract Backround: The treatment of rotator cuff tears is still challenging. Tendon tissue engineering (TTE) might be an alternative in future. Tenocytes seem to be the most suitable cell type as they are easy to obtain and no differentiation in vitro is necessary. The aim of this study was to examine, if the long head of the biceps tendon (LHB) can deliver viable tenocytes for TTE. In this context, different isolation methods, such as enzymatic digestion (ED) and cell migration (CM), are investigated on differences in gene expression and cell morphology. Methods: Samples of the LHB were obtained from patients, who underwent surgery for primary shoulder arthroplasty. Using ED as isolation method, 0.2% collagenase I solution was used. Using CM as isolation method, small pieces of minced tendon were put into petri-dishes. After cell cultivation, RT-PCR was performed for collagen type I, collagen type III, decorin, tenascin-C, fibronectin, Scleraxis, tenomodulin, osteopontin and agreccan. Results: The total number of isolated cells, in relation to 1 g of native tissue, was 14 times higher using ED. The time interval for cell isolation was about 17 hours using ED and approximately 50 days using CM. Cell morphology in vitro was similar for both isolation techniques. Higher expression of collagen type I could be observed in tenocyte-like cell cultures (TLCC) using ED as isolation method (p < 0.05), however decorin expression was higher in TLCC using CM as isolation method (p < 0.05). -

Collagens—Structure, Function, and Biosynthesis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of East Anglia digital repository Advanced Drug Delivery Reviews 55 (2003) 1531–1546 www.elsevier.com/locate/addr Collagens—structure, function, and biosynthesis K. Gelsea,E.Po¨schlb, T. Aignera,* a Cartilage Research, Department of Pathology, University of Erlangen-Nu¨rnberg, Krankenhausstr. 8-10, D-91054 Erlangen, Germany b Department of Experimental Medicine I, University of Erlangen-Nu¨rnberg, 91054 Erlangen, Germany Received 20 January 2003; accepted 26 August 2003 Abstract The extracellular matrix represents a complex alloy of variable members of diverse protein families defining structural integrity and various physiological functions. The most abundant family is the collagens with more than 20 different collagen types identified so far. Collagens are centrally involved in the formation of fibrillar and microfibrillar networks of the extracellular matrix, basement membranes as well as other structures of the extracellular matrix. This review focuses on the distribution and function of various collagen types in different tissues. It introduces their basic structural subunits and points out major steps in the biosynthesis and supramolecular processing of fibrillar collagens as prototypical members of this protein family. A final outlook indicates the importance of different collagen types not only for the understanding of collagen-related diseases, but also as a basis for the therapeutical use of members of this protein family discussed in other chapters of this issue. D 2003 Elsevier B.V. All rights reserved. Keywords: Collagen; Extracellular matrix; Fibrillogenesis; Connective tissue Contents 1. Collagens—general introduction ............................................. 1532 2. Collagens—the basic structural module......................................... -

Sources of Collagen for Biomaterials in Skin Wound Healing
bioengineering Review Sources of Collagen for Biomaterials in Skin Wound Healing Evan Davison-Kotler 1,2, William S. Marshall 1 and Elena García-Gareta 2,* 1 Biology Department, St. Francis Xavier University, Antigonish, NS B2G 2W5, Canada 2 Regenerative Biomaterials Group, The RAFT Institute, Mount Vernon Hospital, Northwood HA6 2RN, UK * Correspondence: [email protected]; Tel.: +44-(0)-1923844350 Received: 23 May 2019; Accepted: 26 June 2019; Published: 30 June 2019 Abstract: Collagen is the most frequently used protein in the fields of biomaterials and regenerative medicine. Within the skin, collagen type I and III are the most abundant, while collagen type VII is associated with pathologies of the dermal–epidermal junction. The focus of this review is mainly collagens I and III, with a brief overview of collagen VII. Currently, the majority of collagen is extracted from animal sources; however, animal-derived collagen has a number of shortcomings, including immunogenicity, batch-to-batch variation, and pathogenic contamination. Recombinant collagen is a potential solution to the aforementioned issues, although production of correctly post-translationally modified recombinant human collagen has not yet been performed at industrial scale. This review provides an overview of current collagen sources, associated shortcomings, and potential resolutions. Recombinant expression systems are discussed, as well as the issues associated with each method of expression. Keywords: collagen; collagen sources; recombinant collagen; biomaterials; regenerative medicine; tissue engineering; wound healing; skin 1. Introduction 1.1. The Molecular Structure of Collagen The 28 different collagen types of the collagen superfamily are further divided into eight subfamilies, with the majority of the collagen types belonging to the fibril-forming or fibrillar subfamily [1,2]. -

