Suprefact Depot (Buserelin)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study Protocol and Documented in the Subject Dispensing Log
Protocol Title of trial: A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism NCT number: NCT01976728 Sponsor trial code: 000070 Date: 06 Dec 2017 Gonadorelin Acetate, FE Trial Code: 000070 Date: 06 Dec 2017 999037, FE 999903 E-Protocol Amendment-21975;1.0 No Specified Dosage Form and Strength Supersedes: None Clinical Trial Protocol - Amendment 7 Page 1 of 82 CLINICAL TRIAL PROTOCOL A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism Trial Code 000070 Consolidated Protocol Incorporating Amendments 1-7 IND Number: 22,278 Investigational Medicinal Product: LutrePulse OmniPod Indication: Primary Hypothalamic Amenorrhea Phase: III Name and Address of Sponsor: Ferring International Pharmascience Center U.S., Inc. 100 Interpace Parkway Parsippany, NJ 07054 P: 973-796-1600 F: 973-796-1660 GCP Statement: This trial will be performed in compliance with GCP. The information in this document is confidential and is proprietary to Ferring International Pharmascience Center U.S. or another company within the Ferring Group. It is understood that information in this document shall not be disclosed to any third party, in any form, without prior written consent -

Hormones and Breeding
IN-DEPTH: REPRODUCTIVE ENDOCRINOLOGY Hormones and Breeding Carlos R.F. Pinto, MedVet, PhD, Diplomate ACT Author’s address: Theriogenology and Reproductive Medicine, Department of Veterinary Clinical Sciences, College of Veterinary Medicine, The Ohio State University, Columbus, OH 43210; e-mail: [email protected]. © 2013 AAEP. 1. Introduction affected by PGF treatment to induce estrus. In The administration of hormones to mares during other words, once luteolysis takes place, whether breeding management is an essential tool for equine induced by PGF treatment or occurring naturally, practitioners. Proper and timely administration of the events that follow (estrus behavior, ovulation specific hormones to broodmares may be targeted to and fertility) are essentially similar or minimally prevent reproductive disorders, to serve as an aid to affected (eg, decreased signs of behavioral estrus). treating reproductive disorders or hormonal imbal- Duration of diestrus and interovulatory intervals ances, and to optimize reproductive efficiency, for are shortened after PGF administration.1 The example, through induction of estrus or ovulation. equine corpus luteum (CL) is responsive to PGF These hormones, when administered exogenously, luteolytic effects any day after ovulation; however, act to control the duration and onset of the different only CL Ͼ5 days are responsive to one bolus injec- stages of the estrous cycle, specifically by affecting tion of PGF.2,3 Luteolysis or antiluteogenesis can duration of luteal function, hastening ovulation es- be reliably achieved in CL Ͻ5 days only if multiple pecially for timed artificial insemination and stimu- PGF treatments are administered. For that rea- lating myometrial activity in mares susceptible to or son, it became a widespread practice to administer showing delayed uterine clearance. -
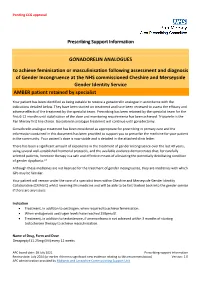
Prescribing Support Information GONADORELIN ANALOGUES To
Pending CCG approval Prescribing Support Information GONADORELIN ANALOGUES to achieve feminisation or masculinisation following assessment and diagnosis of Gender Incongruence at the NHS commissioned Cheshire and Merseyside Gender Identity Service AMBER patient retained by specialist Your patient has been identified as being suitable to receive a gonadorelin analogue in accordance with the indications detailed below. They have been started on treatment and have been reviewed to assess the efficacy and adverse effects of the treatment by the specialist team. Prescribing has been retained by the specialist team for the first 6-12 months until stabilisation of the dose and monitoring requirements has been