The Francis Crick Institute Studies on Low Ph-Activated HA2 From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wellcome Trust Annual Report and Financial Statements 2017 Contents
Annual Report and Financial Statements 2017 2 Wellcome Trust Annual Report and Financial Statements 2017 Contents Report from the Chair and the Director 5 Trustee’s Report 8 What we do 8 Review of Charitable Activities 9 Review of Investment Activities 18 Financial Review 29 Structure and Governance 34 Risk Management 37 Remuneration Report 40 Audit Committee Report 43 Independent Auditor’s Report 45 Financial Statements 58 Consolidated Statement of Financial Activities 58 Consolidated Balance Sheet 59 Statement of Financial Activities of the Trust 60 Balance Sheet of the Trust 61 Consolidated Cash Flow Statement 62 Notes to the Financial Statements 63 Reference and Administrative Details 117 3 Wellcome Trust Annual Report and Financial Statements 2017 “ At Wellcome, we believe in the power of ideas to improve health” Jeremy Farrar Director 4 Wellcome Trust Annual Report and Financial Statements 2017 Report from the Chair and the Director “Our core approach is funding people to explore great ideas, at every step of the way from discovery to impact” At Wellcome, we believe in the power of ideas to improve cause of maternal mortality in the world. It also includes health. Funded from our independent investment portfolio, supporting research in the humanities and social sciences, we support thousands of scientists and researchers in more such as a project which this year published ethical guidelines than 70 countries, as well as innovators, educators and artists. for involving pregnant women in Zika vaccine research. Together, we take on big problems, fuel imaginations and spark And resources like the Human Induced Pluripotent Stem Cell debate, working always to achieve better health for everyone. -
The Electron Microscopy Science Technology Platform at the Francis
The Francis Crick Institute is a The Electron biomedical discovery institute Microscopy dedicated to understanding the fundamental biology underlying Science health and disease. Its work Technology is helping to understand why disease develops and to translate Platform at discoveries into new ways to the Francis prevent, diagnose and treat illnesses such as cancer, heart Crick Institute disease, stroke, infections, and Lucy Collinson neurodegenerative diseases. An independent organisation, its founding partners are the Medical Research Council (MRC), Cancer Research UK, Wellcome, University College London, Imperial College London and King’s College London. The Crick was formed in 2015, with many of the Crick’s scientists joining from two ‘parent’ institutes, the MRC’s National Institute for Medical Research and Cancer Research UK’s London Research Institute, and in 2016 it moved into a brand new state-of- the-art building in central London which brings together 1500 scientists and support staff working collaboratively across disciplines, making it the biggest biomedical research facility under a single roof in Europe. © Nick Guttridge 4 ISSUE 46 JUNE 2017 5 Each microscope room is a six-sided shielded box, • The Phenom-World DelPhi benchtop SEM with walls that contain complex metallic layers has an integrated fluorescence microscope to attenuate DC fields, and an active cancellation for correlative imaging system to attenuate AC fields. Under each • The FEI Twin 120 kV TEM has a cryo stage for microscope is a concrete platform, cast in place, and screening vitrified macromolecular samples supported by air springs that remove environmental prior to imaging on 200 kV and 300 kV TEMs vibration to <1 Hz. -

Structure of Human Aspartyl Aminopeptidase Complexed With
