Financing Social Protection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

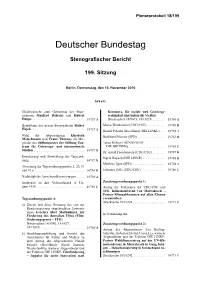
Plenarprotokoll 18/240
Plenarprotokoll 18/240 Deutscher Bundestag Stenografscher Bericht 240. Sitzung Berlin, Donnerstag, den 22. Juni 2017 Inhalt: Gedenken an Bundeskanzler a. D. Dr. Helmut Elisabeth Scharfenberg (BÜNDNIS 90/ Kohl DIE GRÜNEN) ...................... 24489 A Präsident Dr. Norbert Lammert ........... 24479 A Hermann Gröhe, Bundesminister BMG ..... 24491 B Erweiterung und Abwicklung der Tagesord- Harald Weinberg (DIE LINKE) ........... 24493 A nung. 24530 D Dr. Karl Lauterbach (SPD) ............... 24493 D Absetzung der Tagesordnungspunkte 13, 14 c, 14 d und 15 b. 24484 A Nadine Schön (St. Wendel) (CDU/CSU) .... 24495 A Mechthild Rawert (SPD). 24496 B Zur Geschäftsordnung ................. 24484 B Erich Irlstorfer (CDU/CSU) .............. 24497 A Petra Crone (SPD) ...................... 24498 A Tagesordnungspunkt 7: a) – Zweite und dritte Beratung des von der Bundesregierung eingebrachten Ent- Tagesordnungspunkt 8: wurfs eines Gesetzes zur Reform der a) Unterrichtung durch die Bundesregie- Pfegeberufe (Pfegeberufereformge- rung: Bericht zur Umsetzung der High- setz – PfBRefG) tech-Strategie – Fortschritt durch For- Drucksachen 18/7823, 18/12847 ..... 24484 C schung und Innovation – Stellungnahme – Bericht des Haushaltsausschusses ge- der Bundesregierung zum Gutachten mäß § 96 der Geschäftsordnung zu Forschung, Innovation und techno- logischer Leistungsfähigkeit Deutsch- Drucksache 18/12848 ............. 24484 C lands 2017 b) Beschlussempfehlung und Bericht des Drucksache 18/11810 ................ 24499 C Ausschusses für Gesundheit zu dem Antrag -

Vorstände Der Parlamentariergruppen in Der 18. Wahlperiode
1 Vorstände der Parlamentariergruppen in der 18. Wahlperiode Deutsch-Ägyptische Parlamentariergruppe Vorsitz: Karin Maag (CDU/CSU) stv. Vors.: Dr. h.c. Edelgard Bulmahn (SPD) stv. Vors.: Heike Hänsel (DIE LINKE.) stv. Vors.: Dr. Franziska Brantner (BÜNDNIS 90/DIE GRÜNEN) Parlamentariergruppe Arabischsprachige Staaten des Nahen Ostens (Bahrain, Irak, Jemen, Jordanien, Katar, Kuwait, Libanon, Oman, Saudi Arabien, Syrien, Vereinigte Arabische Emirate, Arbeitsgruppe Palästina) Vorsitz: Michael Hennrich (CDU/CSU) stv. Vors.: Gabriele Groneberg (SPD) stv. Vors.: Heidrun Bluhm (DIE LINKE.) stv. Vors.: Luise Amtsberg (BÜNDNIS 90/DIE GRÜNEN) Parlamentariergruppe ASEAN (Brunei, Indonesien, Kambodscha, Laos, Malaysia, Myanmar, Philippinen, Singapur, Thailand, Vietnam) Vorsitz: Dr. Thomas Gambke (BÜNDNIS 90/DIE GRÜNEN) stv. Vors.: Dr. Michael Fuchs (CDU/CSU) stv. Vors.: Johann Saathoff (SPD) stv. Vors.: Caren Lay (DIE LINKE.) Deutsch-Australisch-Neuseeländische Parlamentariergruppe (Australien, Neuseeland, Ost-Timor) Vorsitz: Volkmar Klein(CDU/CSU) stv. Vors.: Rainer Spiering (SPD) stv. Vors.: Cornelia Möhring (DIE LINKE.) stv. Vors.: Anja Hajduk (BÜNDNIS 90/DIE GRÜNEN) Deutsch-Baltische Parlamentariergruppe (Estland, Lettland, Litauen) Vorsitz: Alois Karl (CDU/CSU) stv. Vors.: René Röspel (SPD) stv. Vors.: Dr. Axel Troost (DIE LINKE.) stv. Vors.: Dr. Konstantin von Notz (BÜNDNIS 90/DIE GRÜNEN) Deutsch-Belarussische Parlamentariergruppe Vorsitz: Oliver Kaczmarek (SPD) stv. Vors.: Dr. Johann Wadephul (CDU/CSU) stv. Vors.: Andrej Hunko (DIE LINKE.) stv. Vors.: N.N. (BÜNDNIS 90/DIE GRÜNEN) 2 Deutsch-Belgisch-Luxemburgische Parlamentariergruppe (Belgien, Luxemburg) Vorsitz: Patrick Schnieder (CDU/CSU) stv. Vors.: Dr. Daniela de Ridder (SPD) stv. Vors.: Katrin Werner (DIE LINKE.) stv. Vors.: Corinna Rüffer (BÜNDNIS 90/DIE GRÜNEN) Parlamentariergruppe Bosnien und Herzegowina Vorsitz: Marieluise Beck (BÜNDNIS 90/DIE GRÜNEN) stv. -

