DRUG NAME: Goserelin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hormones and Breeding
IN-DEPTH: REPRODUCTIVE ENDOCRINOLOGY Hormones and Breeding Carlos R.F. Pinto, MedVet, PhD, Diplomate ACT Author’s address: Theriogenology and Reproductive Medicine, Department of Veterinary Clinical Sciences, College of Veterinary Medicine, The Ohio State University, Columbus, OH 43210; e-mail: [email protected]. © 2013 AAEP. 1. Introduction affected by PGF treatment to induce estrus. In The administration of hormones to mares during other words, once luteolysis takes place, whether breeding management is an essential tool for equine induced by PGF treatment or occurring naturally, practitioners. Proper and timely administration of the events that follow (estrus behavior, ovulation specific hormones to broodmares may be targeted to and fertility) are essentially similar or minimally prevent reproductive disorders, to serve as an aid to affected (eg, decreased signs of behavioral estrus). treating reproductive disorders or hormonal imbal- Duration of diestrus and interovulatory intervals ances, and to optimize reproductive efficiency, for are shortened after PGF administration.1 The example, through induction of estrus or ovulation. equine corpus luteum (CL) is responsive to PGF These hormones, when administered exogenously, luteolytic effects any day after ovulation; however, act to control the duration and onset of the different only CL Ͼ5 days are responsive to one bolus injec- stages of the estrous cycle, specifically by affecting tion of PGF.2,3 Luteolysis or antiluteogenesis can duration of luteal function, hastening ovulation es- be reliably achieved in CL Ͻ5 days only if multiple pecially for timed artificial insemination and stimu- PGF treatments are administered. For that rea- lating myometrial activity in mares susceptible to or son, it became a widespread practice to administer showing delayed uterine clearance. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Altered Cognitive Function in Men Treated for Prostate
Altered Cognitive Function in Men Treated for Prostate Cancer with LHRH Analogues and Cyproterone Acetate: A Randomised Controlled Trial H. J. Green PhD1,2, K. I. Pakenham PhD1, B. C. Headley PhD3, J. Yaxley FRACS3, D. L. Nicol FRACS2,4, P. N. Mactaggart FRACS2,5, C. Swanson PhD2, R. B. W atson FRACS6, & R. A. Gardiner MD2,3 1School of Psychology and 2Department of Surgery, The University of Queensland, 3Royal Brisbane, 4Princess Alexandra, 5Queen Elizabeth II & 6Mater Hospitals, Brisbane, Queensland, Australia In conjunction with the Northern Section of the Urological Society of Australasia Correspondence should be addressed to: Dr R. A. Gardiner, Department of Surgery, The University of Queensland, Brisbane, Qld 4072, Australia Fax: +61 7 3365 5559; Phone: +61 7 3365 5233; Email: f.gardiner@ mailbox.uq.edu.au This work was wholly funded by Queensland Cancer Fund. **PREPRINT. Final version published in British Journal of Urology (BJU: International) (2002), 90, 427-432 ** Short Title: COGNITIVE CHANGES W ITH HORMONAL MEDICATION 2 Objective. Luteinising hormone releasing hormone (LHRH) analogues have been associated with memory impairments in women using these drugs for gynaecological conditions. This is the first systematic investigation of the cognitive effects of LHRH analogues in male patients. Methods. 82 men with non-localised prostate cancer were randomly assigned to receive continuous leuprorelin (LHRH analogue), goserelin (LHRH analogue), cyproterone acetate (steroidal antiandrogen) or close clinical monitoring. These patients underwent cognitive assessments at baseline and before commencement of treatment (77) then 6 months later (65). Results. Compared with baseline assessments, men administered androgen suppression monotherapy performed worse in 2/12 tests of attention and memory. -

