Immunotherapy for Targeting Cancer Stem Cells in Hepatocellular Carcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Maria Khayutina • [email protected] the Tombs
Maria Khayutina [email protected] The Tombs of Peng State and Related Questions Paper for the Chicago Bronze Workshop, November 3-7, 2010 (, 1.1.) () The discovery of the Western Zhou period’s Peng State in Heng River Valley in the south of Shanxi Province represents one of the most fascinating archaeological events of the last decade. Ruled by a lineage of Kui (Gui ) surname, Peng, supposedly, was founded by descendants of a group that, to a certain degree, retained autonomy from the Huaxia cultural and political community, dominated by lineages of Zi , Ji and Jiang surnames. Considering Peng’s location right to the south of one of the major Ji states, Jin , and quite close to the eastern residence of Zhou kings, Chengzhou , its case can be very instructive with regard to the construction of the geo-political and cultural space in Early China during the Western Zhou period. Although the publication of the full excavations’ report may take years, some preliminary observations can be made already now based on simplified archaeological reports about the tombs of Peng ruler Cheng and his spouse née Ji of Bi . In the present paper, I briefly introduce the tombs inventory and the inscriptions on the bronzes, and then proceed to discuss the following questions: - How the tombs M1 and M2 at Hengbei can be dated? - What does the equipment of the Hengbei tombs suggest about the cultural roots of Peng? - What can be observed about Peng’s relations to the Gui people and to other Kui/Gui- surnamed lineages? 1. General Information The cemetery of Peng state has been discovered near Hengbei village (Hengshui town, Jiang County, Shanxi ). -

The 16Th International Conference on Service Systems and Service Management
The 16th International Conference on Service Systems and Service Management Co-Sponsored by: IEEE SMC The Chinese University of Hong Kong, Shenzhen Tsinghua University University of Electronic Science and Technology of China July 13-15, 2019 The Chinese University of Hong Kong, Shenzhen (CUHKSZ) Welcome Message from the Conference Co-Chairs Welcome to Shenzhen; Welcome to ICSSSM2019! ICSSSM is a conference series, organized annually, focusing on state-of-the- art research in service systems and service management. The 16th ICSSSM is jointly sponsored by IEEE Systems, Man and Cybernetics Society, The Chinese University of Hong Kong (Shenzhen), Tsinghua University, and University of Electronic Science and Technology of China. It is hosted by The Chinese University of Hong Kong (Shenzhen). The main purpose of ICSSSM is to provide a platform for researchers, scholars, practitioners and students involved in the broad area of service systems and service management to disseminate their latest research results, as well as to exchange views on the future research directions. This year, 259 technical papers have been accepted, after a rigorous review process, for presentation at the Conference and publication in the conference proceedings. ICSSSM2019 has scheduled to organize a wide range of activities. Four Keynote Speeches will be given by distinguished speakers. Moreover, thirty-eight Technical Sessions will be organized. The topics of the technical sessions include Electronic Business New Models and Strategies; Specific Industrial Service Management; Supply Chain Management for Service; Service System Design, Operations, and Management; Theory and Principle of Service Sciences; Service Information Technology and Decision Making; Data Analytics and Service Management; Service Empirical Studies and Case Studies; Service Marketing and Financial Management; and Management of Healthcare Services. -

