Gynecological Disorders Objectives at the End of This Lecture the Student
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Female Pelvic Relaxation
FEMALE PELVIC RELAXATION A Primer for Women with Pelvic Organ Prolapse Written by: ANDREW SIEGEL, M.D. An educational service provided by: BERGEN UROLOGICAL ASSOCIATES N.J. CENTER FOR PROSTATE CANCER & UROLOGY Andrew Siegel, M.D. • Martin Goldstein, M.D. Vincent Lanteri, M.D. • Michael Esposito, M.D. • Mutahar Ahmed, M.D. Gregory Lovallo, M.D. • Thomas Christiano, M.D. 255 Spring Valley Avenue Maywood, N.J. 07607 www.bergenurological.com www.roboticurology.com Table of Contents INTRODUCTION .................................................................1 WHY A UROLOGIST? ..........................................................2 PELVIC ANATOMY ..............................................................4 PROLAPSE URETHRA ....................................................................7 BLADDER .....................................................................7 RECTUM ......................................................................8 PERINEUM ..................................................................9 SMALL INTESTINE .....................................................9 VAGINAL VAULT .......................................................10 UTERUS .....................................................................11 EVALUATION OF PROLAPSE ............................................11 SURGICAL REPAIR OF PELVIC PROLAPSE .....................15 STRESS INCONTINENCE .........................................16 CYSTOCELE ..............................................................18 RECTOCELE/PERINEAL LAXITY .............................19 -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -

Obstetrics and Gyneclogy
3/28/2016 Obstetrics and Gynecology Presented by: Peggy Stilley, CPC, CPC-I, CPMA, CPB, COBGC Objectives • Procedures • Pregnancy • Payments • Patient Relationships 1 3/28/2016 Female Genital Anatomy Terminology and Abbreviations • Endometriosis • Neoplasm • BUS • TAH/BSO • G3P2 2 3/28/2016 Procedures • Hysterectomy • Prolapse repairs • IUDs • Colposcopy Hysterectomy • Approach • Open • Vaginal • Total Laparoscopic • Laparoscopic assisted • Extent • Total • Subtotal • Supracervical • Diagnosis 3 3/28/2016 CPT Codes • Abdominal 58150 – • With or without removal tubes/ovaries 58240 • Some additional services • Vaginal 58260-58270 • Size of uterus < 250 grams, > 250 grams 58275-58294 • Additional services CPT Codes • LAVH 58541-58544 • Detach uterus , cervix, and structures through the scope 58548-58554 • Uterus removed thru the vagina • TLH • Detach structures laparoscopically entire 58570- 58573 uterus, cervix, bodies • Removed thru the vagina or abdomen • LSH • Detaching structures through the scope, 58541 – 58544 leaving the cervix • Morcellating – removing abdominally 4 3/28/2016 Hysterectomy Additional procedures performed • Tubes & Ovaries removed • Enterocele repair • Repairs for incontinence • Marshall-Marchetti-Krantz • Colporrhaphy • Colpo-urethropexy • Urethral Sling • TVT, TOT 5 3/28/2016 Procedures • 57288 Sling • 57240 Anterior Repair • 57250 Posterior Repair • +57267 Add on code for mesh/graft • 57260 Combo of A&P • 57425 Laparoscopic Colpopexy • 57280 Colpopexy, Abdominal approach • 57282 Colpopexy, vaginal approach Example 1 PREOPERATIVE DIAGNOSES: 1. Menorrhagia unresponsive to medical treatment with resulting chronic blood loss anemia POSTOPERATIVE DIAGNOSES: 1. Menorrhagia 2. Blood loss anemia TITLE OF SURGERY: Total abdominal hysterectomy ANESTHESIA: GENERAL ENDOTRACHEAL ANESTHESIA. INDICATIONS: The patient is a lovely 52-year-old female who presented with menorrhagia that is non- responsive to medical treatment. -
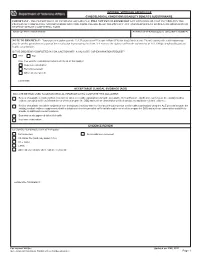
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

Grading Pelvic Prolapse and Pelvic Floor Relaxation Using Dynamic Magnetic Resonance Imaging
ADULT UROLOGY GRADING PELVIC PROLAPSE AND PELVIC FLOOR RELAXATION USING DYNAMIC MAGNETIC RESONANCE IMAGING CRAIG V. COMITER, SANDIP P. VASAVADA, ZORAN L. BARBARIC, ANGELO E. GOUSSE, AND SHLOMO RAZ ABSTRACT Objectives. With significant vaginal prolapse, it is often difficult to differentiate among cystocele, enterocele, and high rectocele by physical examination alone. Our group has previously demonstrated the utility of magnetic resonance imaging (MRI) for evaluating pelvic prolapse. We describe a simple objective grading system for quantifying pelvic floor relaxation and prolapse. Methods. One hundred sixty-four consecutive women presenting with pelvic pain (n ϭ 39) or organ prolapse (n ϭ 125) underwent dynamic MRI. The “H-line” (levator hiatus) measures the distance from the pubis to the posterior anal canal. The “M-line” (muscular pelvic floor relaxation) measures the descent of the levator plate from the pubococcygeal line. The “O” classification (organ prolapse) characterizes the degree of visceral prolapse beyond the H-line. Results. The image acquisition time was 2.5 minutes per study. Each study cost $540. In the pain group, the H-line averaged 5.2 Ϯ 1.1 cm versus 7.5 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). The M-line averaged 1.9 Ϯ 1.2 cm in the pain group versus 4.1 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). Incidental pelvic pathologic features were commonly noted, including uterine fibroids, ovarian cysts, hydroureter, urethral diverticula, and foreign body. Conclusions. The HMO classification provides a straightforward and reproducible method for staging and quantifying pelvic floor relaxation and visceral prolapse. -

OBGYN Outpatient Surgery Coding
OBGYN Outpatient Surgery Coding Anatomy Anatomy • Hyster/o – uterus, womb • Uter/o – uterus, womb • Metr/o – uterus, womb • Salping/o – tube, usually fallopian tube • Oophor/o – ovary • Ovari/o - ovary Terminology • Colpo – vagina • Cervic/o – cervix, lower part of the uterus, the “neck” • Episi/o – vulva • Vulv/o – vulva • Perine/o – the space between the anus and vulva Hysterectomy • A hysterectomy is an operation to remove a woman's uterus. • A woman may have a hysterectomy for different reasons, including: • Uterine fibroids that cause pain • bleeding, or other problems. • Uterine prolapse, which is a sliding of the uterus from its normal position into the vaginal canal. Hysterectomy • There are around 30 hysterectomy CPT codes. • To find the correct code you have to first check: • the surgical approach and • extent of the procedure. Surgical Approaches • Abdominal – the uterus is removed via an incision in the lower abdomen • Vaginal – the uterus is removed via an incision in the vagina • Laparoscopic – the procedure is performed using a laparoscope , inserted via several small incisions in the body. • Their are also CPT codes for laparoscopic-assisted vaginal approach. In this procedure ,the scope is inserted via a small incisions in the vagina. Extent of Procedure • Total hysterectomy: It includes laparoscopically detaching the entire uterine cervix and body from the surrounding supporting structures and suturing the vaginal cuff. It includes bivalving, coring, or morcellating the excised tissues, as required. The uterus is then removed through the vagina or abdomen. • Subtotal, partial or supracervical hysterectomy: It is the removal of the fundus or op portion of the uterus only, leaving the cervix in place. -

Male Infertility
Guidelines on Male Infertility A. Jungwirth, T. Diemer, G.R. Dohle, A. Giwercman, Z. Kopa, C. Krausz, H. Tournaye © European Association of Urology 2012 TABLE OF CONTENTS PAGE 1. METHODOLOGY 6 1.1 Introduction 6 1.2 Data identification 6 1.3 Level of evidence and grade of recommendation 6 1.4 Publication history 7 1.5 Definition 7 1.6 Epidemiology and aetiology 7 1.7 Prognostic factors 8 1.8 Recommendations on epidemiology and aetiology 8 1.9 References 8 2. INVESTIGATIONS 9 2.1 Semen analysis 9 2.1.1 Frequency of semen analysis 9 2.2 Recommendations for investigations in male infertility 10 2.3 References 10 3. TESTICULAR DEFICIENCY (SPERMATOGENIC FAILURE) 10 3.1 Definition 10 3.2 Aetiology 10 3.3 Medical history and physical examination 11 3.4 Investigations 11 3.4.1 Semen analysis 11 3.4.2 Hormonal determinations 11 3.4.3 Testicular biopsy 11 3.5 Conclusions and recommendations for testicular deficiency 12 3.6 References 12 4. GENETIC DISORDERS IN INFERTILITY 14 4.1 Introduction 14 4.2 Chromosomal abnormalities 14 4.2.1 Sperm chromosomal abnormalities 14 4.2.2 Sex chromosome abnormalities 14 4.2.3 Autosomal abnormalities 15 4.3 Genetic defects 15 4.3.1 X-linked genetic disorders and male fertility 15 4.3.2 Kallmann syndrome 15 4.3.3 Mild androgen insensitivity syndrome 15 4.3.4 Other X-disorders 15 4.4 Y chromosome and male infertility 15 4.4.1 Introduction 15 4.4.2 Clinical implications of Y microdeletions 16 4.4.2.1 Testing for Y microdeletions 17 4.4.2.2 Y chromosome: ‘gr/gr’ deletion 17 4.4.2.3 Conclusions 17 4.4.3 Autosomal defects with severe phenotypic abnormalities and infertility 17 4.5 Cystic fibrosis mutations and male infertility 18 4.6 Unilateral or bilateral absence/abnormality of the vas and renal anomalies 18 4.7 Unknown genetic disorders 19 4.8 DNA fragmentation in spermatozoa 19 4.9 Genetic counselling and ICSI 19 4.10 Conclusions and recommendations for genetic disorders in male infertility 19 4.11 References 20 5. -

Chronic Pelvic Pain D
Guidelines on Chronic Pelvic Pain D. Engeler (Chair), A.P. Baranowski, J. Borovicka, A. Cottrell (Guidelines Associate), P. Dinis-Oliveira, S. Elneil, J. Hughes, E.J. Messelink (Vice-chair), A. van Ophoven, Y. Reisman, A.C. de C Williams © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 Aim 6 1.1.1 Structure and scope 6 1.2 Publication history 6 1.3 Panel composition 7 1.4 Methods 7 2. CHRONIC PELVIC PAIN 8 2.1 Introduction to chronic urogenital pain syndromes 8 2.2 Pain mechanisms - pain as a disease process 8 2.2.1 Ongoing peripheral visceral pain mechanisms as a cause of CPP 9 2.2.2 Central sensitisation - spinal and higher mechanisms of visceral pain 9 2.2.3 Spinal mechanisms and visceral hyperalgesia 9 2.2.4 Supraspinal modulation of pain perception 10 2.2.5 Higher centre modulation of spinal nociceptive pathways 10 2.2.6 Neuromodulation and psychology 10 2.2.7 Autonomic nervous system 10 2.2.8 Endocrine system 10 2.2.9 Genetics and chronic pain 10 2.3 Clinical paradigms and CPP 11 2.3.1 Referred pain 11 2.3.2 Referred pain to somatic tissues with hyperalgesia in the somatic tissues 11 2.3.3 Muscles and pelvic pain 11 2.3.4 Visceral hyperalgesia 11 2.3.5 Viscero-visceral hyperalgesia 11 2.4 Classification of CPP syndromes 12 2.4.1 Importance of classification 12 2.4.2 Pain syndromes 14 2.4.2.1 Definition of chronic pelvic pain (CPP) 14 2.4.2.2 Definition of chronic pelvic pain syndrome 14 2.4.2.2.1 Further subdivision of CPPS 14 2.4.2.2.2 Psychological considerations for classification 14 2.4.2.2.3 Functional considerations for classification 15 2.5.2.2.4 Multisystem subdivision 15 2.4.2.2.5 Dyspareunia 15 2.4.2.2.6 Perineal pain syndrome 15 2.5 Conclusions and recommendations: CPP and mechanisms 15 2.6 An algorithm for CPP diagnosis and treatment 16 3. -

Pelviperineology September 2017
71-73 PETROS ANZJOG.qxp_severe 31/08/17 11:59 Pagina 71 Original article Acknowledgment: This paper is reprinted by permission of the ANZJOG journal. Aust. NZ J 0bst. Gynaecol 1996; 36: 3: 351-354 Severe chronic pelvic pain in women may be caused by ligamentous laxity in the posterior fornix of the vagina PETER P. PETROS, D Med Sc, FRCOG, FRACOG, CU Department of Gynaecology, Royal Perth Hospital, Western Australia Summary: The aim was to prospectively study the relationship between pelvic pain of otherwise unknown origin and laxity in the posterior vaginal fornix. Twenty-eight patients with negative laparoscopy findings, lower abdominal pain and laxity in the posterior ligamentous sup - ports of the uterus underwent surgical approximation of their uterosacral ligaments. At 3-month review, 85% of patients were cured, and at 12 months, 70%. Nonorganic pelvic pain has frequently been attributed to psychological factors. However, the results suggest that this may be a T12-Ll sympathetic pain referred to the lower abdomen, perhaps due to the force of gravity stimulating pain nerves unable to be sup - ported by the lax uterosacral ligaments in which they are contained. It was concluded that laxity in the posterior ligaments of the vagina should first be excluded before referring patients with pelvic floor discomfort or pain for psychiatric care. Key words: Chronic pelvic pain; Uterosacral ligaments; Surgical cure. INTRODUCTION Exclusion criteria. Known causes of pelvic pain such as Historically, laxity in the ligamentous supports of the chronic pelvic inflammatory disease, or endometriosis were 1 excluded by prior laparoscopy. uterus has been described as a cause of pelvic pain . -

SJH Procedures
SJH Procedures - Gynecology and Gynecology Oncology Services New Name Old Name CPT Code Service ABLATION, LESION, CERVIX AND VULVA, USING CO2 LASER LASER VAPORIZATION CERVIX/VULVA W CO2 LASER 56501 Destruction of lesion(s), vulva; simple (eg, laser surgery, Gynecology electrosurgery, cryosurgery, chemosurgery) 56515 Destruction of lesion(s), vulva; extensive (eg, laser surgery, Gynecology electrosurgery, cryosurgery, chemosurgery) 57513 Cautery of cervix; laser ablation Gynecology BIOPSY OR EXCISION, LESION, FACE AND NECK EXCISION/BIOPSY (MASS/LESION/LIPOMA/CYST) FACE/NECK General, Gynecology, Plastics, ENT, Maxillofacial BIOPSY OR EXCISION, LESION, FACE AND NECK, 2 OR MORE EXCISE/BIOPSY (MASS/LESION/LIPOMA/CYST) MULTIPLE FACE/NECK 11102 Tangential biopsy of skin (eg, shave, scoop, saucerize, curette); General, Gynecology, single lesion Aesthetics, Urology, Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11103 Tangential biopsy of skin (eg, shave, scoop, saucerize, curette); General, Gynecology, each separate/additional lesion (list separately in addition to Aesthetics, Urology, code for primary procedure) Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11104 Punch biopsy of skin (including simple closure, when General, Gynecology, performed); single lesion Aesthetics, Urology, Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11105 Punch biopsy of skin (including simple closure, when General, Gynecology, performed); each separate/additional lesion -

Female Chronic Pelvic Pain Syndromes 1 Standard of Care
BRIGHAM AND WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: Female Chronic Pelvic Pain Syndromes ICD 9 Codes: 719.45 Pain in the pelvic region 625.9 Vulvar/pelvic pain/vulvodynia/vestibulodynia (localized provoked vestibulodynia or unprovoked) 625.0 Dyspareunia 595.1 Interstitial cystitis/painful bladder syndrome 739.5 Pelvic floor dysfunction 569.42 Anal/rectal pain 564.6 Proctalgia fugax/spasm anal sphincter 724.79 Coccygodynia 781.3 Muscular incoordination (other possible pain diagnoses: prolapse 618.0) Case Type/Diagnosis: Chronic pelvic pain (CPP) can be defined as: “non-malignant pain perceived in structures related to the pelvis, in the anterior abdominal wall below the level of the umbilicus, the spine from T10 (ovarian nerve supply) or T12 (nerve supply to pelvic musculoskeletal structures) to S5, the perineum, and all external and internal tissues within these reference zones”. 1 Specifically, pelvic pain syndrome has been further defined as: “the occurrence of persistent or recurrent episodic pelvic pain associated with symptoms suggestive of lower urinary tract, sexual, bowel or gynecological dysfunction with no proven infection or other obvious pathology”.1 Generally, female pelvic pain has been defined as pain and dysfunction in and around the pelvic outlet, specifically the suprapubic, vulvar, and anal regions. A plethora of various terms/diagnoses encompass pelvic pain as a symptom, including but not limited to: chronic pelvic pain (CPP), vulvar pain, vulvodynia, vestibulitis/vestibulodynia (localized provoked vestibulodynia or unprovoked vestibulodynia), vaginismus, dyspareunia, interstitial cystitis (IC)/painful bladder syndrome (PBS), proctalgia fugax, levator ani syndrome, pelvic floor dysfunction, vulvodynia, vestibulitis/vestibulodynia dyspareunia, vaginismus, coccygodynia, levator ani syndrome, tension myaglia of the pelvic floor, shortened pelvic floor, and muscular incoordination of the pelvic floor muscles. -

Vaginal Reconstruction/Sling Urethropexy)
Patient Name: _ Date: _ New Jersey Urologic Institute Dr Betsy Greenleaf DO, FACOOG Pelvic Medicine and Reconstructive Surgery 10Industrial Way East, Suite 101, Eatontown, New Jersey 07724 732-963-9091 Fax: 732-963-9092 Findings: _ Post Operative Instructions (Vaginal Reconstruction/Sling Urethropexy) 1. Activity: May do as much as you feel up to. Your body will let you know when you are doing too much. Don't push yourself, however. Walking is ok and encouraged. If you sit too long you will become stiff and it will make it more difficult to move. Lying around can promote the formation of blood clots that can be life threatening. It is therefore important to move around. If you don't feel like walking, at least move your legs around in bed from time to time. Stairs are ok, just be careful of standing up too quickly and becoming light headed. Sitting still can also increase your risk of pneumonia. In addition to moving around, practice taking deep breaths ( 10 times each every hour or so) to keep your lungs properly aerated. Limitations: Avoid lifting or pushing/pulling any objects heavier than 1Olbs for at least 3 months. For patients with pelvic hernia or prolapse repairs it is recommended not to lift objects heavier than 25 Ibs for life. This may seem unrealistic. Try to put off lifting as long as possible. If you must lift, do not hold your breathe. Blow out as you lift to decrease abdominal and pelvic pressure. Also be aware that if you choose to lift objects heavier than recommended you risk forming another hernia 2.