Artikel Muster
VPT INFORMIERT Personal und Strukturen des Ausschusses für Gesundheit in der 18. Wahlperiode des Deutschen Bundestages – Vorsitz, Obleute, Berichterstatter und Sekretariat Unter Leitung des Bundestagsvizepräsidenten Johanes Singhammer (CSU) hat schlussempfehlungen an den Bundestag ̈ ̈ sich am 15. Januar 2014 der Ausschuss für Gesundheit konstituiert. Zum Vor- durfen sich nur auf die ihnen uberwiesenen Vorlagen oder mit diesen in unmittelbarem sitzenden wurde der 53-jährige promovierte Jurist Edgar Franke (SPD) bestimmt, Sachzusammenhang stehenden Fragen be- der damit die Nachfolge von Dr. Carola Reimann (SPD) antrat, die dem Ausschuss ziehen. Dies bedeutet also, dass den Aus- ̈ nicht mehr angehört und in den Vorstand der SPD-Bundestagsfraktion berufen schussen kein Initiativrecht im Plenum zu- kommt. Zu ihren Befugnissen zählt auch das wurde. Zitierrecht, wonach der Ausschuss die An- wesenheit eines Mitgliedes der Bundesre- Franke ist Rektor und Professor an der Hoch- sind bereits im 14. Jahrhundert„Standing gierung verlangen kann. Auch der Gesund- schule der Gesetzlichen Unfallversicherung Committees“ nachgewiesen. In Deutschland heitsausschuss macht von diesem Recht der in Bad Hersfeld und Mitherausgeber eines sahen Landesverfassungen des 19. Jahr- Herbeirufung aber nur selten Gebrauch, weil Lehr- und Praxiskommentars zum Siebten hunderts Ausschüsse vor. So wurden nach eine Bundesregierung um störungsfreie Buch Sozialgesetzbuch – Gesetzliche Un- einer Geschäftsordnung des Preußischen Kommunikationsflüsse zu den Ausschüssen fallversicherung. -

EU Camps in North Africa Are Pointless and Illegal "The So-Called Disembarkation Platforms Remain Nothing but Hot Air
Andrej Hunko Mitglied des Deutschen Bundestages Platz der Republik 1, 11011 Berlin Telefon030 227 – 79133 Fax30 227 – 76133 E-Mail: [email protected] Wahlkreis Augustastr. 69, 52070 Aachen Telefon 0241 9906825-0 Fax 0241 9906825-1 E-Mail: [email protected] Berlin, October 25th, 2018 Press releas EU camps in North Africa are pointless and illegal "The so-called disembarkation platforms remain nothing but hot air. Not one of the intended countries in North Africa has been asked, there is not even a diplomatic concept or timetable in the relevant EU Council working groups. And the Federal Government now only wants to talk about 'disembarkation agreements'", stated Andrej Hunko, European policy spokesman for the Left Party parliamentary group in the German Bundestag in reaction to a related response from the Federal Ministry of the Interior. The European Union is examining the establishment of "regional disembarkation centres" or "regional disembarkation platforms" in third countries. In its conclusions of 28 June 2018, the Council calls upon the Commission to examine such a concept for refugees rescued in the Mediterranean Sea, alongside the United Nations High Commission for Refugees (UNHCR) and the International Organization for Migration (IOM). According to the Ministry, to date no third country has declared itself willing to enter a "disembarkation agreement". Andrej Hunko continued: "A plan for European camps in North Africa was already floated by former Minister of the Interior Otto Schily. Yet it remains illegal, as these would perpetuate the return of those seeking protection Seite 1 von 2 Andrej Hunko Mitglied des Deutschen Bundestages Platz der Republik 1, 11011 Berlin Telefon030 227 – 79133 Fax30 227 – 76133 E-Mail: [email protected] Wahlkreis Augustastr. -

