Obstetrics and Gyneclogy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2021 – the Following CPT Codes Are Approved for Billing Through Women’S Way
WHAT’S COVERED – 2021 Women’s Way CPT Code Medicare Part B Rate List Effective January 1, 2021 For questions, call the Women’s Way State Office 800-280-5512 or 701-328-2389 • CPT codes that are specifically not covered are 77061, 77062 and 87623 • Reimbursement for treatment services is not allowed. (See note on page 8). • CPT code 99201 has been removed from What’s Covered List • New CPT codes are in bold font. 2021 – The following CPT codes are approved for billing through Women’s Way. Description of Services CPT $ Rate Office Visits New patient; medically appropriate history/exam; straightforward decision making; 15-29 minutes 99202 72.19 New patient; medically appropriate history/exam; low level decision making; 30-44 minutes 99203 110.77 New patient; medically appropriate history/exam; moderate level decision making; 45-59 minutes 99204 165.36 New patient; medically appropriate history/exam; high level decision making; 60-74 minutes. 99205 218.21 Established patient; evaluation and management, may not require presence of physician; 99211 22.83 presenting problems are minimal Established patient; medically appropriate history/exam, straightforward decision making; 10-19 99212 55.88 minutes Established patient; medically appropriate history/exam, low level decision making; 20-29 minutes 99213 90.48 Established patient; medically appropriate history/exam, moderate level decision making; 30-39 99214 128.42 minutes Established patient; comprehensive history exam, high complex decision making; 40-54 minutes 99215 128.42 Initial comprehensive -
Agreement Between Endocervical Brush and Endocervical Curettage in Patients Undergoing Repeat Endocervical Sampling
Agreement Between Endocervical Brush and Endocervical Curettage in Patients Undergoing Repeat Endocervical Sampling Meredith J. Alston MD David W. Doo MD Sara E. Mazzoni MD MPH Elaine H. Stickrath MD Denver Health Medical Center University of Colorado Department of Obstetrics and Gynecology Background • Women with abnormal Pap tests referred for colposcopy frequently require sampling of the endocervix • ASCCP deems both the endocervical brush (ECB) and the endocervical currette (ECC) appropriate means of collecting endocervical samples (1) • Both have advantages and disadvantages, and it is unclear if one modality is superior Background • ECB has good sensitivity for endocervical lesions, it has poor specificity, ranging from 26- 38%2,3 • ECC has an excellent negative predictive value of 99.4% in women who had a satisfactory colposcopy • ECB is better tolerated by the patient, but runs the risk of contamination from the ectocervix • ECC is less likely to obtain an adequate sample Background • The results from the endocervical sample may influence clinical management after colposcopy. • Certain treatment options for high grade squamous intraepithelial neoplasia are available only to women with negative endocervical sampling. ▫ Ablative techniques ▫ Expectant management Background • Over concerns related to potential complications of excisional treatments, as well as over- treatment, there has been a push to re-introduce ablative techniques and, in appropriate clinical circumstances, expectant management, into the routine treatment of patients with cervical cancer precursors (12). Background • At our institution, it is our concern that due to the possibility of contamination from the ectocervix, a positive ECB may not represent a true positive endocervical sample. • We do not use a sleeve • Positive ECBs return for ECC if otherwise a candidate for ablative therapy or expectant management Objective • To describe the agreement between these two modalities of endocervical sampling. -

Female Pelvic Relaxation
