Peripheral Nerve Blockade and the Effects of Paraesthesiae
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nerve Ultrasound in Dorsal Root Ganglion Disorders: Smaller Nerves Lead to Bigger Insights
Clinical Neurophysiology 130 (2019) 550–551 Contents lists available at ScienceDirect Clinical Neurophysiology journal homepage: www.elsevier.com/locate/clinph Editorial Nerve ultrasound in dorsal root ganglion disorders: Smaller nerves lead to bigger insights See Article, pages 568–572 After decades of having to make do with electric stimulation representing the fascicles, bundled together in a large outer cable and recording (i.e. nerve conduction studies, electromyography sheath (van Alfen et al., 2018). and evoked potentials), nerve ultrasound now provides the oppor- Next, it is important to realize what the ratio between axon/ tunity to improve neurodiagnostic patient care by deploying a myelin and connective tissue in a given nerve segment is, and powerful tool to detect neuromuscular pathology in an accurate how that ratio changes from the proximal root to the distal end and patient-friendly way (Mah et al., 2018; Walker et al., 2018). branches (Schraut et al., 2016). Connective tissue elements of the Nerve ultrasound is also increasingly providing neurologists and perineurium and epineurium are relatively sparse at the very prox- clinical neurophysiologists with the opportunity to increase their imal root and plexus levels, with an average connective tissue con- insight in the pathophysiology of peripheral nervous system tent of around 25–30%. Ultrasonographically, this means that roots (PNS) pathology. In this issue of Clinical Neurophysiology, Leadbet- will always look rather black in appearance without much dis- ter and coworkers (Leadbetter et al., 2019) describe the results of cernible fascicular architecture, as the sparseness of connective tis- their study on nerve ultrasound for diagnosing sensory neuronopa- sue elements provides relatively few reflectors to create an image thy in spinocerebellar ataxia type 2 and CANVAS syndrome. -

Spinal Nerves, Ganglia, and Nerve Plexus Spinal Nerves
Chapter 13 Spinal Nerves, Ganglia, and Nerve Plexus Spinal Nerves Posterior Spinous process of vertebra Posterior root Deep muscles of back Posterior ramus Spinal cord Transverse process of vertebra Posterior root ganglion Spinal nerve Anterior ramus Meningeal branch Communicating rami Anterior root Vertebral body Sympathetic ganglion Anterior General Anatomy of Nerves and Ganglia • Spinal cord communicates with the rest of the body by way of spinal nerves • nerve = a cordlike organ composed of numerous nerve fibers (axons) bound together by connective tissue – mixed nerves contain both afferent (sensory) and efferent (motor) fibers – composed of thousands of fibers carrying currents in opposite directions Anatomy of a Nerve Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Epineurium Perineurium Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Endoneurium Nerve Rootlets fiber Posterior root Fascicle Posterior root ganglion Anterior Blood root vessels Spinal nerve (b) Copyright by R.G. Kessel and R.H. Kardon, Tissues and Organs: A Text-Atlas of Scanning Electron Microscopy, 1979, W.H. Freeman, All rights reserved Blood vessels Fascicle Epineurium Perineurium Unmyelinated nerve fibers Myelinated nerve fibers (a) Endoneurium Myelin General Anatomy of Nerves and Ganglia • nerves of peripheral nervous system are ensheathed in Schwann cells – forms neurilemma and often a myelin sheath around the axon – external to neurilemma, each fiber is surrounded by -

The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -
PN1 (Midha) Microanatomy of Peripheral Nerves-Part1.Pdf
Peripheral Nerve Basics • Consist of processes of cell bodies found in the DRG, anterior horn, and autonomic ganglia • Organized by several distinct connective tissue layers – the epineurium, perineurium, and endoneurium • Vascular supply provided by the vasa nervorum Peripheral Nerve Basics • Neuronal processes bound into fascicles by perineurium • Fascicles bound into nerves by epineurium • Endoneurium is a division of the perineurium which form thin layers of connective tissue surrounding neuronal fibers in a fascicle Sural nerve in cross-section Epineurium • Loose areolar tissue with sparse, longitudinally-oriented collagen fibers • Some elastic fibers where epineurium abuts perineurium • Able to accommodate a significant amount of nerve stretching and movement • Increases in thickness where nerves cross joints • Constitutes an increasing proportion of nerves as they increase in size • Epineurial fat helps cushion nerves from compressive injury • Decreased epineurial fat found in patients with diabetes Perineurium • Cellular component composed of laminated fibroblasts of up to 15 layers in thickness which are bounded by a basal lamina • Semi-permeable: inner lamellae have tight junctions, providing a barrier to intercellular transport of macromolecules – Tight junctions can be loosened with topical anaesthetics and with osmotic change Perineurium • Exhibits a slightly positive internal pressure – Fascicular contents herniate upon perineurial injury • Under tension longitudinally – Nerve segment shortens upon transection – may complicate surgical repair as nerve can be stretched only approximately 10% before being inhibited by collagen Endoneurium • Intrafascicular connective tissue consisting of a collagenous matrix in the interstitial space • Develops into partitions of dense connective tissue between diverging fascicles and eventually becomes perineurium when the fascicles separate • Collagen fibers are longitudinally-oriented and run along nerve fibers and capillaries. -