China to Keep Watch on TPP
Table for strangers Hainan helps visitors Memory protection Special police target tourism An app connects amateur chefs industry irregularities in Sanya with willing dining companions Database to be created on > CHINA, PAGE 4 > LIFE, PAGE 9 the Nanjing Massacre > p3 MONDAY, October 12, 2015 chinadailyusa.com $1 COMMERCE China to keep watch on TPP Such trade deals can disrupt non-signatories: offi cial By ZHONG NAN highly unlikely that the TPP would in Beijing lead to the creation of a trade bloc [email protected] that excludes China. “The economic development China will conduct comprehensive mode in China has already changed and systematic assessments of the from low-end product trade to ‘going fallout from the Trans-Pacifi c Part- global’ strategies like setting up or nership, a broad agreement between moving manufacturing facilities and 12 Pacifi c Rim countries, including to more direct investment in over- Japan and the United States, since it seas markets,” said Fan. believes that such deals have disrup- Besides the US, other signatories tive eff ects on non-signatory nations, to the TPP are Australia, Brunei, a top government offi cial said. Canada, Chile, Japan, Malaysia, Mex- Commerce Minister Gao Hucheng ico, New Zealand, Peru, Singapore said China is of the view that changes and Vietnam. in the global trade pattern should be China has to date signed bilateral decided by adjustments in the indus- and multilateral free trade agree- trial structure and through product ments with seven TPP members. competitiveness in global -

Download File
On the Periphery of a Great “Empire”: Secondary Formation of States and Their Material Basis in the Shandong Peninsula during the Late Bronze Age, ca. 1000-500 B.C.E Minna Wu Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMIBIA UNIVERSITY 2013 @2013 Minna Wu All rights reserved ABSTRACT On the Periphery of a Great “Empire”: Secondary Formation of States and Their Material Basis in the Shandong Peninsula during the Late Bronze-Age, ca. 1000-500 B.C.E. Minna Wu The Shandong region has been of considerable interest to the study of ancient China due to its location in the eastern periphery of the central culture. For the Western Zhou state, Shandong was the “Far East” and it was a vast region of diverse landscape and complex cultural traditions during the Late Bronze-Age (1000-500 BCE). In this research, the developmental trajectories of three different types of secondary states are examined. The first type is the regional states established by the Zhou court; the second type is the indigenous Non-Zhou states with Dong Yi origins; the third type is the states that may have been formerly Shang polities and accepted Zhou rule after the Zhou conquest of Shang. On the one hand, this dissertation examines the dynamic social and cultural process in the eastern periphery in relation to the expansion and colonization of the Western Zhou state; on the other hand, it emphasizes the agency of the periphery during the formation of secondary states by examining how the polities in the periphery responded to the advances of the Western Zhou state and how local traditions impacted the composition of the local material assemblage which lay the foundation for the future prosperity of the regional culture. -
Langdon Warner at Dunhuang: What Really Happened? by Justin M
ISSN 2152-7237 (print) ISSN 2153-2060 (online) The Silk Road Volume 11 2013 Contents In Memoriam ........................................................................................................................................................... [iii] Langdon Warner at Dunhuang: What Really Happened? by Justin M. Jacobs ............................................................................................................................ 1 Metallurgy and Technology of the Hunnic Gold Hoard from Nagyszéksós, by Alessandra Giumlia-Mair ......................................................................................................... 12 New Discoveries of Rock Art in Afghanistan’s Wakhan Corridor and Pamir: A Preliminary Study, by John Mock .................................................................................................................................. 36 On the Interpretation of Certain Images on Deer Stones, by Sergei S. Miniaev ....................................................................................................................... 54 Tamgas, a Code of the Steppes. Identity Marks and Writing among the Ancient Iranians, by Niccolò Manassero .................................................................................................................... 60 Some Observations on Depictions of Early Turkic Costume, by Sergey A. Yatsenko .................................................................................................................... 70 The Relations between China and India -