Goserelin (Zoladex)
Goserelin (Zoladex) This booklet explains what goserelin is, when it may be prescribed, how it works and what side effects may occur. Goserelin is the generic (non‑branded) name of the drug and how it’s referred to in this booklet. Its current brand name is Zoladex. This information is by Breast Cancer Care. We are the only specialist UK‑wide charity that supports people affected by breast cancer. We’ve been supporting them, their family and friends and campaigning on their behalf since 1973. Today, we continue to offer reliable information and personal support, over the phone and online, from nurses and people who’ve been there. We also offer local support across the UK. From the moment you notice something isn’t right, through to treatment and beyond, we’re here to help you feel more in control. For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancercare.org.uk Visit breastcancercare.org.uk 3 What is goserelin? Goserelin is a type of hormone therapy used to treat breast cancer in pre-menopausal women (women who have not been through the menopause). It is given as an injection into the abdomen (belly). It can also be used to try to preserve fertility during chemotherapy (see page 4). Goserelin as a treatment for breast cancer How does it work? Some breast cancers are stimulated to grow by the hormone oestrogen. Before the menopause, oestrogen is mainly produced in the ovaries. Goserelin switches off this production by interfering with hormone signals from the brain that control how the ovaries work. -
Triptorelin, Goserelin and Leuprorelin for Prostate
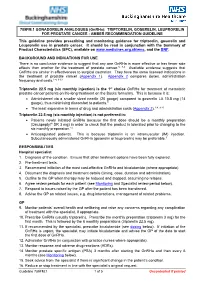
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Luteal Support with Very Low Daily Dose of Human Chorionic Gonadotropin After Fresh Embryo Transfer As an Alternative to Cycle S
pharmaceuticals Article Luteal Support with very Low Daily Dose of Human Chorionic Gonadotropin after Fresh Embryo Transfer as an Alternative to Cycle Segmentation for High Responders Patients Undergoing Gonadotropin-Releasing Hormone Agonist-Triggered IVF Andrea Roberto Carosso 1,*,† , Stefano Canosa 1,† , Gianluca Gennarelli 1 , Marta Sestero 1, Bernadette Evangelisti 1, Lorena Charrier 2 , Loredana Bergandi 3 , Chiara Benedetto 1,‡ and Alberto Revelli 1,‡ 1 Obstetrics and Gynecology 1U, Physiopathology of Reproduction and IVF Unit, Department of Surgical Sciences, Sant’Anna Hospital, University of Torino, 10042 Turin, Italy; [email protected] (S.C.); [email protected] (G.G.); [email protected] (M.S.); [email protected] (B.E.); [email protected] (C.B.); [email protected] (A.R.) 2 Department of Public Health and Pediatrics, University of Torino, Via Santena, 5 bis, 10126 Torino, Italy; [email protected] 3 Department of Oncology, University of Torino, Via Santena 5 bis, 10126 Torino, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-333-8111155 or +39-011-3135763 † These authors contributed equally to this work. Citation: Carosso, A.R.; Canosa, S.; ‡ These authors jointly supervised this work. Gennarelli, G.; Sestero, M.; Evangelisti, B.; Charrier, L.; Bergandi, Abstract: The segmentation of the in vitro fertilization (IVF) cycle, consisting of the freezing of L.; Benedetto, C.; Revelli, A. Luteal all embryos and the postponement of embryo transfer (ET), has become popular in recent years, Support with very Low Daily Dose of Human Chorionic Gonadotropin after with the main purpose of preventing ovarian hyperstimulation syndrome (OHSS) in patients with Fresh Embryo Transfer as an high response to controlled ovarian stimulation (COS). -

Antiprogestins, a New Form of Endocrine Therapy for Human Breast Cancer1