achieved. Triptorelin is the Pan Mersey first line choice. Gonadorelin analogue treatment will continue until gonadectomy. Gonadorelin analogue treatment has been considered as appropriate for prescribing in primary care and the information contained in this document has been provided to support you to prescribe the medicine for your patient in the community. Your patient’s dose is now stable and is detailed in the attached clinic letter. There has been a significant amount of experience in the treatment of gender incongruence over the last 40 years, using several well-established hormonal protocols, and the available evidence demonstrates that, for carefully selected patients, hormone therapy is a safe and effective means of alleviating the potentially debilitating condition of gender dysphoria.1.2 Although these medicines are not licensed for the treatment of gender incongruence, they are medicines with which GPs may be familiar. Your patient will remain under the care of a specialist team within Cheshire and Merseyside Gender Identity Collaborative (CMAGIC) whilst receiving this medicine and will be able to be fast tracked back into the gender service if there are any issues. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Sgnrha-Ovarh-Study-Protocol.Pdf
STUDY PROTOCOL FOR A COMPASSIONATE AQUACULTURE INVESTIGATIONAL NEW ANIMAL DRUG (INAD) EXEMPTION FOR SALMON GONADOTROPIN-RELEASING HORMONE ® ANALOGUE (sGnRHa - OvaRH ) (INAD 012-186) Sponsor: U.S. Fish and Wildlife Service, Division of Fish Hatcheries ______________________ ___________________ Sponsor Signature Date Approved Manufacturer: Western Chemical Inc. 1269 Lattimore Road Ferndale, WA Facility for Coordination of sGnRHa (OvaRH®) INAD: Aquatic Animal Drug Approval Partnership Program 4050 Bridger Canyon Road Bozeman, Mt 59715 Proposed Starting Date September 1, 2012 Proposed Ending Date August 31, 2017 Study Director Mr. Jim Bowker _________________________ ________________ Study Director Signature Date Clinical Field Trial Location and Trial Number: __________________________________________ _________________ Type or Print Facility Name Trial Number Investigator______________________________________________________ Type or Print Name __________________________________________ _________________ Investigator Signature Date I. STUDY ID AND TITLE .................................................................................................................................. 1 II. SPONSOR..................................................................................................................................................... 1 III. INVESTIGATORS/FACILITIES .................................................................................................................... 2 IV. PROPOSED STARTING AND COMPLETION DATES: ........................................................................ -

(12) United States Patent (10) Patent No.: US 6,235,712 B1 Stevenson Et Al
US006235.712B1 (12) United States Patent (10) Patent No.: US 6,235,712 B1 Stevenson et al. (45) Date of Patent: May 22, 2001 (54) NON-AQUEOUS POLARAPROTIC PEPTIDE Helm, et al., “Stability of Gonadorelin and Triptorelin in FORMULATIONS Aqueous Solution”, Pharm. Res., 7/12, pp. 1253-1256 (1990). (75) Inventors: Cynthia L. Stevenson; Steven J. Johnson, et al., “Degradation of the LH-RHAnalog Nafare Prestrelski, both of Mountain View, CA lin Acetate in Aqueous Solution”, Intl. J. Pharm., 31, pp. (US) 125-129 (1986). 73) Assignee:9. ALZA Corporation,p Mountain View, Lupron (leuprolide acetate for Subcutaneous injection), Phy CA (US) sician's Desk Ref, 50th Ed., pp. 2555-2556 (1996). Lupron Depot (leuprolide acetate for depot Suspension), * ) Notice: Subject to anyy disclaimer, the term of this Physician's Desk Ref, 50th Ed., pp. 2556-2562 (1996). patent is extended or adjusted under 35 Lutrepulse (gonadorelin acetate for IV injection), Physi U.S.C. 154(b) by 0 days. cian's Desk Ref, 50th Ed., pp.980–982 (1996). Okada, et al., “New Degradation Product of (21) Appl. No.: 09/514,951 Des-Gly'-NH-LH-RH-Ethylamide (Fertirelin) in Aque (22) Filed: Feb. 28, 2000 ous Solution”, J. Pharm. Sci., 80/2, pp. 167–170 (1991). Okada, et al., “Preparation of Three-Month Depot Injectable Related U.S. Application Data MicroSpheres of Leuprorelin Acetate Using Biodegradable Polymers”, Pharm. Res., 11/8, pp. 1143–1147 (1994). (62) Division of application No. 09/293,839, filed on Apr. 19, 1999, now Pat. No. 6,124,261, which is a continuation of Oyler, et al., “Characterization of the Solution Degradation application No. -

