Hysterectomy Medical Policy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Controversies and Complications in Pelvic Reconstructive Surgery (Didactic)
Controversies and Complications in Pelvic Reconstructive Surgery (Didactic) PROGRAM CHAIR Andrew I. Sokol, MD Cheryl B. Iglesia, MD Charles R. Rardin, MD Sponsored by AAGL Advancing Minimally Invasive Gynecology Worldwide Professional Education Information Target Audience Educational activities are developed to meet the needs of surgical gynecologists in practice and in training, as well as, other allied healthcare professionals in the field of gynecology. Accreditation AAGL is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. The AAGL designates this live activity for a maximum of 3.75 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. DISCLOSURE OF RELEVANT FINANCIAL RELATIONSHIPS As a provider accredited by the Accreditation Council for Continuing Medical Education, AAGL must ensure balance, independence, and objectivity in all CME activities to promote improvements in health care and not proprietary interests of a commercial interest. The provider controls all decisions related to identification of CME needs, determination of educational objectives, selection and presentation of content, selection of all persons and organizations that will be in a position to control the content, selection of educational methods, and evaluation of the activity. Course chairs, planning committee members, presenters, authors, moderators, panel members, and others in a position to control the content of this activity are required to disclose relevant financial relationships with commercial interests related to the subject matter of this educational activity. Learners are able to assess the potential for commercial bias in information when complete disclosure, resolution of conflicts of interest, and acknowledgment of commercial support are provided prior to the activity. -

Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021
Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021 INDIVIDUAL MARKETPLACE | PROMEDICA MEDICARE PLAN | PPO GUIDELINES This policy does not certify benefits or authorization of benefits, which is designated by each individual policyholder terms, conditions, exclusions and limitations contract. It does not constitute a contract or guarantee regarding coverage or reimbursement/payment. Self-Insured group specific policy will supersede this general policy when group supplementary plan document or individual plan decision directs otherwise. Paramount applies coding edits to all medical claims through coding logic software to evaluate the accuracy and adherence to accepted national standards. This medical policy is solely for guiding medical necessity and explaining correct procedure reporting used to assist in making coverage decisions and administering benefits. SCOPE X Professional X Facility DESCRIPTION Transgender is a broad term that can be used to describe people whose gender identity is different from the gender they were thought to be when they were born. Gender dysphoria (GD) or gender identity disorder is defined as evidence of a strong and persistent cross-gender identification, which is the desire to be, or the insistence that one is of the other gender. Persons with this disorder experience a sense of discomfort and inappropriateness regarding their anatomic or genetic sexual characteristics. Individuals with GD have persistent feelings of gender discomfort and inappropriateness of their anatomical sex, strong and ongoing cross-gender identification, and a desire to live and be accepted as a member of the opposite sex. Gender Dysphoria (GD) is defined by the Diagnostic and Statistical Manual of Mental Disorders - Fifth Edition, DSM-5™ as a condition characterized by the "distress that may accompany the incongruence between one’s experienced or expressed gender and one’s assigned gender" also known as “natal gender”, which is the individual’s sex determined at birth. -

Female Pelvic Relaxation
FEMALE PELVIC RELAXATION A Primer for Women with Pelvic Organ Prolapse Written by: ANDREW SIEGEL, M.D. An educational service provided by: BERGEN UROLOGICAL ASSOCIATES N.J. CENTER FOR PROSTATE CANCER & UROLOGY Andrew Siegel, M.D. • Martin Goldstein, M.D. Vincent Lanteri, M.D. • Michael Esposito, M.D. • Mutahar Ahmed, M.D. Gregory Lovallo, M.D. • Thomas Christiano, M.D. 255 Spring Valley Avenue Maywood, N.J. 07607 www.bergenurological.com www.roboticurology.com Table of Contents INTRODUCTION .................................................................1 WHY A UROLOGIST? ..........................................................2 PELVIC ANATOMY ..............................................................4 PROLAPSE URETHRA ....................................................................7 BLADDER .....................................................................7 RECTUM ......................................................................8 PERINEUM ..................................................................9 SMALL INTESTINE .....................................................9 VAGINAL VAULT .......................................................10 UTERUS .....................................................................11 EVALUATION OF PROLAPSE ............................................11 SURGICAL REPAIR OF PELVIC PROLAPSE .....................15 STRESS INCONTINENCE .........................................16 CYSTOCELE ..............................................................18 RECTOCELE/PERINEAL LAXITY .............................19 -