MEMORANDUM 2017 Statt „Germany First“: Alternativen Für Ein Solidarisches Europa
Neue Kleine Bibliothek 247 Arbeitsgruppe Alternative Wirtschaftspolitik MEMORANDUM 2017 Statt „Germany first“: Alternativen für ein solidarisches Europa PapyRossa Verlag © 2017 by PapyRossa Verlags GmbH & Co. KG, Köln Luxemburger Str. 202, D–50937 Köln Tel.: +49 (0) 221 – 44 85 45 Fax: +49 (0) 221 – 44 43 05 E-Mail: [email protected] Internet: www.papyrossa.de Alle Rechte vorbehalten Grafiken: Safran Works, Frankfurt/Main Druck: Interpress Die Deutsche Nationalbibliothek verzeichnet diese Publikation in der Deutschen Nationalbibliografie; detaillierte bibliografische Daten sind im Internet über http://dnb.d-nb.de abrufbar. ISBN 978-3-89438-645-0 Inhalt Vorwort 9 I. Kurzfassung des MEMORANDUM 11 II. Langfassung des MEMORANDUM 63 1 Vier Jahre Große Koalition – verpasste Chancen 65 1.1 Wirtschaftliche Rahmendaten zeigen positive Entwicklung 67 1.2 Gestaltung der Politik: Ein paar positive Ansätze, viel Austerität 71 1.3 Günstige Rahmenbedingungen ermöglichen Erfolge 75 1.4 Versäumnisse und Erfolge auf dem Arbeitsmarkt 78 1.5 Geldpolitik und Niedrigzinsen sanieren den deutschen Haushalt 83 1.6 Günstige Rahmenbedingungen – keine Fortschritte der Politik 85 2 Statt „Germany first“: Alternativen für ein solidarisches Europa 89 2.1 Die existenzielle Krise der EU 90 2.2 Das unglaubliche Ausmaß der Austeritätspolitik und ihre Folgen 91 2.3 Die Folgen des gescheiterten Krisenmanagements 95 2.4 Raus aus dem Euro? Eine Kritik an Euro-Ausstiegs- kampagnen 98 2.5 Die sieben Säulen einer radikalen Euro-Reform 101 2.6 Ausblick 126 3 Arbeitsmarkt: Entwicklung -
The Committee on Health 2 “Patients Are at the Centre of Our Health Policy
The Committee on Health 2 “Patients are at the centre of our health policy. The quality of the care they receive is the yardstick by which the organisation of our health system is judged. We would all like to live a long, healthy life, and we all wish to benefit from medical advances and the oppor tunities opened up by the digital revolution. At the same time, however, the health system must remain affordable. At the centre of these conflicting interests, the Committee on Health discusses all topics falling within its remit and prepares decisions with the aim of equipping our health system to cope with future challenges.” Erwin Rüddel, CDU/CSU Chairman of the Committee on Health 3 The German Bundestag’s decisions are prepared by its committees, which are estab lished at the start of each elec toral term. Four of them are stipulated by the Basic Law, the German constitution: the Committee on Foreign Affairs, the Defence Committee, the Committee on the Affairs of the European Union and the Petitions Committee. The Budget Committee and the Committee for the Rules of Procedure are also required by law. The spheres of respon sibility of the committees essentially reflect the Federal Government’s distribution of ministerial portfolios. This enables Parliament to scruti nise the government’s work effectively. The Bundestag committees The German Bundestag sets political priorities of its own by establishing additional committees for specific sub jects, such as sport, cultural affairs or tourism. In addition, special bodies such as parlia mentary advisory councils, The committees discuss and committees of inquiry or deliberate on items referred study commissions can also to them by the plenary. -