Icmfloc 2018
The Second International Conference of Microfluidics, Nanofluidics, and Lab-on-a-Chip Beijing, China June 8 - 10, 2018 http://www.icmfloc2018.org ICMFLOC 2018 Program Organized by Beijing International Center for Theoretical and Applied Mechanics Institute of Mechanics, Chinese Academy of Sciences Beijing University of Technology Supported by National Natural Science Foundation of China The State Key Laboratory of Nonlinear Mechanics | Sponsors www.amaxchina.com www.mesobiosys.com www.bmftec.cn www.beijingec.com www.stella-litho.com www.worldoflab.com www.fhsci.com.cn www.dolomite-microfluidics.com www.dantecdynamics.com www.hicomp.com www.highraychip.com www.rdmicro.com www.idex-hs.com | Media Partners www.mdpi.com/journal/micromachines www.mdpi.com/journal/sensors Table of Content Welcome……………………………………………………………………1 Conference Organization……………………………………………2 Conference at a Glance………………………………………………4 Special Events…………………………………………………………….5 Conference Rooms Plan………..……………………………………6 Program Overview……………………………..………………………7 Parallel Sessions……………………………………………..………….8 Poster Sessions………………………………………………..…….…16 Author Index………………………………………………………....…19 Call for the papers in Special Issues Special Issue of ICMFLOC2018 in Microfluidics and Nanofluidics http://www.editorialmanager.com/mano/default.aspx Guest editors: Guoqing Hu, Zhaomiao Liu, Ting Si Special Issue of ICMFLOC2018 in Electrophoresis http://mc.manuscriptcentral.com/elpho Guest editors: Xiangchun Xuan, Yuejun Kang, Jiashu Sun Welcome We warmly welcome all distinguished guests to the Second International Conference of Microfluidics, Nanofluidics and Lab-on-a-Chip (ICMFLOC) held in Beijing in June 8-10, 2018. This conference was organized by the Beijing International Center for Theoretical and Applied Mechanics, the Institute of Mechanics of the Chinese Academy of Sciences, and the Beijing University of Technology. Research on microfluidics, nanofluidics and lab-on-a-chip has advanced rapidly over the past two decades. -

2017 36Th Chinese Control Conference (CCC 2017)
2017 36th Chinese Control Conference (CCC 2017) Dalian, China 26-28 July 2017 Pages 1-776 IEEE Catalog Number: CFP1740A-POD ISBN: 978-1-5386-2918-5 1/15 Copyright © 2017, Technical Committee on Control Theory, Chinese Association of Automation All Rights Reserved *** This is a print representation of what appears in the IEEE Digital Library. Some format issues inherent in the e-media version may also appear in this print version. IEEE Catalog Number: CFP1740A-POD ISBN (Print-On-Demand): 978-1-5386-2918-5 ISBN (Online): 978-9-8815-6393-4 ISSN: 1934-1768 Additional Copies of This Publication Are Available From: Curran Associates, Inc 57 Morehouse Lane Red Hook, NY 12571 USA Phone: (845) 758-0400 Fax: (845) 758-2633 E-mail: [email protected] Web: www.proceedings.com Proceedings of the 36th Chinese Control Conference, July 26-28, 2017, Dalian, China Contents Systems Theory and Control Theory Robust H∞filter design for continuous-time nonhomogeneous markov jump systems . BIAN Cunkang, HUA Mingang, ZHENG Dandan 28 Continuity of the Polytope Generated by a Set of Matrices . MENG Lingxin, LIN Cong, CAI Xiushan 34 The Unmanned Surface Vehicle Course Tracking Control with Input Saturation . BAI Yiming, ZHAO Yongsheng, FAN Yunsheng 40 Necessary and Sufficient D-stability Condition of Fractional-order Linear Systems . SHAO Ke-yong, ZHOU Lipeng, QIAN Kun, YU Yeqiang, CHEN Feng, ZHENG Shuang 44 A NNDP-TBD Algorithm for Passive Coherent Location . ZHANG Peinan, ZHENG Jian, PAN Jinxing, FENG Songtao, GUO Yunfei 49 A Superimposed Intensity Multi-sensor GM-PHD Filter for Passive Multi-target Tracking . -