Triptorelin, Goserelin and Leuprorelin for Prostate
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Study of Enteral Versus Parenteral Application of The
Journal of Reproduction and Development, Vol. 53, No. 3, 2007 —Research Note— Study of Enteral versus Parenteral Application of the Gonadotropin Releasing Hormone Agonist Gonadorelin[6-D-Phe] (D-Phe6-LHRH) on LH Secretion in Goettinger Miniature Pigs Klaus-Peter BRÜSSOW1), Ellen KANITZ2), Armin TUCHSCHERER3) and Petra TOSCH4) Departments of 1)Reproductive Biology, 2)Behavioural Physiology and 3)Genetic and Biometry, FBN Research Institute for the Biology of Farm Animals, D-18196 Dummerstorf, Germany and 4)VetCom-pharma GmbH, 6900 Bregenz, Austria Abstract. With respect to the assessment of residue situation and as a part of preclinical trials to determine the biological activities of potential gonadotropin releasing hormone (GnRH) residues in porcine organisms the GnRH agonist Gonadorelin[6-D-Phe] (D-Phe6-LHRH) was administered either enterally or intramuscularly (i.m.) to female Goettinger miniature pigs in order to evaluate the GnRH- induced luteinizing hormone (LH) surge. Gilts received an (i) enteral application of 10 mg D-Phe6- LHRH via a probang (enteral group, n=7), (ii) i.m. injection of 0.1 mg D-Phe6-LHRH (parenteral group, n= 5), or (iii) saline injection (control group, n=4). The GnRH and saline applications were repeated every second day with up to seven repetitions. Blood samples were collected via previously fitted jugular catheters immediately before injections, over an 8 h period in 1 h intervals beginning 2 h after injections, and at 24, 26, 28 and 30 h after applications. Enteral application of D-Phe6-LHRH induced an LH surge in 23 of 30 treatments. All gilts in the parenteral group exhibited LH release after each D- Phe6-LHRH application (P<0.05), whereas no LH surges were observed after saline injection in the control group. -

Gnrh Analogues for Treatment of Urinary
Europäisches Patentamt *EP001330257B1* (19) European Patent Office Office européen des brevets (11) EP 1 330 257 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: A61K 38/09, A61K 45/06, of the grant of the patent: A61P 13/00 31.08.2005 Bulletin 2005/35 (86) International application number: (21) Application number: 01975948.9 PCT/CH2001/000636 (22) Date of filing: 26.10.2001 (87) International publication number: WO 2002/036144 (10.05.2002 Gazette 2002/19) (54) GNRH ANALOGUES FOR TREATMENT OF URINARY INCONTINENCE VERWENDUNG VON GNRH-ANALOGUE ZUR BEHANDLUNG DER HARNINKONTINENZ UTILISATION D’ANALOGUES DE GNRH DANS LE TRAITEMENT DE L’INCONTINENCE URINAIRE (84) Designated Contracting States: (74) Representative: Isler & Pedrazzini AG AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU Gotthardstrasse 53 MC NL PT SE TR Postfach 6940 8002 Zürich (CH) (30) Priority: 30.10.2000 EP 00811011 (56) References cited: (43) Date of publication of application: WO-A-99/55358 30.07.2003 Bulletin 2003/31 • JANSSENS L A ET AL: "Comparisons between (73) Proprietor: UNIVERSITY OF ZURICH stress incontinence in women and sphincter 8006 Zürich (CH) mechanism incompetence in the female dog." VETERINARY RECORD, (1997 DEC 13) 141 (24) (72) Inventors: 620-5. REF: 93 , XP001061849 • ARNOLD, Susi • CONN P M ET AL: CH-5115 Möriken AG (CH) "GONADOTROPIN-RELEASINGHORMONEAND • REICHLER, Iris ITS ANALOGUES" NEW ENGLAND JOURNAL CH-8057 Zürich (CH) OF MEDICINE, THE, MASSACHUSETTS • HUBLER, Madeleine MEDICAL SOCIETY, WALTHAM, MA, US, vol. CH-8342 Wernetshausen (CH) 324, 10 January 1991 (1991-01-10), pages 93-103, XP001002186 ISSN: 0028-4793 Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. -