FEMALE PELVIC RELAXATION A Primer for Women with Pelvic Organ Prolapse Written by: ANDREW SIEGEL, M.D. An educational service provided by: BERGEN UROLOGICAL ASSOCIATES N.J. CENTER FOR PROSTATE CANCER & UROLOGY Andrew Siegel, M.D. • Martin Goldstein, M.D. Vincent Lanteri, M.D. • Michael Esposito, M.D. • Mutahar Ahmed, M.D. Gregory Lovallo, M.D. • Thomas Christiano, M.D. 255 Spring Valley Avenue Maywood, N.J. 07607 www.bergenurological.com www.roboticurology.com Table of Contents INTRODUCTION .................................................................1 WHY A UROLOGIST? ..........................................................2 PELVIC ANATOMY ..............................................................4 PROLAPSE URETHRA ....................................................................7 BLADDER .....................................................................7 RECTUM ......................................................................8 PERINEUM ..................................................................9 SMALL INTESTINE .....................................................9 VAGINAL VAULT .......................................................10 UTERUS .....................................................................11 EVALUATION OF PROLAPSE ............................................11 SURGICAL REPAIR OF PELVIC PROLAPSE .....................15 STRESS INCONTINENCE .........................................16 CYSTOCELE ..............................................................18 RECTOCELE/PERINEAL LAXITY .............................19 -
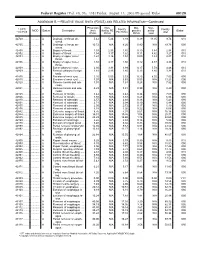
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

2019 Reimbursement Schedule IMPORTANT INFORMATION REGARDING REIMBURSEMENT by the CARE for YOURSELF PROGRAM 1
Iowa Department of Public Health Effective on or after Date of Service 01.01.2019 Division of Health Promotion Chronic Disease Prevention Iowa Care for Yourself Program 2019 Reimbursement Schedule IMPORTANT INFORMATION REGARDING REIMBURSEMENT BY THE CARE FOR YOURSELF PROGRAM 1. If a Pap test is performed, the collection of the Pap (CPT codes 99000, Q0091 & Q0111) is included in the office visit reimbursement. The woman is not to be billed for the collection or handling of the specimen. 2. These amounts apply when service is performed for the purpose of this program. Rates listed for services include all incidental charges related to the procedure; additional amounts may not be billed to the client. 3. Federal funding can not be used to reimburse for treatment of breast cancer, cervical intraepithelial neoplasia or cervical cancer. CPT Description End RATE Code OFFICE VISITS Notes 26 TC Total 99201 New Patient Visit; problem focused 3 42.90 99202 New Patient Visit; expanded problem focused 3 72.00 99203 New Patient Visit; detailed, low complexity 3 102.01 99204 New Patient Visit; comprehensive history, exam, moderate complexity 1 155.82 99205 New Patient Visit; comprehensive history, exam, high complexity 1,3 196.16 99211 Established Patient Visit, may not require presence of physician 21.35 99212 Established Patient Visit, problem focused 3,4 42.42 99213 Established Patient Visit, expanded problem focused 3,4 70.35 99214 Established Patient Visit, comprehensive moderate complexity 3,4 103.31 99215 Established Patient Visit, comprehensive high complexity 3,4 138.47 99385 New Patient Visit (18 - 39 y.o) - paid at 99203 rate 2 102.01 99386 New Patient Visit (40 - 64 y.o.) - paid at 99203 rate 2 102.01 99387 New Patient Visit (65+ y.o.) - paid at 99203 rate 2 102.01 99395 Established Patient Visit (18 - 39 y.o.) - paid at 99213 rate 2 70.35 99396 Established Patient Visit (40 - 64 y.o.) - paid at 99213 rate 2,3,4 70.35 99397 Established Patient Visit (65+ y.o.) - paid at 99213 rate 2 70.35 G0101 Cancer screening; pelvic and breast exam included. -
2012 Updated Consensus Guidelines for Managing Abnormal Cervical