Osteogenesis Imperfecta Types I-XI Implications for the Neonatal Nurse Jody Womack , RNC-NIC, NNP-BC, MS
Ksenia Zukowsky, PhD, APRN, NNP-BC ❍ Section Editor Beyond the Basics 3.0 HOURS Continuing Education Osteogenesis Imperfecta Types I-XI Implications for the Neonatal Nurse Jody Womack , RNC-NIC, NNP-BC, MS ABSTRACT Osteogenesis imperfecta (OI), also called “brittle bone disease,” is a rare heterozygous connective tissue disorder that is caused by mutations of genes that affect collagen. Osteogenesis imperfecta is characterized by decreased bone mass, bone fragility, and skin hyperlaxity. The phenotype present is determined according to the mutation on the affected gene as well as the type and location of the mutation. Osteogenesis imperfecta is neither preventable nor treatable. Osteogenesis imperfecta is classified into 11 types to date, on the basis of their clinical symptoms and genetic components. This article discusses the definition of the disease, the classifications on the basis of its clinical features, incidence, etiology, and pathogenesis. In addition, phenotype, natural history, diagnosis and manage- ment of this disease, recurrence risk, and, most importantly, the implications for the neonatal nurse and management for the family are discussed. Key Words: brittle bone disease , COL1A1 , COL1A2 , collagen disorders , osteogenesis imperfecta steogenesis imperfecta (OI) is a rare connec- is imperative to help the patient and the parents car- tive tissue disorder that is caused by muta- ing for infants born with OI. tions of genes that affect collagen. 1-4 Collagen O is the major protein of connective tissues, which is the REVIEW OF LITERATURE framework of bones. When collagen is not function- ing properly or there is lack of collagen in the tissue, Osteogenesis imperfecta was thought to have affected bones break easily. -

Serum Type I and Type III Procollagen Peptide Levels in Sarcoidosis
Eur Respir J, 1996, 9, 1648–1651 Copyright ERS Journals Ltd 1996 DOI: 10.1183/09031936.96.09081648 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Serum type I and type III procollagen peptide levels in sarcoidosis L. Bacchella*, C. Tinelli**, L.S. Gilè+, V. Peona+, C. Aprile*, M.Gorrini+, L. Pasturenzi+, G. Cetta++, M. Luisetti+ Serum type I and type III procollagen peptide levels in sarcoidosis. L. Bacchella, C. *Servizio di Medicina Nucleare, Fondazione Tinelli, L.S. Gilè, V. Peona, C. Aprile, M.Gorrini, L. Pasturenzi, G. Cetta, M. Luisetti. Clinica del Lavoro, Pavia, Italy. **Unità ERS Journals Ltd 1996. di Statistica and +Istituto di Tisiologia e ABSTRACT: Type I and type III are the most abundant collagens in the lung. Malattie Respiratorie, IRCCS Policlinico ++ The aim of our study was to compare type I and III procollagen peptides in sera San Matteo, Pavia, Italy. Dipartimento of sarcoid patients. di Biochimica, Università di Pavia, Italy. Sixty eight patients with sarcoidosis were studied (19 with newly recognized dis- Correspondence: M. Luisetti, Istituto di ease, 7 with relapsing disease, 15 with chronic disease, and 27 in stable remission). Tisiologia e Malattie Respiratorie, IRCCS Thirty healthy volunteers served as controls. The levels of procollagen I and III Policlinico San Matteo, Università degli peptides were determined by radioimmunoassay. Angiotensin-converting enzyme Studi di Pavia, Via Taramelli 5, 27100 (ACE) level was evaluated by means of a colorimetric assay. Pavia, Italy In patients with newly recognized sarcoidosis, both serum procollagen I and III peptide levels were increased with respect to controls (p=0.0014 and p<0.00001, Keywords: Angiotensin-converting enzyme, respectively). -

Identification and Structural Analysis of Type I Collagen Sites in Complex with Fibronectin Fragments
Identification and structural analysis of type I collagen sites in complex with fibronectin fragments Miche` le C. Erata, David A. Slatterb, Edward D. Lowec, Christopher J. Millarda, Richard W. Farndaleb, Iain D. Campbella, and Ioannis Vakonakisa,1 aDepartment of Biochemistry and cLaboratory of Molecular Biophysics, University of Oxford, Oxford OX1 3QU, United Kingdom; and bDepartment of Biochemistry, University of Cambridge, Cambridge CB2 1QW, United Kingdom Edited by John Kuriyan, University of California, Berkeley, CA, and approved January 28, 2009 (received for review December 9, 2008) Collagen and fibronectin are major components of vertebrate ments bind the same peptide sequence just C-terminal to the extracellular matrices. Their association and distribution control MMP-1 cleavage site; the tightest binding, however, is mediated 8–9 the development and properties of diverse tissues, but thus far no by the FnI domain pair that also binds ␣2(I). A 2.1-Å crystal 8–9 structural information has been available for the complex formed. structure of FnI in complex with the ␣1(I) peptide shows an ␣ Here, we report binding of a peptide, derived from the 1 chain of extended single-strand peptide conformation, which suggests type I collagen, to the gelatin-binding domain of human fibronec- that FN stabilizes a noncanonical collagen structure upon bind- tin and present the crystal structure of this peptide in complex with ing. We explore this hypothesis in thermal denaturation exper- 8–9 the FnI domain pair. Both gelatin-binding domain subfrag- iments using model triple-helical peptides. The results presented 6 1–2 7 8–9 ments, FnI FnII FnI and FnI, bind the same specific sequence show the first atomic resolution picture of the interaction ␣ on D-period 4 of collagen I 1, adjacent to the MMP-1 cleavage site. -