Welcome to the Water Margin Podcast. This Is Episode 10. Last Time
Welcome to the Water Margin Podcast. This is episode 10. Last time, Lu Zhishen managed to get himself kicked out of the monastery on Wutai Mountain, but the abbot still looked out for him and sent him to a colleague at another monastery located in the capital. On his way, Lu Zhishen came across a manor where an old man was being forced to marry his daughter to a bandit chieftain. Lu Zhishen told the old man he could persuade the bandit to change his mind and give up the marriage, so the old man allowed him to wait for the bandit in the bridal chamber. And of course, by “persuade,” Lu Zhishen meant “I’ll make the guy think he’s coming to meet his wife in the dark and then beat him to a bloody pulp, and I’ll do it totally naked, just for more laughs.” But when all was said and done, no one else was laughing. Not the bandit chieftain, who ran back to his mountain hideout bruised and bloodied, and especially not the old man, Grandpa Liu (2), who was dreading the death and destruction that will no doubt rain down his house when said bandit chieftain returns with a vengeance. After Lu Zhishen spared everyone further trauma by putting his clothes back on, Grandpa Liu said to him, “I thought you were going to talk to the bandit and convince him to change his mind. I didn’t know you were going to give him a beating. Now he must have gone off to round up the rest of his men to come slaughter me and my family.” “Sir, don’t worry,” Zhishen said. -

Read Book # Articles on Water Margin Characters, Including: Emperor
ZKGCK4RENJHS » eBook » Articles On Water Margin Characters, including: Emperor Huizong Of Song, Du Wei... Download Kindle ARTICLES ON WATER MARGIN CHARACTERS, INCLUDING: EMPEROR HUIZONG OF SONG, DU WEI (WATER MARGIN), FANG JIE, TIAN HU, WANG QING, SHI BAO (WATER MARGIN), PANG WANCHUN, FANG TIANDING, ZHOU TONG (ARCHER), L Read PDF Articles On Water Margin Characters, including: Emperor Huizong Of Song, Du Wei (water Margin), Fang Jie, Tian Hu, Wang Qing, Shi Bao (water Margin), Pang Wanchun, Fang Tianding, Zhou Tong (archer), L Authored by Books, Hephaestus Released at 2016 Filesize: 4.77 MB To read the e-book, you will want Adobe Reader software program. You can download the installer and instructions free from the Adobe Web site if you do not have Adobe Reader already installed on your computer. You could possibly download and keep it on your laptop for afterwards read. Be sure to follow the hyperlink above to download the PDF file. Reviews Comprehensive guide for pdf fanatics. It is lled with knowledge and wisdom It is extremely difcult to leave it before concluding, once you begin to read the book. -- Valentin Thompson The ideal pdf i at any time go through. It is really basic but unexpected situations from the fty percent of your pdf. Its been designed in an extremely easy way and is particularly only after i finished reading this pdf through which really changed me, alter the way i really believe. -- Prof. Kendrick Stracke Thorough manual for pdf lovers. I am quite late in start reading this one, but better then never. It is extremely difcult to leave it before concluding, once you begin to read the book. -