Chaikuad et al. BMC Structural Biology 2012, 12:14 http://www.biomedcentral.com/1472-6807/12/14 RESEARCH ARTICLE Open Access Structure of human aspartyl aminopeptidase complexed with substrate analogue: insight into catalytic mechanism, substrate specificity and M18 peptidase family Apirat Chaikuad1, Ewa S Pilka1, Antonio De Riso2, Frank von Delft1, Kathryn L Kavanagh1, Catherine Vénien-Bryan2, Udo Oppermann1,3 and Wyatt W Yue1* Abstract Backround: Aspartyl aminopeptidase (DNPEP), with specificity towards an acidic amino acid at the N-terminus, is the only mammalian member among the poorly understood M18 peptidases. DNPEP has implicated roles in protein and peptide metabolism, as well as the renin-angiotensin system in blood pressure regulation. Despite previous enzyme and substrate characterization, structural details of DNPEP regarding ligand recognition and catalytic mechanism remain to be delineated. Results: The crystal structure of human DNPEP complexed with zinc and a substrate analogue aspartate-β- hydroxamate reveals a dodecameric machinery built by domain-swapped dimers, in agreement with electron microscopy data. A structural comparison with bacterial homologues identifies unifying catalytic features among the poorly understood M18 enzymes. The bound ligands in the active site also reveal the coordination mode of the binuclear zinc centre and a substrate specificity pocket for acidic amino acids. Conclusions: The DNPEP structure provides a molecular framework to understand its catalysis that is mediated by active site loop swapping, a mechanism likely adopted in other M18 and M42 metallopeptidases that form dodecameric complexes as a self-compartmentalization strategy. Small differences in the substrate binding pocket such as shape and positive charges, the latter conferred by a basic lysine residue, further provide the key to distinguishing substrate preference. -

A Critical Base Pair in K-Turns That Confers Folding Characteristics and Correlates with Biological Function
ARTICLE Received 16 Apr 2014 | Accepted 2 Sep 2014 | Published 29 Oct 2014 DOI: 10.1038/ncomms6127 OPEN A critical base pair in k-turns that confers folding characteristics and correlates with biological function Scott A. McPhee1, Lin Huang1 & David M.J. Lilley1 Kink turns (k-turns) are widespread elements in RNA that mediate tertiary contacts by kinking the helical axis. We have found that the ability of k-turns to undergo ion-induced folding is conferred by a single base pair that follows the conserved AG pairs, that is, the 3b3n position. A Watson–Crick pair leads to an inability to fold in metal ions alone, while 3n ¼ Gor3b¼ C (but not both) permits folding. Crystallographic study reveals two hydrated metal ions coordinated to O6 of G3n and G2n of Kt-7. Removal of either atom impairs Mg2 þ - induced folding in solution. While SAM-I riboswitches have 3b3n sequences that would predispose them to ion-induced folding, U4 snRNA are strongly biased to an inability to such folding. Thus riboswitch sequences allow folding to occur independently of protein binding, while U4 should remain unfolded until bound by protein. The empirical rules deduced for k-turn folding have strong predictive value. 1 Cancer Research UK Nucleic Acid Structure Research Group, MSI/WTB Complex, The University of Dundee, Dow Street, Dundee DD1 5EH, UK. Correspondence and requests for materials should be addressed to D.M.J.L. (email: [email protected]). NATURE COMMUNICATIONS | 5:5127 | DOI: 10.1038/ncomms6127 | www.nature.com/naturecommunications 1 & 2014 Macmillan Publishers Limited. -
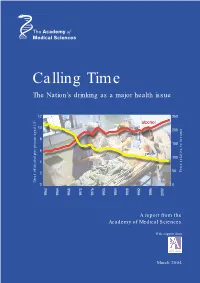
Calling Time the Nation’S Drinking As a Major Health Issue
Calling Time The Nation’s drinking as a major health issue 12 250 10 200 8 150 6 100 4 50 to income Price relative 2 Litres of alcohol per person aged 15+Litres 0 0 1960 1964 1968 1970 1976 1980 1984 1988 1992 1996 2000 A report from the Academy of Medical Sciences With support from March 2004 The independent Academy of Medical Sciences promotes advances in medical science and public health and campaigns to ensure these are translated as quickly as possible into benefits for society. The Academy’s 750 Fellows are the United Kingdom’s leading medical scientists from hospitals, academia, industry and the public service. The aims of the Academy are to: • give national and international leadership in the medical sciences; • promote the application of research to the practice of medicine and to the advancement of human health and welfare; • promote the aims and ethos of medical sciences with particular emphasis on excellence in research and training; • enhance public understanding of the medical sciences and their impact on society; • assess and advise on issues of medical science of public concern. The Academy of Medical Sciences was established in 1998 following the recommendations of a working group chaired by Sir Michael Atiyah, Past President of the Royal Society. There is an elected Council of 22 Fellows that includes the five Officers of the Academy: President Sir Keith Peters, FRS, PMedSci Vice-President (Clinical) Lord Turnberg, FMedSci Vice-President (Non-clinical) Sir John Skehel, FRS, FMedSci Treasurer Sir Colin Dollery, FMedSci Registrar Professor Patrick Vallance, FMedSci The Academy is a registered charity and a company limited by guarantee. -