2012 Updated Consensus Guidelines for the Management of Abnormal Cervical Cancer Screening Tests and Cancer Precursors L. Stewart Massad, MD, Mark H. Einstein, MD, Warner K. Huh, MD, Hormuzd A. Katki, PhD, Walter K. Kinney, MD, Mark Schiffman, MD, Diane Solomon, MD, Nicolas Wentzensen, MD, and Herschel W. Lawson, MD, for the 2012 ASCCP Consensus Guidelines Conference From Washington University School of Medicine, St. Louis, Missouri; Albert Einstein College of Medicine, New York, New York; University of Alabama School of Medicine, Birmingham, Alabama; Division of Cancer Epidemiology and Genetics and Division of Cancer Prevention, National Cancer Institute, Bethesda, Maryland; The Permanente Medical Group, Sacramento, California; and Emory University School of Medicine, Atlanta, Georgia h ABSTRACT: A group of 47 experts representing 23 Kaiser Permanente Northern California Medical Care Plan professional societies, national and international health provided evidence on risk after abnormal tests. Where data organizations, and federal agencies met in Bethesda, MD, were available, guidelines prescribed similar management September 14Y15, 2012, to revise the 2006 American Society for women with similar risks forCIN3,AIS,andcancer.Most for Colposcopy and Cervical Pathology Consensus Guidelines. prior guidelines were reaffirmed. Examples of updates in- The group’s goal was to provide revised evidence-based clude: Human papillomavirusYnegative atypical squamous consensus guidelines for managing women with abnormal cells of undetermined significance results are followed with cervical cancer screening tests, cervical intraepithelial neo- co-testing at 3 years before return to routine screening and plasia (CIN) and adenocarcinoma in situ (AIS) following are not sufficient for exiting women from screening at age adoption of cervical cancer screening guidelines incorporat- 65 years; women aged 21Y24 years need less invasive man- ing longer screening intervals and co-testing. -

OBGYN Outpatient Surgery Coding
OBGYN Outpatient Surgery Coding Anatomy Anatomy • Hyster/o – uterus, womb • Uter/o – uterus, womb • Metr/o – uterus, womb • Salping/o – tube, usually fallopian tube • Oophor/o – ovary • Ovari/o - ovary Terminology • Colpo – vagina • Cervic/o – cervix, lower part of the uterus, the “neck” • Episi/o – vulva • Vulv/o – vulva • Perine/o – the space between the anus and vulva Hysterectomy • A hysterectomy is an operation to remove a woman's uterus. • A woman may have a hysterectomy for different reasons, including: • Uterine fibroids that cause pain • bleeding, or other problems. • Uterine prolapse, which is a sliding of the uterus from its normal position into the vaginal canal. Hysterectomy • There are around 30 hysterectomy CPT codes. • To find the correct code you have to first check: • the surgical approach and • extent of the procedure. Surgical Approaches • Abdominal – the uterus is removed via an incision in the lower abdomen • Vaginal – the uterus is removed via an incision in the vagina • Laparoscopic – the procedure is performed using a laparoscope , inserted via several small incisions in the body. • Their are also CPT codes for laparoscopic-assisted vaginal approach. In this procedure ,the scope is inserted via a small incisions in the vagina. Extent of Procedure • Total hysterectomy: It includes laparoscopically detaching the entire uterine cervix and body from the surrounding supporting structures and suturing the vaginal cuff. It includes bivalving, coring, or morcellating the excised tissues, as required. The uterus is then removed through the vagina or abdomen. • Subtotal, partial or supracervical hysterectomy: It is the removal of the fundus or op portion of the uterus only, leaving the cervix in place. -

Chronic Pelvic Pain D
Guidelines on Chronic Pelvic Pain D. Engeler (Chair), A.P. Baranowski, J. Borovicka, A. Cottrell (Guidelines Associate), P. Dinis-Oliveira, S. Elneil, J. Hughes, E.J. Messelink (Vice-chair), A. van Ophoven, Y. Reisman, A.C. de C Williams © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 Aim 6 1.1.1 Structure and scope 6 1.2 Publication history 6 1.3 Panel composition 7 1.4 Methods 7 2. CHRONIC PELVIC PAIN 8 2.1 Introduction to chronic urogenital pain syndromes 8 2.2 Pain mechanisms - pain as a disease process 8 2.2.1 Ongoing peripheral visceral pain mechanisms as a cause of CPP 9 2.2.2 Central sensitisation - spinal and higher mechanisms of visceral pain 9 2.2.3 Spinal mechanisms and visceral hyperalgesia 9 2.2.4 Supraspinal modulation of pain perception 10 2.2.5 Higher centre modulation of spinal nociceptive pathways 10 2.2.6 Neuromodulation and psychology 10 2.2.7 Autonomic nervous system 10 2.2.8 Endocrine system 10 2.2.9 Genetics and chronic pain 10 2.3 Clinical paradigms