[CANCER RESEARCH 49, 2851-2856, June 1, 1989] Antiprogestins, a New Form of Endocrine Therapy for Human Breast Cancer1 Jan G. M. Klijn,2Frank H. de Jong, Ger H. Bakker, Steven W. J. Lamberts, Cees J. Rodenburg, and Jana Alexieva-Figusch Department of Medical Oncology (Division of Endocrine Oncology) [J. G. M. K., G. H. B., C. J. K., J. A-F.J, Dr. Daniel den Hoed Cancer Center, and Department of Endocrinology ¡F.H. d. J., S. W. ]. L.J, Erasmus University, Rotterdam, The Netherlands ABSTRACT especially pronounced effects on the endometrium, decidua, ovaries, and hypothalamo-pituitary-adrenal axis. With regard The antitumor, endocrine, hematological, biochemical, and side effects of chronic second-line treatment with the antiprogestin mifepristone (RU to clinical practice, the drug has currently been used as a contraceptive agent or abortifacient as a result of its antipro 486) were investigated in 11 postmenopausal patients with metastatic breast cancer. We observed one objective response, 6 instances of short- gestational properties (2, 22-24). Based on its antiglucocorti term stable disease, and 4 instances of progressive disease. Mean plasma coid properties, this drug has been used or has been proposed concentrations of adrenocorticotropic hormone (/' < 0.05), cortisol (/' < for treatment of conditions related to excess corticosteroid 0.001), androstenedione (/' < 0.01), and estradici (P < 0.002) increased production such as Cushing's syndrome (19, 25-27) and for significantly during treatment accompanied by a slight decrease of sex treatment of lymphomas (24) and glaucoma (28); because of its hormone binding globulin levels, while basal and stimulated gonadotropi effects on the immune system, the drug has been suggested to levels did not change significantly. -
![1 SUPPLEMENTARY DATA Draft Medline Search – Pubmed Interface 1# "Puberty"[Mesh] OR (Puberties) OR (Pubertal Maturati](https://docslib.b-cdn.net/cover/5679/1-supplementary-data-draft-medline-search-pubmed-interface-1-puberty-mesh-or-puberties-or-pubertal-maturati-1835679.webp)
1 SUPPLEMENTARY DATA Draft Medline Search – Pubmed Interface 1# "Puberty"[Mesh] OR (Puberties) OR (Pubertal Maturati
SUPPLEMENTARY DATA Draft Medline search – PubMed interface 1# "Puberty"[Mesh] OR (Puberties) OR (Pubertal Maturation) OR (Early Puberty) OR "Puberty, Precocious"[Mesh] OR (Precocious Puberty) OR "Precocious Puberty, Central" [Supplementary Concept] OR (Central Precocious Puberty) OR "Sexual precocity" [Supplementary Concept] OR (Idiopathic sexual precocity) OR (Familial precocious puberty) OR (Sexual Precocity) OR "Sexual Maturation"[Mesh] OR (Maturation, Sexual) OR (Maturation, Sex) OR (Sex Maturation) OR "Sexual Development"[Mesh] OR (Development, Sexual) OR (Sex Development) OR (Development, Sex) OR (Gonadal Disorder Maturation) OR (Pubertal Onset) OR "Menstruation Disturbances"[Mesh] OR (Precocious Menses) OR (Early Menses) OR (Early Menarche) OR (Precocious Menarche) OR (Disorders of Puberty) OR (Gonadotropin-Dependent Precocious Puberty) OR (Gonadotropin-Independent Precocious Puberty) OR (Isolated Precocious Thelarche) OR (Isolated Precocious Pubarche) OR (Isolated Precocious Menarche) 2# "Gonadotropin-Releasing Hormone"[Mesh] OR (Gonadotropin Releasing Hormone) OR (Luteinizing Hormone-Releasing Hormone) OR (Luteinizing Hormone Releasing Hormone) OR (GnRH) OR (Gonadoliberin) OR (Gonadorelin) OR (LFRH) OR (LH-FSH Releasing Hormone) OR (LH FSH Releasing Hormone) OR (LH-Releasing Hormone) OR (LH Releasing Hormone) OR (LH-RH) OR (LHFSH Releasing Hormone) OR (Releasing Hormone, LHFSH) OR (LHFSHRH) OR (LHRH) OR (Luliberin) OR (FSH-Releasing Hormone) OR (FSH Releasing Hormone) OR (Gn-RH) OR (Factrel) OR (Gonadorelin Acetate) OR (Kryptocur) -

Luteinising Hormone-Releasing Hormone (LHRH) Agonists in Prostate Cancer This Bulletin Focuses on Luteinising Hormone-Releasing Hormone (LHRH) Agonists