Three Decades of Research on Recombinant Collagens: Reinventing the Wheel Or Developing New Biomedical Products?
bioengineering Review Three Decades of Research on Recombinant Collagens: Reinventing the Wheel or Developing New Biomedical Products? Andrzej Fertala Department of Orthopaedic Surgery, Sidney Kimmel Medical College, Thomas Jefferson University, Curtis Building, Room 501, 1015 Walnut Street, Philadelphia, PA 19107, USA; axf116@jefferson.edu; Tel.: +1-215-503-0113 Received: 20 October 2020; Accepted: 23 November 2020; Published: 2 December 2020 Abstract: Collagens provide the building blocks for diverse tissues and organs. Furthermore, these proteins act as signaling molecules that control cell behavior during organ development, growth, and repair. Their long half-life, mechanical strength, ability to assemble into fibrils and networks, biocompatibility, and abundance from readily available discarded animal tissues make collagens an attractive material in biomedicine, drug and food industries, and cosmetic products. About three decades ago, pioneering experiments led to recombinant human collagens’ expression, thereby initiating studies on the potential use of these proteins as substitutes for the animal-derived collagens. Since then, scientists have utilized various systems to produce native-like recombinant collagens and their fragments. They also tested these collagens as materials to repair tissues, deliver drugs, and serve as therapeutics. Although many tests demonstrated that recombinant collagens perform as well as their native counterparts, the recombinant collagen technology has not yet been adopted by the biomedical, pharmaceutical, or food industry. This paper highlights recent technologies to produce and utilize recombinant collagens, and it contemplates their prospects and limitations. Keywords: recombinant collagen; gelatin; biomaterials; tissue engineering 1. Introduction Proteins, including insulin, various growth factors, enzymes, vaccines, and antibodies serve as irreplaceable therapeutics to prevent and treat diverse diseases. -

Structure, Function and Ageing of the Collagens of the Eye
Eye (1987) 1, 175-183 Structure, Function and Ageing of the Collagens of the Eye ALLEN 1. BAILEY Bristol I. Introduci:ion twelve genetically distinct types of collagen in The collagenous tissues of the eye have mammalian tissues. They have all been charac received considerable attention since, 'apart terised biochemically and their precise from the importance ofthe organ itself, the eye location in complex tissues has been deter is composed of several highly specialised mined by immunohistochemical techniques. tissues which possess distinct collagenous The collagens identifiedto date have been clas structures. It is, in fact, a vivid example of the sified by several criteria, length of molecule, biological diversity of collagenous tissues. This molecular weight, flexibility of the molecule, diversity has recently been shown to be due to and by ultimate supramolecular structure. the existence of a whole family of collagen mol Employing the latter classification one can ecules that are capable of aggregating in dif consider three groups: the fibrous collagens, ferent ways to produce a variety of collagenous the non-fibrouscollagens and the filamentous structures.l At the present time there are about collagens. The variations in structure of these aggregates is shown in Figure 1. FffiROUS COLLAGENS Fibrous collagens. These collagens are revealed in the electron microscope as thick TypeI,n,JIl fibreswith a characteristic axial repeat pattern of 67 nm. The diameter of the fibresvaries con siderably, from 200 nm in skin and tendon to NON - FIBROUS COLLAGENS about 25 nm in the cornea. The size distri Type IV bution within a particular tissue may be uni form, for example the fibresof the cornea vary from 25 to 30 nm, or may be highly variable as in the skin, where they can vary from 20 to 200nm. -
3Helix.Com (Tech Support)
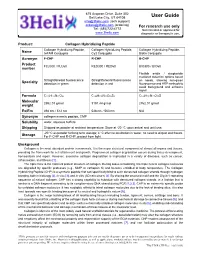
675 Arapeen Drive, Suite 302 Salt Lake City, UT 84108 User Guide [email protected] (tech support) [email protected] (ordering) For research use only Tel: (385)722-4772 Not intended or approved for www.3helix.com diagnostic or therapeutic use. Product: Collagen Hybridizing Peptide Collagen Hybridizing Peptide, Collagen Hybridizing Peptide, Collagen Hybridizing Peptide, Name 5-FAM Conjugate Cy3 Conjugate Biotin Conjugate Acronym F-CHP R-CHP B-CHP Product FLU300 / FLU60 RED300 / RED60 BIO300 / BIO60 number Flexible avidin / streptavidin mediated detection options based Straightforward fluorescence Straightforward fluorescence on needs, allowing non-green Specialty detection in green detection in red fluorescence and HRP methods to avoid background and enhance signal Formula C135H175N31O45 C144H198N33O46S2 C124H181N31O39S Molecular 2952.01 g/mol 3191.44 g/mol 2762.01 g/mol weight Ex/Em 494 nm / 512 nm 548 nm / 563 nm N/A Synonym collagen mimetic peptide, CMP Solubility water, aqueous buffers Shipping Shipped as powder at ambient temperature. Store at -20 °C upon arrival and until use. -20 °C as powder for long term storage; 4 °C after reconstitution in water, no need to aliquot and freeze. Storage For F-CHP and R-CHP, protect from light. Background Collagen is the most abundant protein in mammals. It is the major structural component of almost all organs and tissues, providing the framework for cell attachment and growth. Programmed collagen degradation occurs during tissue development, homeostasis and repair. However, excessive collagen degradation is implicated in a variety of diseases, such as cancer, inflammation, and fibrosis [1]. The triple helix is the hallmark protein structure of collagen. -