Plenarprotokoll 19/67
Plenarprotokoll 19/67 Deutscher Bundestag Stenografischer Bericht 67. Sitzung Berlin, Mittwoch, den 28. November 2018 Inhalt: Ausschussüberweisungen ............... 7583 A Wolfgang Kubicki (FDP) ............... 7601 C Kathrin Vogler (DIE LINKE) ............ 7602 B Tagesordnungspunkt 1: Sylvia Kotting-Uhl (BÜNDNIS 90/ DIE GRÜNEN) ..................... 7603 B Vereinbarte Debatte: Organspende 7583 B Stephan Pilsinger (CDU/CSU) ........... 7604 A Karin Maag (CDU/CSU) ............... 7583 D Detlev Spangenberg (AfD) .............. 7604 D Dr. Axel Gehrke (AfD) ................. 7584 D Hilde Mattheis (SPD) .................. 7605 C Dr. Karl Lauterbach (SPD) .............. 7585 C Dr. Claudia Schmidtke (CDU/CSU) ....... 7606 B Christine Aschenberg-Dugnus (FDP) ...... 7586 C Helge Lindh (SPD) .................... 7607 A Katja Kipping (DIE LINKE) ............ 7587 C Rudolf Henke (CDU/CSU) .............. 7608 A Annalena Baerbock (BÜNDNIS 90/ DIE GRÜNEN) ..................... 7588 B Leni Breymaier (SPD) ................. 7608 D Jens Spahn (CDU/CSU) ................ 7589 B Michael Brand (Fulda) (CDU/CSU) ....... 7609 D Paul Viktor Podolay (AfD) .............. 7590 B René Röspel (SPD) .................... 7610 D Kerstin Griese (SPD) .................. 7590 D Oliver Grundmann (CDU/CSU) .......... 7611 C Katrin Helling-Plahr (FDP) .............. 7591 C Mario Mieruch (fraktionslos) ............ 7612 B Dr. Petra Sitte (DIE LINKE) ............. 7592 B Axel Müller (CDU/CSU) ............... 7613 A Dr. Kirsten Kappert-Gonther (BÜNDNIS 90/ Thomas Rachel (CDU/CSU) -
Plenarprotokoll 18/199
Plenarprotokoll 18/199 Deutscher Bundestag Stenografischer Bericht 199. Sitzung Berlin, Donnerstag, den 10. November 2016 Inhalt: Glückwünsche zum Geburtstag der Abge- Kommerz, für soziale und Genderge- ordneten Manfred Behrens und Hubert rechtigkeit und kulturelle Vielfalt Hüppe .............................. 19757 A Drucksachen 18/8073, 18/10218 ....... 19760 A Begrüßung des neuen Abgeordneten Rainer Marco Wanderwitz (CDU/CSU) .......... 19760 B Hajek .............................. 19757 A Harald Petzold (Havelland) (DIE LINKE) .. 19762 A Wahl der Abgeordneten Elisabeth Burkhard Blienert (SPD) ................ 19763 B Motschmann und Franz Thönnes als Mit- glieder des Stiftungsrates der Stiftung Zen- Tabea Rößner (BÜNDNIS 90/ trum für Osteuropa- und internationale DIE GRÜNEN) ..................... 19765 C Studien ............................. 19757 B Dr. Astrid Freudenstein (CDU/CSU) ...... 19767 B Erweiterung und Abwicklung der Tagesord- Sigrid Hupach (DIE LINKE) ............ 19768 B nung. 19757 B Matthias Ilgen (SPD) .................. 19769 A Absetzung der Tagesordnungspunkte 5, 20, 31 und 41 a ............................. 19758 D Johannes Selle (CDU/CSU) ............. 19769 C Nachträgliche Ausschussüberweisungen ... 19759 A Gedenken an den Volksaufstand in Un- Zusatztagesordnungspunkt 1: garn 1956 ........................... 19759 C Antrag der Fraktionen der CDU/CSU und SPD: Klimakonferenz von Marrakesch – Pariser Klimaabkommen auf allen Ebenen Tagesordnungspunkt 4: vorantreiben Drucksache 18/10238 .................. 19771 C a) -

Formatvorlage Antrag (Ohne Enorm)