Living Healthier for Longer Sharing Data Saves Lives
News from the Medical Research Council network Spring 2014 Leading science for better health MEASUREto How some MRC scientific workshops are making custom-made kit to enable pioneering research Living healthier for longer Supporting innovative ageing research through the Lifelong Health and Wellbeing initiative Sharing data saves lives Opinions from two MRC researchers Network can also be downloaded as a PDF at: www.mrc.ac.uk/network CONTENTS NEWS News COMMENT FROM £39.1m for improving data research 3 £39.1m for improving Science festival fun 4 John Let’s talk about dementia 7 data research Savill A £32m MRC investment, announced by Universities and Science the MRC Consortium for Medical Microbial Bioinformatics led by Minister David Willetts at the High Performance Computing and Warwick University, the Medical Bioinformatics partnership led People CHIEF EXECUTIVE Big Data Conference in London on 6 February, plus an additional by Imperial College London and University College London £7.1m, is the latest instalment of a £90m funding initiative to Partners which includes the Francis Crick Institute, will also Dr Jane Cope on the power of persuasion 9 In February, the Minister for tackle health and bioinformatics challenges for the advancement support career opportunities for computational scientists, Universities and Science David of medical research. technologists and programme leaders, enhancing the UK’s skills Willetts announced a £32m MRC in this area. investment into improving the UK’s Six major strategic awards will strengthen collaborative links, capability in, and capacity for, improve tools and infrastructure for researchers and support the Mr Willets said: “Making the most of large and complex data is a Latest discoveries medical bioinformatics. -
The Diamond Light Source
The Diamond Light Source ... a bright future for UK and World science Richard P. Walker, Technical Director What is Diamond ? • The largest scientific investment in the UK for 30 years • A synchrotron light source producing pinpoint UV and X-ray light beams of exceptional brightness • A ‘super microscope’ for new research opportunities into the structure and properties of matter What is Diamond ? • A Power Converter ! 15 MW of electrical power from the grid … 300-500 kW of X-rays … … but most of which only produces unwanted heat; only a fraction is selected for use in experiments. What is Synchrotron Radiation ? SR is electromagnetic radiation emitted when a high energy beam of charged particles (electrons) is deflected by a magnetic field. What’s so special about Synchrotron Radiation ? SR SR is emitted over a wide range of the electromagnetic spectrum, from Infra-red to hard X-rays Any desired radiation wavelength can be produced - enabling a very wide range of scientific and technological applications What’s so special about Synchrotron Radiation ? SR is very intense, and has extremely high brightness (emitted from a small area, with small angular divergence, determined by the properties of the electron beam) High brightness means: - it can be focused to sub-micron spot sizes: possibility of examining extremely small samples or investigating the structure and properties of objects with very fine spatial resolution - experiments can be carried out much more quickly: high through-put of samples or ability to follow chemical and biological reactions in real-time Diamond is a “third-generation” synchrotron radiation source • 1st generation: machines originally built for other purposes e.g. -

Science & Policy Meeting Jennifer Lippincott-Schwartz Science in The