Mechanics and Structural Stability of the Collagen Triple Helix
Mechanics and Structural Stability of the Collagen Triple Helix Michael W.H. Kirkness,1 Kathrin Lehmann2 and Nancy R. Forde1,2 1Department of Molecular Biology and Biochemistry and 2Department of Physics, Simon Fraser University. Burnaby, BC, V5A 1S6 Canada [email protected] Abstract The primary building block of the body is collagen, which is found in the extracellular matrix and in many stress-bearing tissues such as tendon and cartilage. It provides elasticity and support to cells and tissues while influencing biological pathways including cell signaling, motility and differentiation. Collagen’s unique triple helical structure is thought to impart mechanical stability. However, detailed experimental studies on its molecular mechanics have been only recently emerging. Here, we review the treatment of the triple helix as a homogeneous flexible rod, including bend (standard worm-like chain model), twist, and stretch deformations, and the assumption of backbone linearity. Additionally, we discuss protein- specific properties of the triple helix including sequence dependence, and relate single-molecule mechanics to collagen’s physiological context. Introduction Collagen is the most abundant protein in the human body, accounting for more than 30% of the total protein.1,2 Collagens are defined by their unique right-handed triple helical structure, comprised of three left-handed polyproline-like helices, each with a (Gly-X-Y) repeating sequence where X and Y are often proline and hydroxyproline.2 In the body, collagen forms ordered, hierarchical -

Skin Collagen Through the Lifestages: Importance for Skin Health and Beauty
Reilly et al. Plast Aesthet Res 2021;8:2 Plastic and DOI: 10.20517/2347-9264.2020.153 Aesthetic Research Review Open Access Skin collagen through the lifestages: importance for skin health and beauty David M. Reilly1, Jennifer Lozano2 1Research and Clinicals, Minerva Research Labs, London W1S 1DN, UK. 2NPD and Regulatory, Minerva Research Labs, London W1S 1DN, UK. Correspondence to: Dr. David M. Reilly, Research and Clinicals, Minerva Research Labs, 106 New Bond Street, Mayfair, London W1S 1DN, UK. E-mail: [email protected] How to cite this article: Reilly DM, Lozano J. Skin collagen through the lifestages: importance for skin health and beauty. Plast Aesthet Res 2021;8:2. http://dx.doi.org/10.20517/2347-9264.2020.153 Received: 20 Jul 2020 First Decision: 2 Oct 2020 Revised: 15 Oct 2020 Accepted: 9 Dec 2020 Published: 8 Jan 2021 Academic Editor: Salvador Gonzalez, Raúl González-García Copy Editor: Monica Wang Production Editor: Jing Yu Abstract Collagen-based supplements have become a keystone in the management of the ageing process, with proven ability to repair skin damage, bestowing a youthful and healthy appearance sought in the pursuit of beauty. Collagen is an essential scaffold protein that gives smoothness and elasticity to skin, but its production declines with age. Finding ways to tackle this problem is now strongly promoted as an effective way to transform skin and hair, repairing age- related deterioration. A growing number of scientific studies show exciting evidence that it is possible to rejuvenate ageing or damaged skin, improve function of worn joints, and support personal wellbeing and vitality.