Oophorectomy Or Salpingectomy— Which Makes More Sense?
Oophorectomy or salpingectomy— which makes more sense? During hysterectomy for benign indications, many surgeons routinely remove the ovaries to prevent cancer. Here’s what we know about this practice. William H. Parker, MD CASE Patient opts for hysterectomy, asks than age 45 to prevent the subsequent devel- about oophorectomy opment of ovarian cancer (FIGURES 1 and 2). Your 46-year-old patient reports increasingly The 2002 Women’s Health Initiative re- severe dysmenorrhea at her annual visit, and a port suggested that exogenous hormone use pelvic examination reveals an enlarged uterus. was associated with a slight increase in the You order pelvic magnetic resonance imaging, risk of breast cancer.2 After its publication, which shows extensive adenomyosis. the rate of oophorectomy at the time of hys- After you counsel the patient about terectomy declined slightly, likely reflect- IN THIS her options, she elects to undergo lapa- ARTICLE ing women’s desire to preserve their own roscopic supracervical hysterectomy and source of estrogen.3 For women younger Algorithm: Should asks whether she should have her ovaries than age 50, further slight declines in the rate the ovaries removed at the time of surgery. She has no of oophorectomy were seen from 2002 to be removed? family history of ovarian or breast cancer. 2010. However, in the United States, almost page 54 What would you recommend for this 300,000 women still undergo “prophylactic” woman, based on her situation and current bilateral salpingo-oophorectomy every year.4 medical research? The lifetime risk of ovarian cancer Ovarian cancer does among women with a BRCA 1 mutation not come from the prophylactic procedure should be is 36% to 46%, and it is 10% to 27% among ovary considered only if 1) there is a rea- women with a BRCA 2 mutation. -

Salpingectomy for Ovarian Cancer Prevention Approved 11/9/2017
Health Evidence Review Commission (HERC) Coverage Guidance: Opportunistic Salpingectomy for Ovarian Cancer Prevention Approved 11/9/2017 HERC Coverage Guidance Opportunistic salpingectomy during gynecological procedures is recommended for coverage, without an increased payment (i.e., using a form of reference-based pricing) (weak recommendation). Note: Definitions for strength of recommendation are in Appendix A. GRADE Informed Framework Element Description. Table of Contents HERC Coverage Guidance ............................................................................................................................. 1 Rationale for development of coverage guidances and multisector intervention reports .......................... 3 GRADE-Informed Framework ....................................................................................................................... 4 Should opportunistic salpingectomy be recommended for coverage for ovarian cancer risk reduction? .................................................................................................................................................................. 4 Clinical Background ....................................................................................................................................... 7 Indications ................................................................................................................................................. 7 Technology Description ........................................................................................................................... -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -

Obstetrics and Gyneclogy
3/28/2016 Obstetrics and Gynecology Presented by: Peggy Stilley, CPC, CPC-I, CPMA, CPB, COBGC Objectives • Procedures • Pregnancy • Payments • Patient Relationships 1 3/28/2016 Female Genital Anatomy Terminology and Abbreviations • Endometriosis • Neoplasm • BUS • TAH/BSO • G3P2 2 3/28/2016 Procedures • Hysterectomy • Prolapse repairs • IUDs • Colposcopy Hysterectomy • Approach • Open • Vaginal • Total Laparoscopic • Laparoscopic assisted • Extent • Total • Subtotal • Supracervical • Diagnosis 3 3/28/2016 CPT Codes • Abdominal 58150 – • With or without removal tubes/ovaries 58240 • Some additional services • Vaginal 58260-58270 • Size of uterus < 250 grams, > 250 grams 58275-58294 • Additional services CPT Codes • LAVH 58541-58544 • Detach uterus , cervix, and structures through the scope 58548-58554 • Uterus removed thru the vagina • TLH • Detach structures laparoscopically entire 58570- 58573 uterus, cervix, bodies • Removed thru the vagina or abdomen • LSH • Detaching structures through the scope, 58541 – 58544 leaving the cervix • Morcellating – removing abdominally 4 3/28/2016 Hysterectomy Additional procedures performed • Tubes & Ovaries removed • Enterocele repair • Repairs for incontinence • Marshall-Marchetti-Krantz • Colporrhaphy • Colpo-urethropexy • Urethral Sling • TVT, TOT 5 3/28/2016 Procedures • 57288 Sling • 57240 Anterior Repair • 57250 Posterior Repair • +57267 Add on code for mesh/graft • 57260 Combo of A&P • 57425 Laparoscopic Colpopexy • 57280 Colpopexy, Abdominal approach • 57282 Colpopexy, vaginal approach Example 1 PREOPERATIVE DIAGNOSES: 1. Menorrhagia unresponsive to medical treatment with resulting chronic blood loss anemia POSTOPERATIVE DIAGNOSES: 1. Menorrhagia 2. Blood loss anemia TITLE OF SURGERY: Total abdominal hysterectomy ANESTHESIA: GENERAL ENDOTRACHEAL ANESTHESIA. INDICATIONS: The patient is a lovely 52-year-old female who presented with menorrhagia that is non- responsive to medical treatment. -
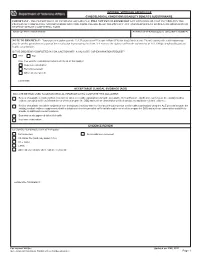
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