B88 | April 2015 | 2.1 Community Interest Company Luteinising hormone-releasing hormone (LHRH) agonists in prostate cancer This bulletin focuses on luteinising hormone-releasing hormone (LHRH) agonists. Currently goserelin and leuprorelin (administered 4 weekly or 12 weekly and monthly or 3 monthly respectively) are the two LHRH agonists used primarily in the management of prostate cancer across England (88% share, ePACT October to December 2014). Triptorelin is also used for prostate cancer and has published data to confirm its efficacy. However triptorelin only accounts for 12% (ePACT October to December 2014) of all LHRH agonist usage. Across England, a switch from 12 weekly goserelin and 3 monthly leuprorelin to 12 weekly or 6 monthly triptorelin could result in an annual saving of £6.8 million (ePACT October to December 2014). Support materials (including the secondary care bulletin: Bulletin 28 Secondary care KPI support bulletins. Gonadorelin analogues – reduced usage of Zoladex) are available at http://www.prescqipp.info Recommendations • Engage and establish opinion with local Trust urologists on preferred formulary choices of LHRH agonists. This should take into account dosage intervals, administration, product price, and fees paid for administration. Local decision making may also be affected by local discounts and rebate scheme activity. • 3 monthly and 6 monthly triptorelin and 3 monthly leuprorelin are the preferred cost effective LHRH agonists for prostate cancer in new patients. • Switch guidance will need to be agreed by local Trust urologists for existing patients and should be considered at the next clinic appointment. • Use 12 weekly/3 monthly or 6 monthly injections in preference to 4 weekly/monthly injections to support administration, convenience to the patient and costs. -

The Effects of Different Gonadotropin Releasing Hormone Analogues in IVF Cycles
Vol. 10, No. 3, 2005 Middle East Fertility Society Journal © Copyright Middle East Fertility Society The effects of different gonadotropin releasing hormone analogues in IVF cycles Cem Fiçicioğlu, M.D., Ph.D., Assoc.Prof. Seval Taşdemir, M.D. Tayfun Kutlu, M.D. Leyla Altuntaş, M.D. Zeynep Kamil Women and Children's Hospital, Reproductive Medicine-Infertility & IVF unit, Istanbul. ABSTRACT Objective: To compare Triptorelin, Leuprolide acetate and Nafarelin sodium in women undergoing controlled ovarian hyperstimulation for in vitro fertilization cycles. Settings: Zeynep Kamil Women and Children's Hospital Reproductive Endocrinology - Infertility - IVF Center. Material and Methods: Sixty patients were haphazardly distributed for each GnRH-a group. GnRH-a was administrated, starting on the 21st day of menstrual cycles for the long protocol: Triptorelin (Decapeptyl, 0.1 mg) as 0.1 mg/day SC, leuprolide (Lucrine, 5 mg flacon) as 0.5 mg/day SC and nafarelin (Synarel, 2 mg/mi nasal spray) as 200 micrograms to each nostril with a daily total dosage of 800 micrograms. The responses from each group were compared on the basis of duration of stimulation, total dosage of gonadotropin, E2 values on day 5, the down regulation duration, cyst formation, E2 values on the 1st day of stimulation and HCG, progesterone values and endometrial thickness on the HCG day, the number oocytes picked up, fertilization rates, the number of transferred embryos, pregnancy and implantation ratios. Results: Evaluating Triptorelin (T), Leuprolide (LA) and Nafarelin (NA) groups respectively, E2 values on the 1st day of menstrual cycles, measured to confirm the down regulation for each GnRH-a, were 24.67 pg/ml, 21.23 pg/ml, 29.62 pg/ml (p<0.05); the total gonadotropin usage (ampoules) were 47.15 ± 12.97, 39.45 ± 13.97, 36.72 ± 13.14 (p<0.05); the number of retrieved oocytes were 9,89 ± 5,98, 10,50 ± 3,69 and 9,19 ± 5,31 (p>0,05); the fertilization rates were 89%, 100% and 100% (p>0.05).