SUMMER 2014 ISSUE 27 encounters page 9 Science in the desert EMBO | EMBL Anniversary Science & Policy Meeting pageS 2 – 3 ANNIVERSARY TH page 8 Interview Jennifer E M B O 50 Lippincott-Schwartz H ©NI Membership expansion EMBO News New funding for senior postdoctoral In perspective Georgina Ferry’s enlarges its membership into evolution, researchers. EMBO Advanced Fellowships book tells the story of the growth and ecology and neurosciences on the offer an additional two years of financial expansion of EMBO since 1964. occasion of its 50th anniversary. support to former and current EMBO Fellows. PAGES 4 – 6 PAGE 11 PAGES 16 www.embo.org HIGHLIGHTS FROM THE EMBO|EMBL ANNIVERSARY SCIENCE AND POLICY MEETING transmissible cancer: the Tasmanian devil facial Science meets policy and politics tumour disease and the canine transmissible venereal tumour. After a ceremony to unveil the 2014 marks the 50th anniversary of EMBO, the 45th anniversary of the ScienceTree (see box), an oak tree planted in soil European Molecular Biology Conference (EMBC), the organization of obtained from countries throughout the European member states who fund EMBO, and the 40th anniversary of the European Union to symbolize the importance of European integration, representatives from the govern- Molecular Biology Laboratory (EMBL). EMBO, EMBC, and EMBL recently ments of France, Luxembourg, Malta, Spain combined their efforts to put together a joint event at the EMBL Advanced and Switzerland took part in a panel discussion Training Centre in Heidelberg, Germany, on 2 and 3 July 2014. The moderated by Marja Makarow, Vice President for Research of the Academy of Finland. -

Structural Basis of Mammalian Mucin Processing by the Human Gut O
ARTICLE https://doi.org/10.1038/s41467-020-18696-y OPEN Structural basis of mammalian mucin processing by the human gut O-glycopeptidase OgpA from Akkermansia muciniphila ✉ ✉ Beatriz Trastoy 1,4, Andreas Naegeli2,4, Itxaso Anso 1,4, Jonathan Sjögren 2 & Marcelo E. Guerin 1,3 Akkermansia muciniphila is a mucin-degrading bacterium commonly found in the human gut that promotes a beneficial effect on health, likely based on the regulation of mucus thickness 1234567890():,; and gut barrier integrity, but also on the modulation of the immune system. In this work, we focus in OgpA from A. muciniphila,anO-glycopeptidase that exclusively hydrolyzes the peptide bond N-terminal to serine or threonine residues substituted with an O-glycan. We determine the high-resolution X-ray crystal structures of the unliganded form of OgpA, the complex with the glycodrosocin O-glycopeptide substrate and its product, providing a comprehensive set of snapshots of the enzyme along the catalytic cycle. In combination with O-glycopeptide chemistry, enzyme kinetics, and computational methods we unveil the molecular mechanism of O-glycan recognition and specificity for OgpA. The data also con- tribute to understanding how A. muciniphila processes mucins in the gut, as well as analysis of post-translational O-glycosylation events in proteins. 1 Structural Biology Unit, Center for Cooperative Research in Biosciences (CIC bioGUNE), Basque Research and Technology Alliance (BRTA), Bizkaia Technology Park, Building 801A, 48160 Derio, Spain. 2 Genovis AB, Box 790, 22007 Lund, Sweden. 3 IKERBASQUE, Basque Foundation for Science, 48013 ✉ Bilbao, Spain. 4These authors contributed equally: Beatriz Trastoy, Andreas Naegeli, Itxaso Anso. -

Structure and Ligand Binding of the ADP-Binding Domain of the NAD+ Riboswitch
Downloaded from rnajournal.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Structure and ligand binding of the ADP-binding domain of the NAD+ riboswitch Lin Huang1, Jia Wang and David M. J. Lilley* Cancer Research UK Nucleic Acid Structure Research Group, MSI/WTB Complex, The University of Dundee, Dow Street, Dundee DD1 5EH, U.K. * To whom correspondence should be addressed 1. Current address : Guangdong Provincial Key Laboratory of Malignant Tumor Epigenetics and Gene Regulation, Medical Research Center, Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, Guangzhou 510120 , P. R. China and RNA Biomedical Institute, Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, Guangzhou 510120, P. R. China Keywords : Riboregulation; RNA structure; X-ray crystallography; metal ions; nucleotide binding Running title: The structure of the NAD+ riboswitch Submitted to the RNA journal 20 January 2020 Editorial enquiries to Professor Lilley: Tel: (+44)-1382-384243 Email: [email protected] Downloaded from rnajournal.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press ABSTRACT The nadA motif is the first known NAD+-dependent riboswitch, comprising two similar tandem bulged stem-loop structures. We have determined the structure of the 5’ domain 1 of the riboswitch. It has three coaxial helical segments, separated by an ACANCCCC bulge and by an internal loop, with a tertiary contact between them that includes two C:G base pairs. We have determined the structure with a number of ligands related to NADH, but in each case only the ADP moiety is observed. The adenosine adopts an anti conformation, and forms multiple hydrogen bonds across the width of the sugar edge of the penultimate C:G base pair of the helix preceding the bulge, and the observed contacts have been confirmed by mutagenesis and calorimetry. -