Nerve and Nerve Injuries” Sunderland : 50 Years Later
2019 Nerve and Nerve Injuries” Sunderland : 50 years later Faye Chiou Tan, MD Professor, Dir. EDX, H. Ben Taub PMR, Baylor College of Medicine Chief PMR, Dir. EDX, Harris Health System 2019 Financial Disclosure • Elsevier Book Royalties for “EMG Secrets” textbook • Revance, consultation panel 2019 Warning Videotaping or taking pictures of the slides associated with this presentation is prohibited. The information on the slides is copyrighted and cannot be used without permission and author attribution. Introduction – Sydney Sunderland was Professor of Experimental Neurology at the University of Melbourne. – His textbook “Nerve and Nerve lnjuries” published in 1968 is no longer in print (copies $1000 on the internet) – Here is a review as relates to new technology: Ultrahigh frequency musculoskeletal ultrasound Part I – I. Anatomic and physiologic features of A. Peripheral nerve fibers B. Peripheral nerve trunks I.A. Peripheral nerve fibers – Axoplasm – Increased flow of cytoplasm from cell body into axons during electrical stimulation (Grande and Richter 1950) – Although overall proximal to distal axoplasmic flow, the pattern of streaming in the axon is bidirectional and faster (up to 3-7 cm/day) (Lubinska 1964). I. A. Peripheral nerve fibers – Sheath – Myelinated – Length of internode elongates with growth (Vizoso and Young 1948, Siminoff 1965) – In contrast, remyelination in adults produce short internodes of same length (Leegarrd 1880, Young 1945,…) – Incisures of Schmidt-Lantermann are clefts conical clefts that open when a nerve trunk is stretched thereby preventing distortion of myelin. (Glees, 1943) Schmidt-Lantermann Clefts Sunderland S. Nerve and Nerve Injuries, Sunderland, Livingstone,LTD, Edinburgh/London, 1968, p. 8 I. A. -

Modulatory Roles of ATP and Adenosine in Cholinergic Neuromuscular Transmission
International Journal of Molecular Sciences Review Modulatory Roles of ATP and Adenosine in Cholinergic Neuromuscular Transmission Ayrat U. Ziganshin 1,* , Adel E. Khairullin 2, Charles H. V. Hoyle 1 and Sergey N. Grishin 3 1 Department of Pharmacology, Kazan State Medical University, 49 Butlerov Street, 420012 Kazan, Russia; [email protected] 2 Department of Biochemistry, Laboratory and Clinical Diagnostics, Kazan State Medical University, 49 Butlerov Street, 420012 Kazan, Russia; [email protected] 3 Department of Medical and Biological Physics with Computer Science and Medical Equipment, Kazan State Medical University, 49 Butlerov Street, 420012 Kazan, Russia; [email protected] * Correspondence: [email protected]; Tel.: +7-843-236-0512 Received: 30 June 2020; Accepted: 1 September 2020; Published: 3 September 2020 Abstract: A review of the data on the modulatory action of adenosine 5’-triphosphate (ATP), the main co-transmitter with acetylcholine, and adenosine, the final ATP metabolite in the synaptic cleft, on neuromuscular transmission is presented. The effects of these endogenous modulators on pre- and post-synaptic processes are discussed. The contribution of purines to the processes of quantal and non- quantal secretion of acetylcholine into the synaptic cleft, as well as the influence of the postsynaptic effects of ATP and adenosine on the functioning of cholinergic receptors, are evaluated. As usual, the P2-receptor-mediated influence is minimal under physiological conditions, but it becomes very important in some pathophysiological situations such as hypothermia, stress, or ischemia. There are some data demonstrating the same in neuromuscular transmission. It is suggested that the role of endogenous purines is primarily to provide a safety factor for the efficiency of cholinergic neuromuscular transmission. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