Deutscher Bundestag Drucksache 19/23942 19. Wahlperiode 03.11.2020 Vorabfassung Antrag der Abgeordneten Dr. Achim Kessler, Susanne Ferschl, Gökay Akbulut, Matthias W. Birkwald, Sylvia Gabelmann, Dr. André Hahn, Ulla Jelpke, Katja Kipping, Jan Korte, Jutta Krellmann, Pascal Meiser, Cornelia Möhring, Niema Movassat, Petra Pau, Martina Renner, Kersten Steinke, Friedrich Straetmanns, Jessica Tatti, Harald Weinberg, Pia Zimmermann, Sabine Zimmermann (Zwickau) und der Fraktion DIE LINKE. - wird Demokratische Kontrolle auch in der Pandemie durch Der Bundestag wolle beschließen: I. Der Deutsche Bundestag stellt fest: Die Corona-Pandemie ist auch für das politische System eine Herausforderung. die Die erste Welle hat im März zu weitgehenden Einschränkungen der persönlichen Bewegungsfreiheit der Menschen, des kulturellen und gesellschaftlichen Lebens sowie der Wirtschaft geführt. Mit der Feststellung der „epidemischen Lage von lektorierte nationaler Tragweite“ wurde das Bundesgesundheitsministerium durch den Bun- destag ermächtigt, ohne Beteiligung des Parlaments oder des Bundesrates Abwei- chungen und Ausnahmen von Gesetzen oder Einreisebestimmungen zu erlassen. Schulschließungen, Kontaktbeschränkungen, Ausgangs- und Besuchsverbote und andere Bestimmungen der Bundesländer greifen tief in essentielle Grundrechte nahezu der gesamten Bevölkerung, in soziale Sicherheiten und in ihren Alltag ein. Auch diese Maßnahmen sind zumeist ohne Beschlüsse der Landesparlamente er- lassen worden. Das widerspricht dem aus dem verfassungsmäßigen Demokratie- prinzip -

Gesamt 3. Namabst. 08.07
Seite: 1 CDU/CSU Name Ja Nein Enthaltung Ungült. Nicht abg. Ilse Aigner X Peter Altmaier X Peter Aumer X Dorothee Bär X Thomas Bareiß X Norbert Barthle X Günter Baumann X Ernst-Reinhard Beck (Reutlingen) X Manfred Behrens (Börde) X Veronika Bellmann X Dr. Christoph Bergner X Peter Beyer X Steffen Bilger X Clemens Binninger X Peter Bleser X Dr. Maria Böhmer X Wolfgang Börnsen (Bönstrup) X Wolfgang Bosbach X Norbert Brackmann X Klaus Brähmig X Michael Brand X Dr. Reinhard Brandl X Helmut Brandt X Dr. Ralf Brauksiepe X Dr. Helge Braun X Heike Brehmer X Ralph Brinkhaus X Cajus Caesar X Gitta Connemann X Alexander Dobrindt X Thomas Dörflinger X Marie-Luise Dött X Dr. Thomas Feist X Enak Ferlemann X Ingrid Fischbach X Hartwig Fischer (Göttingen) X Dirk Fischer (Hamburg) X Axel E. Fischer (Karlsruhe-Land) X Dr. Maria Flachsbarth X Klaus-Peter Flosbach X Herbert Frankenhauser X Dr. Hans-Peter Friedrich (Hof) X Michael Frieser X Erich G. Fritz X Dr. Michael Fuchs X Hans-Joachim Fuchtel X Alexander Funk X Ingo Gädechens X Dr. Peter Gauweiler X Dr. Thomas Gebhart X Norbert Geis X Alois Gerig X Eberhard Gienger X Seite: 2 CDU/CSU Name Ja Nein Enthaltung Ungült. Nicht abg. Michael Glos X Josef Göppel X Peter Götz X Dr. Wolfgang Götzer X Ute Granold X Reinhard Grindel X Hermann Gröhe X Michael Grosse-Brömer X Markus Grübel X Manfred Grund X Monika Grütters X Olav Gutting X Florian Hahn X Dr. Stephan Harbarth X Jürgen Hardt X Gerda Hasselfeldt X Dr. Matthias Heider X Helmut Heiderich X Mechthild Heil X Ursula Heinen-Esser X Frank Heinrich X Rudolf Henke X Michael Hennrich X Jürgen Herrmann X Ansgar Heveling X Ernst Hinsken X Peter Hintze X Christian Hirte X Robert Hochbaum X Karl Holmeier X Franz-Josef Holzenkamp X Joachim Hörster X Anette Hübinger X Thomas Jarzombek X Dieter Jasper X Dr. -

Stellungnahme Zur Grundsicherung