CONFERENCE PROGRAM Second International Conference on Communications and Networking in China (CHINACOM 2007)
CONFERENCE PROGRAM Second International Conference on Communications and Networking in China (CHINACOM 2007) http://www.chinacom.org Co-Sponsored by Technical Sponsors GREETINGS FROM THE GENERAL CHAIRS On behalf of the organizing committee, we would like to welcome you to the 2nd International Conference on Communications and Networking in China (CHINACOM 2007), to be held in Shanghai on August 22-24, 2007. CHINACOM 2007 is being positioned as a premier international annual conference for the presentation of original contributions and fundamental advances in the field of Communications, Networks, and Internet Applications. It will showcase a strong technical program consisting of 6 Symposia, special sessions. CHINACOM 2007 will also feature two prominent invited keynote speakers: Dr. David G. Belanger, AT&T Labs Research V.P. and Chief Scientist of Information & Software Systems, and Dr. Paulo T. de Sousa, Head of Sector, Internet of the Future, in the Directorate-General Information Society, European Commission. We are very grateful to the sponsorship of Create-Net, ICST, and Shanghai Jiao Tong University, and technical support of IEEE, IEEE CAS, IEEE MTT-S, IEEE CVTC, Beijing University of Posts and Telecommunications, and Zhejiang University. We would like to express our sincere thanks and appreciation to all the organizing committee members, the technical program chairs, symposium chairs, the technical program committee members and reviewers. We would also like to thanks all the authors for submitting their papers to the conference. All accepted and presented papers will be included in the CHINACOM 2007 Conference Proceedings. They will be made available in IEEE Xplore Digital Library and be indexed by Engineering Information (EI). -
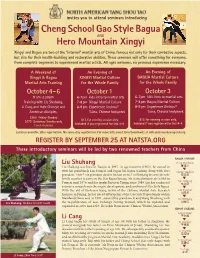
OCT XINGYI and BAGUA Event
invites you to attend seminars introducing Cheng School Gao Style Bagua AND Hero Mountain Xingyi Xingyi and Bagua are two of the “internal” martial arts of China, famous not only for their combative aspects, but also for their health-building and restorative abilities. These seminars will offer something for everyone, from complete beginners to experienced martial artists. All ages welcome, no previous experience neces sary. A Weekend of An Evening of An Evening of Xingyi Bagua XINGYI Martial Culture BAGUA Martial Culture Martial Ar&ts Training for the Whole Family for the Whole Family October 4- 6 October 1 October 3 9 am-3:30 pm 6-7 pm kids intro to martial arts 6-7 pm kids intro to martial arts Training with Liu Shuhang, 7-8 pm Xingyi Martial Culture 7-8 pm Bagua Martial Culture Li Cang and their Chinese and 8- 9 pm Experience Jinshou© 8- 9pm Experience Jinshou© American disciples. Tuina, Chinese bodywork Tuina, Chinese bodywork $200 Friday-Sunday $15 for evening session only. $175 Saturday-Sunday only $15 for evening session only. Included if you registered for Oct 4-6 Lunch included Included if you registered for Oct 4-6 Location available after registration. No same-day registration. For more info email John Groschwitz at [email protected] REGISTER BY SEPTEMBE R 25 AT NATSTA.ORG These introductory seminars will be led by two renowned teachers from China BAGUA LINEAGE: Liu Shuhang Dong Haichuan Liu Shuhang was born in Tianjin in 1947. At age fourteen (1962), he moved in 董海川 with his granduncle Liu Fengcai and began his Bagua training along with Liu’s Cheng Tinghua grandson. -

The Disappearance of Silk Weaves with Weft Effects in Early China
Chinese Science 12 (1995): 41-76 The Disappearance of Silk Weaves with Weft Effects in Early China Angela Sheng [Angela Sheng was formerly Assistant Curator in the Textiles Department, Royal Ontario Museum, Toronto, Canada. She is now living and researching in Japan. Material in Figures 5, Al, A2, and A4 has been reprinted from Dorothy K. Burnham, Warp and Weft: A Textile Tenninology (Toronto: Royal Ontario Museum, 1980), with permission ofthe author.} * * * n 1982 spectacular costumes and textiles were unearthed from the Number I One Chu Tomb (340-278 B.C.) at Mashan in Jiangling (Hubei 1985). Complex patterns woven with weft effect were found on seven silk bands (taodai) trimming the opening of four robes. 1 This discovery all but shatters the misconception that the ancient Chinese learned to weave patterns in the weft from foreigners and obliterates the false debate about the origin of the Chinese drawloom. 2 But it also raises a new question: why did the Chinese not continue 1 The term "weaves with weft effects" follows Dorothy Bumham's classification ( 1980: 195-96). Textile terms are often confusing in both English and Chinese and this confusion is compounded in translation. As much as possible, I will use modem Chinese textile terms that refer to weave structures and provide their English equivalents. Where two different ancient textiles are the same in structure, I will use their historical names. For details on Chinese silk weaves, see Becker 1987: 23-25 and Zhao Feng 1992: 31-73. For an explantion of textile terins, see Appendix. 2 Based on textile finds from Antinoi!, Egypt dating to A.O.