Wellcome Trust Annual Report and Financial Statements 2019 Is © the Wellcome Trust and Is Licensed Under Creative Commons Attribution 2.0 UK
Annual Report and Financial Statements 2019 Table of contents Report from Chair 3 Report from Director 5 Trustee’s Report 7 What we do 8 Review of Charitable Activities 9 Review of Investment Activities 21 Financial Review 31 Structure and Governance 36 Social Responsibility 40 Risk Management 42 Remuneration Report 44 Remuneration Committee Report 46 Nomination Committee Report 47 Investment Committee Report 48 Audit and Risk Committee Report 49 Independent Auditor’s Report 52 Financial Statements 61 Consolidated Statement of Financial Activities 62 Consolidated Balance Sheet 63 Statement of Financial Activities of the Trust 64 Balance Sheet of the Trust 65 Consolidated Cash Flow Statement 66 Notes to the Financial Statements 67 Alternative Performance Measures and Key Performance Indicators 114 Glossary of Terms 115 Reference and Administrative Details 116 Table of Contents Wellcome Trust Annual Report 2019 | 2 Report from Chair During my tenure at Wellcome, which ends in The macro environment is increasingly challenging, 2020, I count myself lucky to have had the which has created volatility in financial markets. opportunity to meet inspiring people from a rich Q4 2018 was a very difficult quarter, but the diversity of sectors, backgrounds, specialisms resumption of interest rate cuts by the US Federal and scientific fields. Reserve underpinned another year of gains for our portfolio. We recognise that the cycle is extended, Wellcome’s achievements belong to the people and that the portfolio is likely to face more who work here and to the people we fund – it is challenging times ahead. a partnership that continues to grow stronger, more influential and more ambitious, spurred by The team is working hard to ensure that our independence. -

Delivering Novel Therapies in the 21St Century Conference Report Held on 24 – 25 October 2018
Part of the conference series Breakthrough science and technologies Transforming our future Delivering novel therapies in the 21st century Conference report Held on 24 – 25 October 2018 Supported by AstraZeneca Delivering novel therapies in the 21st century – Conference report 1 Introduction On 24 – 25 October 2018, the Royal Society and the Academy of Medical Sciences hosted a conference on novel medical therapies. The scientific programme for this meeting was developed by Steve Rees (Vice-President Discovery Biology, AstraZeneca), Professor Molly Stevens FREng (Professor of Biomedical Materials and Regenerative Medicine and Research Director for Biomedical Material Science, Imperial College London), and Sir John Skehel FMedSci FRS (Vice-President and Biological Secretary, the Royal Society). Image: Conference attendees networking. Presentations and discussions outlined recent scientific organised through the Royal Society’s Science and Industry advances in therapeutic modalities and delivery, the programme which demonstrates our commitment to integrate infrastructure required to develop novel treatments, and the science and industry at the Society, promote science and its implications of these advances for policy and healthcare value, build relationships and foster translation. delivery. The conference brought together scientists, technologists and experts from across academia, industry, The Academy’s FORUM programme brings together the NHS and public health, to discuss current challenges in industry, academia and the NHS, and the charity, regulatory human medicine, what future medicines will look like and and wider healthcare sectors. It provides an independent how we can prepare for them. platform for leaders from across the life sciences sector to discuss scientific opportunities, technology trends, This conference, supported by AstraZeneca, forms part of a translational challenges and strategic choices in healthcare.