DEUTSCHER BUNDESTAG Ausschussdrucksache 19(11)1176 Ausschuss für Arbeit und Soziales 4. Juni 2021 19. Wahlperiode Schriftliche Stellungnahme Institut für Arbeitsmarkt- und Berufsforschung der Bundesagentur für Arbeit zur öffentlichen Anhörung von Sachverständigen in Berlin am 7. Juni 2021 um 12:30 Uhr zum a) Gesetzentwurf der Abgeordneten Pascal Kober, Michael Theurer, Jens Beeck, weiterer Abgeordneter und der Fraktion der FDP Entwurf eines Gesetzes zur Einführung einer Bagatellgrenze für Rückforderungen im Zweiten Sozialgesetzbuch - BT-Drucksache 19/29742 b) Antrag der Abgeordneten Ulrike Schielke-Ziesing, René Springer, Jürgen Pohl, weiterer Abgeordneter und der Fraktion der AfD Armutsbekämpfung bei Rentnern – Einführung eines 25-Prozent-Freibetrages in der Grundsicherung - BT-Drucksache 19/29768 c) Antrag der Abgeordneten Matthias W. Birkwald, Katja Kipping, Susanne Ferschl, wei- terer Abgeordneter und der Fraktion DIE LINKE. Grundsicherungskürzungen bei Rentnerinnen und Rentnern verhindern - BT-Drucksache 19/24454 d) Antrag der Abgeordneten Katja Kipping, Matthias W. Birkwald, Susanne Ferschl, wei- terer Abgeordneter und der Fraktion DIE LINKE. Hartz IV überwinden – Sanktionsfreie Mindestsicherung einführen - BT-Drucksache 19/29439 e) Antrag der Abgeordneten Sven Lehmann, Anja Hajduk, Dr. Wolfgang Strengmann- Kuhn, weiterer Abgeordneter und der Fraktion BÜNDNIS 90/DIE GRÜNEN Garantiesicherung statt Hartz IV – Mehr soziale Sicherheit während und nach der Corona-Krise - BT-Drucksache 19/25706 siehe Anlage 03.06.2021 // Öffentliche Anhörung im Bundestagsausschuss für Arbeit und Soziales am 07.06.2021 STELLUNGNAHME ZU DEN ANTRÄGEN a) der Abgeordneten Sven Lehmann, Anja Hajduk, Dr. Wolfgang Strengmann- Kuhn, Markus Kurth, Beate Müller-Gemmeke, Corinna Rüffer, Filiz Polat, Ekin Deligöz, Katharina Dröge, Claudia Müller, Lisa Paus, Stefan Schmidt, Luise Amtsberg, Kai Gehring, Britta Haßelmann, Dr. -
The Committees of the German Bundestag 2 3 Month in and Month Out, the German Bundestag Adopts New Laws Or Amends Existing Legislation
The Committees of the German Bundestag 2 3 Month in and month out, the German Bundestag adopts new laws or amends existing legislation. The Bundestag sets up permanent committees in every electoral term to assist it in accomplishing this task. In these committees, the Members concentrate on a specialised area of policy. They discuss the items referred to them by the ple- nary and draw up recommen- dations for decisions that serve as the basis for the ple- nary’s decision. The permanent committees of the German Bundestag – at the heart of Parliament’s work The Bundestag is largely free to decide how many commit- tees it establishes, a choice which depends on the priori- ties it wants to set in its par- liamentary work. There are 24 committees in the 19th electoral term. They essen- tially mirror the Federal Government’s distribution of ministerial portfolios, corre- sponding to the fields for which the ministries are The Committee on Labour and responsible. This facilitates Social Affairs and the Com- parliamentary scrutiny of the mittee on Internal Affairs and Federal Government’s work, Community have 46 members another of the Bundestag’s each, making them among the central functions. largest committees. Only the That said, in establishing com- Committee on Economic mittees, the Bundestag also Affairs and Energy has more sets political priorities of its members: 49. The Committee own. For example, the com- for the Scrutiny of Elections, mittees responsible for sport, Immunity and the Rules of tourism, or human rights and Procedure is the smallest humanitarian aid do not have committee, with 14 members.