and CPP 11 2.3.1 Referred pain 11 2.3.2 Referred pain to somatic tissues with hyperalgesia in the somatic tissues 11 2.3.3 Muscles and pelvic pain 11 2.3.4 Visceral hyperalgesia 11 2.3.5 Viscero-visceral hyperalgesia 11 2.4 Classification of CPP syndromes 12 2.4.1 Importance of classification 12 2.4.2 Pain syndromes 14 2.4.2.1 Definition of chronic pelvic pain (CPP) 14 2.4.2.2 Definition of chronic pelvic pain syndrome 14 2.4.2.2.1 Further subdivision of CPPS 14 2.4.2.2.2 Psychological considerations for classification 14 2.4.2.2.3 Functional considerations for classification 15 2.5.2.2.4 Multisystem subdivision 15 2.4.2.2.5 Dyspareunia 15 2.4.2.2.6 Perineal pain syndrome 15 2.5 Conclusions and recommendations: CPP and mechanisms 15 2.6 An algorithm for CPP diagnosis and treatment 16 3. -

Pelviperineology September 2017
71-73 PETROS ANZJOG.qxp_severe 31/08/17 11:59 Pagina 71 Original article Acknowledgment: This paper is reprinted by permission of the ANZJOG journal. Aust. NZ J 0bst. Gynaecol 1996; 36: 3: 351-354 Severe chronic pelvic pain in women may be caused by ligamentous laxity in the posterior fornix of the vagina PETER P. PETROS, D Med Sc, FRCOG, FRACOG, CU Department of Gynaecology, Royal Perth Hospital, Western Australia Summary: The aim was to prospectively study the relationship between pelvic pain of otherwise unknown origin and laxity in the posterior vaginal fornix. Twenty-eight patients with negative laparoscopy findings, lower abdominal pain and laxity in the posterior ligamentous sup - ports of the uterus underwent surgical approximation of their uterosacral ligaments. At 3-month review, 85% of patients were cured, and at 12 months, 70%. Nonorganic pelvic pain has frequently been attributed to psychological factors. However, the results suggest that this may be a T12-Ll sympathetic pain referred to the lower abdomen, perhaps due to the force of gravity stimulating pain nerves unable to be sup - ported by the lax uterosacral ligaments in which they are contained. It was concluded that laxity in the posterior ligaments of the vagina should first be excluded before referring patients with pelvic floor discomfort or pain for psychiatric care. Key words: Chronic pelvic pain; Uterosacral ligaments; Surgical cure. INTRODUCTION Exclusion criteria. Known causes of pelvic pain such as Historically, laxity in the ligamentous supports of the chronic pelvic inflammatory disease, or endometriosis were 1 excluded by prior laparoscopy. uterus has been described as a cause of pelvic pain . -
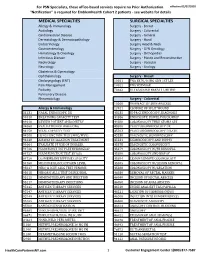
Services Not Requiring Prior Authorization for PSN Specialists
For PSN Specialists, these office-based services require no Prior Authorization. effective 02/07/2020 "Notification" is required for EmblemHealth Cohort 2 patients - see website for details MEDICAL SPECIALTIES SURGICAL SPECIALTIES Allergy & Immunology Surgery - Breast Audiology Surgery - Colorectal Cardiovascular Disease Surgery - General Dermatology & Dermatopathology Surgery - Hand Endocrinology Surgery Head & Neck Gastroenterology Surgery - GYN Oncology Hematology & Oncology Surgery - Orthopedics Infectious Disease Surgery - Plastic and Reconstructive Nephrology Surgery - Vascular Neurology Surgery - Urology Obstetrics & Gynecology Ophthalmology Surgery - Breast Otolaryngology (ENT) 10021 FNA BX W/O IMG GDN 1ST LES Pain Management 10022 FNA W/IMAGE Podiatry 76642 ULTRASOUND BREAST LIMITED Pulmonary Disease Rheumatology Surgery - Colorectal 10060 DRAINAGE OF SKIN ABSCESS Allergy & Immunology 12021 CLOSURE OF SPLIT WOUND 31231 NASAL ENDOSCOPY, DX 43235 UPPR GI ENDOSCOPY, DIAGNOSIS 94010 BREATHING CAPACITY TEST 44386 ENDOSCOPY, BOWEL POUCH/BIOP 94016 REVIEW PATIENT SPIROMETRY 44388 COLONOSCOPY THRU STOMA SPX 94060 EVALUATION OF WHEEZING 45300 PROCTOSIGMOIDOSCOPY DX 94150 VITAL CAPACITY TEST 45303 PROCTOSIGMOIDOSCOPY DILATE 94200 LUNG FUNCTION TEST (MBC/MVV) 45330 DIAGNOSTIC SIGMOIDOSCOPY 94640 AIRWAY INHALATION TREATMENT 45331 SIGMOIDOSCOPY AND BIOPSY 94664 EVALUATE PT USE OF INHALER 45378 DIAGNOSTIC COLONOSCOPY 94726 PULM FUNCT TST PLETHYSMOGRAP 45379 COLONOSCOPY W/FB REMOVAL 94727 PULM FUNCTION TEST BY GAS 45380 COLONOSCOPY AND BIOPSY