(8Th Edition) Procedure Code ACHI (8
Appendix 1. Procedure and Diagnostic Codes Used to Identify Prior Procedures Procedure ACHI (8th ACHI (8th edition) procedure names ICD-10- ICD-10-AM edition) AM diagnosis name procedure diagnosis code code Gynecological laparoscopy 35638-00 Laparoscopic wedge resection of ovary 35638-01 Laparoscopic partial oophorectomy 35638-02 Laparoscopic oophorectomy, unilateral 35638-03 Laparoscopic oophorectomy,bilateral 35638-04 Laparoscopic ovarian cystectomy, unilateral 35638-05 Laparoscopic ovarian cystectomy, bilateral 35638-06 Laparoscopic salpingotomy 35638-07 Laparoscopic partial salpingectomy, unilateral 35638-08 Laparoscopic partial salpingectomy, bilateral 35638-09 Laparoscopic salpingectomy, unilateral 35638-10 Laparoscopic salpingectomy, bilateral 35638-11 Laparoscopic salpingo-oophorectomy, unilateral 35638-12 Laparoscopic salpingo-oophorectomy, bilateral 35638-14 Laparoscopic uterosacral nerve ablation 35637-02 Laparoscopic diathermy of lesion of pelvic cavity 35637-04 Laparoscopic ventrosuspension 35637-07 Laparoscopic rupture of ovarian cyst or abscess 35637-08 Laparoscopic ovarian drilling 35637-10 Laparoscopic excision of lesion of pelvic cavity 35729-00 Laparoscopic transposition of ovary 90430-00 Laparoscopic repair of ovary 90433-00 Other laparoscopic repair of fallopian tube 35694-00 Laparoscopic salpingoplasty 35694-01 Laparoscopic anastomosis of fallopian tube 35694-02 Laparoscopic salpingolysis 35694-03 Laparoscopic salpingostomy 35694-06 Laparoscopic salpingotomy 35649-01* Myomectomy of uterus via laparoscopy Hysteroscopy, including operative hysteroscopy 35630-00 Diagnostic hysteroscopy 35649-00 Hysterotomy 35633-00 Division of uterine adhesions 35634-00 Division of uterine septum via hysteroscopy 35649-02 Division of uterine septum via hysterotomy 35633-01 Polypectomy of uterus via hysteroscopy 35623-00 Myomectomy of uterus via hysteroscopy Baldwin HJ, Patterson JA, Nippita TA, Torvaldsen S, Ibiebele I, Simpson JM, et al. Antecedents of abnormally invasive placenta in primiparous women: the risk from gynecologic procedures. -

Sex Reassignment Surgery Page 1 of 14
Sex Reassignment Surgery Page 1 of 14 Medical Policy An Independent licensee of the Blue Cross Blue Shield Association Title: Sex Reassignment Surgery PRE-DETERMINATION of services is not required, but is highly recommended. http://www.bcbsks.com/CustomerService/Forms/pdf/15-17_predeterm_request_frm.pdf Professional Institutional Original Effective Date: January 1, 2017 Original Effective Date: January 1, 2017 Revision Date(s): January 1, 2017; Revision Date(s): January 1, 2017; January 27, 2021; March 18, 2021 January 27, 2021; March 18, 2021 Current Effective Date: January 1, 2017 Current Effective Date: January 1, 2017 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. DESCRIPTION Gender dysphoria involves a conflict between a person's physical or assigned gender and the gender with which he/she/they identify. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Prophylactic Oophorectomy Or Salpingo- Oophorectomy with Or Without Hysterectomy
Medical Coverage Policy Effective Date ............................................. 2/15/2019 Next Review Date ....................................... 2/15/2020 Coverage Policy Number .................................. 0026 Prophylactic Oophorectomy or Salpingo- oophorectomy With or Without Hysterectomy Table of Contents Related Coverage Resources Coverage Policy ................................................... 1 Colorectal Cancer Screening and Surveillance Overview .............................................................. 2 Genetic Testing for Hereditary Cancer Susceptibility General Background ............................................ 2 Syndromes Coding/Billing Information .................................... 6 Genetic Testing for Hereditary and Multifactorial Conditions References .......................................................... 7 Prophylactic Mastectomy INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD)