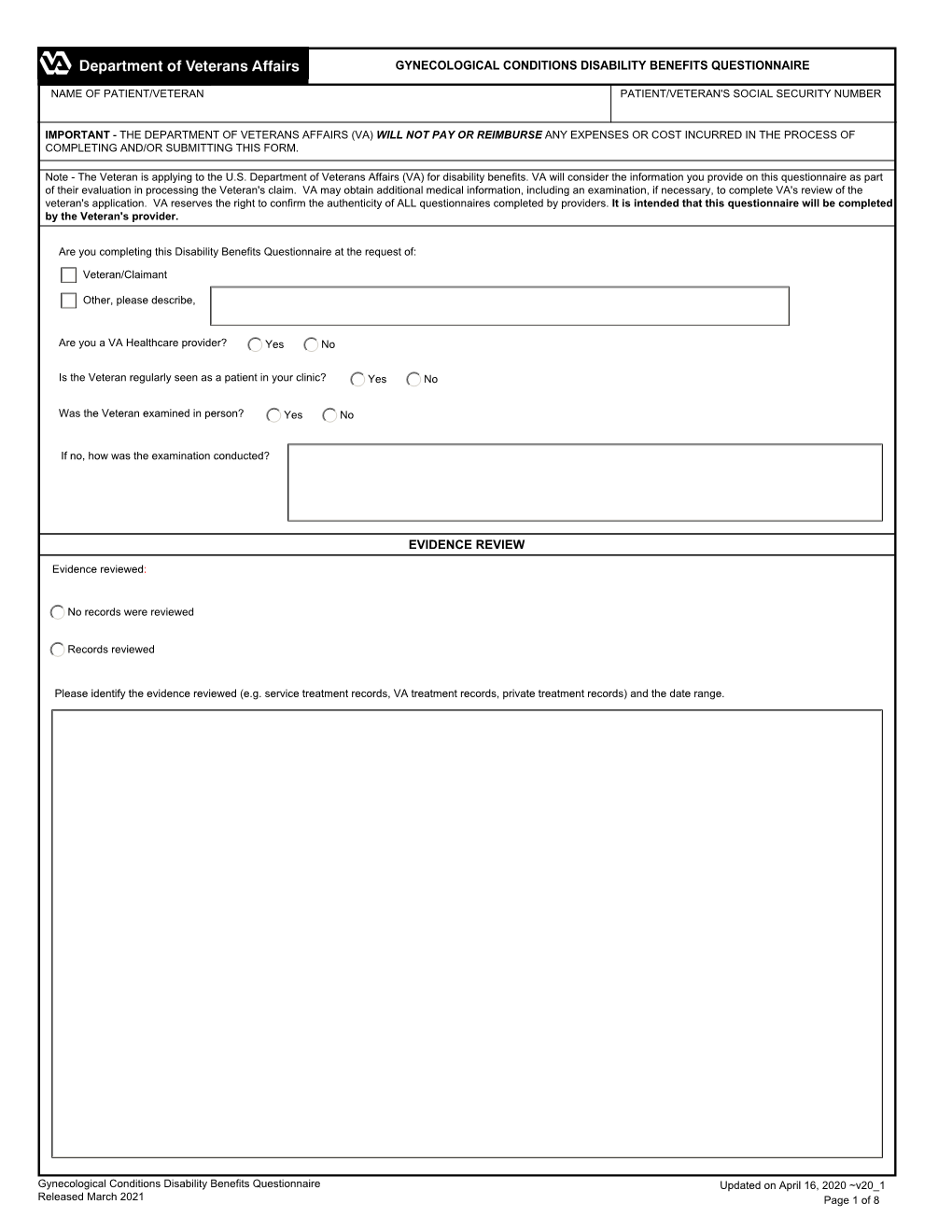
Gynecological Conditions Disability Benefits Questionnaire
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

3-Year Results of Transvaginal Cystocele Repair with Transobturator Four-Arm Mesh: a Prospective Study of 105 Patients
Arab Journal of Urology (2014) 12, 275–284 Arab Journal of Urology (Official Journal of the Arab Association of Urology) www.sciencedirect.com ORIGINAL ARTICLE 3-year results of transvaginal cystocele repair with transobturator four-arm mesh: A prospective study of 105 patients Moez Kdous *, Fethi Zhioua Department of Obstetrics and Gynecology, Aziza Othmana Hospital, Tunis, Tunisia Received 27 January 2014, Received in revised form 1 May 2014, Accepted 24 September 2014 Available online 11 November 2014 KEYWORDS Abstract Objectives: To evaluate the long-term efficacy and safety of transobtura- tor four-arm mesh for treating cystoceles. Genital prolapse; Patients and methods: In this prospective study, 105 patients had a cystocele cor- Cystocele; rected between January 2004 and December 2008. All patients had a symptomatic Transvaginal mesh; cystocele of stage P2 according to the Baden–Walker halfway stratification. We Polypropylene mesh used only the transobturator four-arm mesh kit (SurgimeshÒ, Aspide Medical, France). All surgical procedures were carried out by the same experienced surgeon. ABBREVIATIONS The patients’ characteristics and surgical variables were recorded prospectively. The VAS, visual analogue anatomical outcome, as measured by a physical examination and postoperative scale; stratification of prolapse, and functional outcome, as assessed by a questionnaire TOT, transobturator derived from the French equivalents of the Pelvic Floor Distress Inventory, Pelvic tape; Floor Impact Questionnaire and the Pelvic Organ Prolapse–Urinary Incontinence- TVT, tension-free Sexual Questionnaire, were considered as the primary outcome measures. Peri- vaginal tape; and postoperative complications constituted the secondary outcome measures. TAPF, tendinous arch Results: At 36 months after surgery the anatomical success rate (stage 0 or 1) was of the pelvic fascia; 93%. -

Complications of Incontinence and Prolapse Surgery: Evaluation, Intervention, and Resolution—A Review from Both Specialties W42, 16 October 2012 14:00 - 18:00
Complications of Incontinence and Prolapse Surgery: Evaluation, Intervention, and Resolution—A Review from Both Specialties W42, 16 October 2012 14:00 - 18:00 Start End Topic Speakers 14:00 14:10 Introduction Howard Goldman 14:10 14:35 Complications of incontinence surgery (except Sandip Vasavada retention) 14:35 15:10 Retention/Voiding dysfunction after incontinence Roger Dmochowski surgery 15:10 15:30 Discussion All 15:30 16:00 Break None 16:00 16:35 Complications of prolapse surgery (except Howard Goldman dyspareunia) 16:35 17:00 Dyspareunia after pelvic floor surgery Tristi Muir 17:00 17:40 Discussion All 17:40 18:00 Questions All Aims of course/workshop This course will summarize both common and uncommon complications associated with standard and new technologies used for pelvic floor reconstruction and urinary incontinence therapy in women. The intent of this course is to present both the approach to evaluation and management of these complications from both the urologic and urogynecologic perspective of the combined faculty. The emphasis is on newer technologies and complications, both acute and chronic, which are associated with these various surgeries. The goal of this course will be to summarize, not only identification, but also evaluation and appropriate intervention, as well as patient counselling for these various complications. Educational Objectives This course will provide a detailed paradigm for avoiding, evaluating and managing complications of incontinence and prolapse surgery. Evidence continues to accrue in this area but it runs the spectrum from Level 1 to 5 with much being expert opinion. Unfortunately, very little cross comparison exists to support these differing interventions. -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

Legacy Health
Legacy Health Co-Management and Referral Guidelines Management of Pelvic Floor Dysfunction Phone: 503-413-3707 Legacy Physical Therapy Fax: 503-413-1504 Introduction After appropriate evaluation by your care providers, patients may be referred to pelvic floor physical therapy for management of pelvic floor muscle dysfunctions/pain, incontinence of urine or fecal matter, pelvic floor/girdle physical therapy. • Hypertonic pelvic floor dysfunction — vaginismus, dyspareunia, levator ani syndrome • Hypotonic pelvic floor muscles — organ prolapse, rectus diastasis • Continence issues after abdominal surgeries in male and female (prostate or hysterectomies), overactive bladder • Endometriosis, pelvic pain • Chronic constipation Evaluation Evaluation and A careful history and evaluation/physical exam will be performed to assess the origin and functional Management limitations of the patient. Muscle tone assessment, organ mobility, scar tissue mobility, bladder and/or bowel diary Treatment Strengthening or down-training PF muscles, with or without biofeedback, manual therapy, scar tissue release, electrical stimulation, trigger point release, visceral and myofascial mobilization, body mechanics and core stabilization. Duration One to six 60-minute visits with the physical therapist When to refer Refer when pain is limiting normal activities of daily living, if patient is not able to get to the bathroom dry, if sexual activity is painful (although dyspareunia alone is often not covered by insurance) Commonly referred ICD10 codes and descriptors for PT diagnoses R10.9 Abdominal pain K59.4 Anal spasm/proctalgia fugax R39.89 Bladder pain M53.3 Coccygodynia K59.00 Constipation, unspecified N81.10 Cystocele, unspecified (prolapse of anterior vaginal wall NOS) M62.0 Diastasis rectus post-partum N94.1 Dyspareunia — excludes psychogenic dyspareunia (F52.6). -

Contemporary Issues in Obstetric Fistula
CLINICAL OBSTETRICS AND GYNECOLOGY Volume 00, Number 00, 000–000 Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved. Contemporary Issues in Obstetric Fistula L. LEWIS WALL, MD, DPHIL,*† ITENGRE OUEDRAOGO, MD,‡ and FEKADE AYENACHEW, MD§ *Department of Anthropology, College of Arts and Sciences; †Department of Obstetrics and Gynecology, School of Medicine, Washington University in St. Louis, St. Louis, Missouri; ‡Association Renaissance Arena, Ouagadougou, Burkina Faso; Danja Fistula Center, Danja, Niger; and §International Fistula Alliance, Terrewode Women’s Community Hospital, Soroti, Uganda Abstract: We discuss a variety of contemporary issues connected: for example, a vesicovaginal relating to obstetric fistula. These include definitions of fistula is an abnormal opening between these injuries, the etiologic mechanisms by which fistulas occur, the role of specialist fistula centers in diagnosis the bladder and the vagina. and management, the classification of fistulas, and the Fistulas arise in different ways. A small assessment of surgical outcomes. We also review the number of fistulas are congenital, arising growing need for complex reconstructive surgical pro- from defects that occur during embryog- cedures, follow-up challenges, and the transition to a enesis.1 More commonly, however, fistu- fistula-free world in which other pathologies (such as 2,3 pelvic organ prolapse) will be of increasing importance. las are caused by trauma. Finally, we discuss the need to develop responsive The most common fistulas occurring in systems of maternal health care that treat women with females are genitourinary fistulas (vesico- competence, compassion, respect, and fairness. vaginal fistula, urethrovaginal fistula, Key words: obstetric fistula, vesicovaginal fistula, ’ ureterovaginal fistula, etc.) and genito- obstructed labor, women s rights enteric fistulas (especially rectovaginal fistula). -

Pelvic Floor Ultrasound in Prolapse: What's in It for the Surgeon?
Int Urogynecol J (2011) 22:1221–1232 DOI 10.1007/s00192-011-1459-3 REVIEW ARTICLE Pelvic floor ultrasound in prolapse: what’s in it for the surgeon? Hans Peter Dietz Received: 1 March 2011 /Accepted: 10 May 2011 /Published online: 9 June 2011 # The International Urogynecological Association 2011 Abstract Pelvic reconstructive surgeons have suspected technique became an obvious alternative, whether via the for over a century that childbirth-related trauma plays a transperineal [4, 5] (see Fig. 1) or the vaginal route [6]. major role in the aetiology of female pelvic organ prolapse. More recently, magnetic resonance imaging has also Modern imaging has recently allowed us to define and developed as an option [7], although the difficulty of reliably diagnose some of this trauma. As a result, imaging obtaining functional information, and cost and access is becoming increasingly important, since it allows us to problems, have hampered its general acceptance. identify patients at high risk of recurrence, and to define Clinical examination techniques, in particular if the underlying problems rather than just surface anatomy. examiner is insufficiently aware of their inherent short- Ultrasound is the most appropriate form of imaging in comings, are rather inadequate tools with which to assess urogynecology for reasons of cost, access and performance, pelvic floor function and anatomy. This is true even if one and due to the fact that it provides information in real time. uses the most sophisticated system currently available, the I will outline the main uses of this technology in pelvic prolapse quantification system of the International Conti- reconstructive surgery and focus on areas in which the nence Society (ICS Pelvic Organ Prolapse Quantification benefit to patients and clinicians is most evident. -

The Effects of a Life-Stress Interview for Women with Chronic Urogenital Pain: a Randomized Trial" (2016)
Wayne State University Wayne State University Dissertations 1-1-2016 The ffecE ts Of A Life-Stress Interview For Women With Chronic Urogenital Pain: A Randomized Trial Jennifer Carty Wayne State University, Follow this and additional works at: http://digitalcommons.wayne.edu/oa_dissertations Part of the Clinical Psychology Commons Recommended Citation Carty, Jennifer, "The Effects Of A Life-Stress Interview For Women With Chronic Urogenital Pain: A Randomized Trial" (2016). Wayne State University Dissertations. Paper 1521. This Open Access Dissertation is brought to you for free and open access by DigitalCommons@WayneState. It has been accepted for inclusion in Wayne State University Dissertations by an authorized administrator of DigitalCommons@WayneState. THE EFFECTS OF A LIFE-STRESS INTERVIEW FOR WOMEN WITH CHORNIC UROGENITAL PAIN: A RANDOMIZED TRAIL by JENNIFER N. CARTY DISSERTATION Submitted to the Graduate School of Wayne State University, Detroit, Michigan in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY 2016 MAJOR: PSYCHOLOGY (Clinical) Approved By: ______________________________ Advisor Date ______________________________ ______________________________ ______________________________ ACKNOWLEDGEMENTS I am immensely grateful to many people for their contributions to this project and my professional and personal development. First, I would like to thank my advisor, Dr. Mark Lumley, for his guidance and support in the development of this project, and for both encouraging and challenging me throughout my academic career, for which I will always be grateful. I would also like to thank Dr. Janice Tomakowsky, Dr. Kenneth Peters, and the medical providers, physical therapists, and staff at the Women’s Urology Center at Beaumont Hospital for graciously allowing me to conduct this study at their clinic and with their patients. -

Grading Pelvic Prolapse and Pelvic Floor Relaxation Using Dynamic Magnetic Resonance Imaging
ADULT UROLOGY GRADING PELVIC PROLAPSE AND PELVIC FLOOR RELAXATION USING DYNAMIC MAGNETIC RESONANCE IMAGING CRAIG V. COMITER, SANDIP P. VASAVADA, ZORAN L. BARBARIC, ANGELO E. GOUSSE, AND SHLOMO RAZ ABSTRACT Objectives. With significant vaginal prolapse, it is often difficult to differentiate among cystocele, enterocele, and high rectocele by physical examination alone. Our group has previously demonstrated the utility of magnetic resonance imaging (MRI) for evaluating pelvic prolapse. We describe a simple objective grading system for quantifying pelvic floor relaxation and prolapse. Methods. One hundred sixty-four consecutive women presenting with pelvic pain (n ϭ 39) or organ prolapse (n ϭ 125) underwent dynamic MRI. The “H-line” (levator hiatus) measures the distance from the pubis to the posterior anal canal. The “M-line” (muscular pelvic floor relaxation) measures the descent of the levator plate from the pubococcygeal line. The “O” classification (organ prolapse) characterizes the degree of visceral prolapse beyond the H-line. Results. The image acquisition time was 2.5 minutes per study. Each study cost $540. In the pain group, the H-line averaged 5.2 Ϯ 1.1 cm versus 7.5 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). The M-line averaged 1.9 Ϯ 1.2 cm in the pain group versus 4.1 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). Incidental pelvic pathologic features were commonly noted, including uterine fibroids, ovarian cysts, hydroureter, urethral diverticula, and foreign body. Conclusions. The HMO classification provides a straightforward and reproducible method for staging and quantifying pelvic floor relaxation and visceral prolapse. -

Uro 2018-159 Issue Date: 02/2015 Review Date: 03/2021 © Liverpool Women’S NHS Foundation Trust
Vaginal Pessary Information Leaflet What Is A Pessary? A pessary is a plastic or silicone device that fits into your vagina to support a prolapsed bladder, rectum or uterus (womb). There are different types but the most commonly used are either a ring or a shelf pessary. 71%- 90% of women are successfully fitted with a pessary. What Is A Prolapse? A prolapse means that your uterus, bladder or rectum is bulging or leaning into the vagina, because the muscular walls of the vagina have become weakened. This can sometimes be felt as a lump in the vagina. If the prolapse is large it may also cause difficulty when emptying the bladder or bowel. It is possible for women to have more than one type of prolapse. 50% of women can get a prolapse. Patients can have varying symptoms such as vaginal heaviness, pelvic pressure bulging into the vagina and backache. What Are The Different Types Of Prolapse? Cystocele A cystocele occurs when the vaginal wall that is next to the bladder becomes weakened. This causes the bladder to lean (or prolapse) into the vagina, where it may then be felt as a lump (See Figure 1) Cystocele Figure 1 Rectocele A rectocele occurs when the vaginal wall next to the rectum becomes weakened. This causes the rectum to lean (or prolapse) into the vagina, where it may then be felt as a lump. This type of prolapse may cause difficulty when opening your bowels. (See Figure 2) Figure 2 Uterine prolapse A Uterine prolapse occurs when the structures that support the womb weaken. -

Differential Diagnosis of Endometriosis by Ultrasound
diagnostics Review Differential Diagnosis of Endometriosis by Ultrasound: A Rising Challenge Marco Scioscia 1 , Bruna A. Virgilio 1, Antonio Simone Laganà 2,* , Tommaso Bernardini 1, Nicola Fattizzi 1, Manuela Neri 3,4 and Stefano Guerriero 3,4 1 Department of Obstetrics and Gynecology, Policlinico Hospital, 35031 Abano Terme, PD, Italy; [email protected] (M.S.); [email protected] (B.A.V.); [email protected] (T.B.); [email protected] (N.F.) 2 Department of Obstetrics and Gynecology, “Filippo Del Ponte” Hospital, University of Insubria, 21100 Varese, VA, Italy 3 Obstetrics and Gynecology, University of Cagliari, 09124 Cagliari, CA, Italy; [email protected] (M.N.); [email protected] (S.G.) 4 Department of Obstetrics and Gynecology, Azienda Ospedaliero Universitaria, Policlinico Universitario Duilio Casula, 09045 Monserrato, CA, Italy * Correspondence: [email protected] Received: 6 October 2020; Accepted: 15 October 2020; Published: 20 October 2020 Abstract: Ultrasound is an effective tool to detect and characterize endometriosis lesions. Variances in endometriosis lesions’ appearance and distorted anatomy secondary to adhesions and fibrosis present as major difficulties during the complete sonographic evaluation of pelvic endometriosis. Currently, differential diagnosis of endometriosis to distinguish it from other diseases represents the hardest challenge and affects subsequent treatment. Several gynecological and non-gynecological conditions can mimic deep-infiltrating endometriosis. For example, abdominopelvic endometriosis may present as atypical lesions by ultrasound. Here, we present an overview of benign and malignant diseases that may resemble endometriosis of the internal genitalia, bowels, bladder, ureter, peritoneum, retroperitoneum, as well as less common locations. An accurate diagnosis of endometriosis has significant clinical impact and is important for appropriate treatment. -

Male Infertility
Guidelines on Male Infertility A. Jungwirth, T. Diemer, G.R. Dohle, A. Giwercman, Z. Kopa, C. Krausz, H. Tournaye © European Association of Urology 2012 TABLE OF CONTENTS PAGE 1. METHODOLOGY 6 1.1 Introduction 6 1.2 Data identification 6 1.3 Level of evidence and grade of recommendation 6 1.4 Publication history 7 1.5 Definition 7 1.6 Epidemiology and aetiology 7 1.7 Prognostic factors 8 1.8 Recommendations on epidemiology and aetiology 8 1.9 References 8 2. INVESTIGATIONS 9 2.1 Semen analysis 9 2.1.1 Frequency of semen analysis 9 2.2 Recommendations for investigations in male infertility 10 2.3 References 10 3. TESTICULAR DEFICIENCY (SPERMATOGENIC FAILURE) 10 3.1 Definition 10 3.2 Aetiology 10 3.3 Medical history and physical examination 11 3.4 Investigations 11 3.4.1 Semen analysis 11 3.4.2 Hormonal determinations 11 3.4.3 Testicular biopsy 11 3.5 Conclusions and recommendations for testicular deficiency 12 3.6 References 12 4. GENETIC DISORDERS IN INFERTILITY 14 4.1 Introduction 14 4.2 Chromosomal abnormalities 14 4.2.1 Sperm chromosomal abnormalities 14 4.2.2 Sex chromosome abnormalities 14 4.2.3 Autosomal abnormalities 15 4.3 Genetic defects 15 4.3.1 X-linked genetic disorders and male fertility 15 4.3.2 Kallmann syndrome 15 4.3.3 Mild androgen insensitivity syndrome 15 4.3.4 Other X-disorders 15 4.4 Y chromosome and male infertility 15 4.4.1 Introduction 15 4.4.2 Clinical implications of Y microdeletions 16 4.4.2.1 Testing for Y microdeletions 17 4.4.2.2 Y chromosome: ‘gr/gr’ deletion 17 4.4.2.3 Conclusions 17 4.4.3 Autosomal defects with severe phenotypic abnormalities and infertility 17 4.5 Cystic fibrosis mutations and male infertility 18 4.6 Unilateral or bilateral absence/abnormality of the vas and renal anomalies 18 4.7 Unknown genetic disorders 19 4.8 DNA fragmentation in spermatozoa 19 4.9 Genetic counselling and ICSI 19 4.10 Conclusions and recommendations for genetic disorders in male infertility 19 4.11 References 20 5.