Luteal Support with Very Low Daily Dose of Human Chorionic Gonadotropin After Fresh Embryo Transfer As an Alternative to Cycle S
pharmaceuticals Article Luteal Support with very Low Daily Dose of Human Chorionic Gonadotropin after Fresh Embryo Transfer as an Alternative to Cycle Segmentation for High Responders Patients Undergoing Gonadotropin-Releasing Hormone Agonist-Triggered IVF Andrea Roberto Carosso 1,*,† , Stefano Canosa 1,† , Gianluca Gennarelli 1 , Marta Sestero 1, Bernadette Evangelisti 1, Lorena Charrier 2 , Loredana Bergandi 3 , Chiara Benedetto 1,‡ and Alberto Revelli 1,‡ 1 Obstetrics and Gynecology 1U, Physiopathology of Reproduction and IVF Unit, Department of Surgical Sciences, Sant’Anna Hospital, University of Torino, 10042 Turin, Italy; [email protected] (S.C.); [email protected] (G.G.); [email protected] (M.S.); [email protected] (B.E.); [email protected] (C.B.); [email protected] (A.R.) 2 Department of Public Health and Pediatrics, University of Torino, Via Santena, 5 bis, 10126 Torino, Italy; [email protected] 3 Department of Oncology, University of Torino, Via Santena 5 bis, 10126 Torino, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-333-8111155 or +39-011-3135763 † These authors contributed equally to this work. Citation: Carosso, A.R.; Canosa, S.; ‡ These authors jointly supervised this work. Gennarelli, G.; Sestero, M.; Evangelisti, B.; Charrier, L.; Bergandi, Abstract: The segmentation of the in vitro fertilization (IVF) cycle, consisting of the freezing of L.; Benedetto, C.; Revelli, A. Luteal all embryos and the postponement of embryo transfer (ET), has become popular in recent years, Support with very Low Daily Dose of Human Chorionic Gonadotropin after with the main purpose of preventing ovarian hyperstimulation syndrome (OHSS) in patients with Fresh Embryo Transfer as an high response to controlled ovarian stimulation (COS). -

Antiprogestins, a New Form of Endocrine Therapy for Human Breast Cancer1
[CANCER RESEARCH 49, 2851-2856, June 1, 1989] Antiprogestins, a New Form of Endocrine Therapy for Human Breast Cancer1 Jan G. M. Klijn,2Frank H. de Jong, Ger H. Bakker, Steven W. J. Lamberts, Cees J. Rodenburg, and Jana Alexieva-Figusch Department of Medical Oncology (Division of Endocrine Oncology) [J. G. M. K., G. H. B., C. J. K., J. A-F.J, Dr. Daniel den Hoed Cancer Center, and Department of Endocrinology ¡F.H. d. J., S. W. ]. L.J, Erasmus University, Rotterdam, The Netherlands ABSTRACT especially pronounced effects on the endometrium, decidua, ovaries, and hypothalamo-pituitary-adrenal axis. With regard The antitumor, endocrine, hematological, biochemical, and side effects of chronic second-line treatment with the antiprogestin mifepristone (RU to clinical practice, the drug has currently been used as a contraceptive agent or abortifacient as a result of its antipro 486) were investigated in 11 postmenopausal patients with metastatic breast cancer. We observed one objective response, 6 instances of short- gestational properties (2, 22-24). Based on its antiglucocorti term stable disease, and 4 instances of progressive disease. Mean plasma coid properties, this drug has been used or has been proposed concentrations of adrenocorticotropic hormone (/' < 0.05), cortisol (/' < for treatment of conditions related to excess corticosteroid 0.001), androstenedione (/' < 0.01), and estradici (P < 0.002) increased production such as Cushing's syndrome (19, 25-27) and for significantly during treatment accompanied by a slight decrease of sex treatment of lymphomas (24) and glaucoma (28); because of its hormone binding globulin levels, while basal and stimulated gonadotropi effects on the immune system, the drug has been suggested to levels did not change significantly.