The Coolest Innovation in Pain Management
A NEW WAY TO FREEZE OUT Provides Temporary POST-OPERATIVE PAIN. Post-Operative Pain Relief Cryo Nerve Block (cryoNB) harnesses the power of cryotherapy to provide a new form of temporary pain relief for patients who undergo certain invasive cardiac or thoracic surgical procedures. This technology uses a unique freezing method to temporarily block pain signals from nerves in the affected area, providing an effect that’s similar to a local anesthetic. ATRICURE, INC. Indications for Use: AtriCure’s cryoICE� cryoSPHERE™ cryoablation probes are sterile, single use devices 7555 Innovation Way intended for use in blocking pain by temporarily ablating Mason, Ohio 45040 peripheral nerves. The Coolest Innovation +1 (513) 755-4100 Please review the Instructions for Use for a complete +1 (888) 347-6403 listing of contraindications, warnings, precautions and potential adverse events prior to using these devices. in Pain Management. Customer Service / Product Inquiries Rx Only. Phone: +1 (866) 349-2342 Fax: +1 (513) 755-4567 PM-US-0017A-0920-G HOW cryoNB WORKS. 2 / STOPPING THE PAIN SIGNALS A NEW APPLICATION FOR Freezing blocks pain signals, which originate from a structure within the A PROVEN TECHNOLOGY. 1 / FREEZING THE NERVE nerve called the axon. The axons subsequently degenerate while leaving the A surgical probe delivers extremely cold temperature to nerve tissue in the tubule structures (epineurium, perineurium, endoneurium) intact for the Cryotherapy was originally developed as a treatment for cardiac nerves around the surgical incision. axons to regenerate within. arrhythmias. AtriCure consulted with leading pain management experts to develop new techniques for applying cryoNB to nerves, specifically in order to block pain. -

Journal of Biomechanical Science and Engineering Researches on Biomechanical Properties and Models of Peripheral Nerves
Bulletin of the JSME Vol.12, No.1, 2017 Journal of Biomechanical Science and Engineering 【Review Paper】 Researches on biomechanical properties and models of peripheral nerves - a review Ming-Shaung JU*, Chou-Ching K. LIN** and Cheng-Tao CHANG* *Department of Mechanical Engineering, National Cheng Kung University 1 University Road, Tainan 701, Taiwan (R.O.C.) E-mail: [email protected] **Department of Neurology College of Medicine and University Hospital National Cheng Kung University 1 University Road, Tainan 701, Taiwan (R.O.C.) Received: 14 December 2016; Revised: 11 February 2017; Accepted: 6 March 2017 Abstract The biomechanics of peripheral nerve plays an important role in physiology of the healthy and pathology of the diseased such as the diabetic neuropathy, the cauda equine compression and the carpal tunnel syndrome. The other application is recent development of neural prostheses. The goal of this paper is to review researches done by members of Taiwanese Society of Biomechanics on the biomechanics of peripheral nerves in the past two decades. First, a brief introduction of the anatomy of peripheral nerve is given. Then experiment designs and mechanical models for testing the nerves are presented. The material properties ranged from linear elastic to nonlinear visco-elastic and scales ranged from organ level to tissue level are reviewed. Implications of these studies to clinical problems will be addressed and the challenges and future perspective on biomechanics of peripheral nerve are discussed. Key words: Biomechanics, Peripheral nerve, Review, Diabetic mellitus, Cauda equine 1. Introduction Nervous system plays an important role in the human body it can coordinate voluntary and involuntary actions of other tissues and sub-systems. -
The “Road Map”
PRACTICAL ROADMAP NERVOUS TISSUE DR N GRAVETT NEURONS • MOTOR • SENSORY Anterior (ventral) horn Dorsal root of spinal of spinal cord cord Multipolar Pseudounipolar ANTERIOR HORN CELLS • Slide 64 Spinal Cord (vervet monkey) Stain: Kluver and Berrera Technique NOTE: with this technique, myelin stains dark blue and basophilic substances such as rER and nuclei stain violet. In this case we use “blue” and “purple” to describe the staining and not eosinophilic and basophilic. SPINAL CORD Anterior Ventral Horn Arachnoid Ventricle Pia Mater Grey Matter White Matter Posterior Horn Dura Mater Dorsal ANTERIOR HORN CELL Neuropil Cell Body Dendrite Vesicular Nucleus Nucleolus Nucleus of Nissl Bodies Neuroglial Cell ANTERIOR HORN CELL Neuropil Cell Body Vesicular Nucleus Nucleolus Nissl Body Nucleus of Neuroglial Cell Dendrite Nissl Body Axon Hillock Axon SPINAL (DORSAL ROOT) GANGLION CELLS • Slide 62 Spinal Ganglion Stain: H&E NOTE: The spinal ganglion is also known as the dorsal root ganglia and contains pseudounipolar neuron cell bodies. SPINAL (DORSAL ROOT) GANGLIA Cell Bodies Processes (Axons and Dendrites) SPINAL (DORSAL ROOT) GANGLIA Cell Bodies Processes (Axons and Dendrites) NOTE: The neuronal cell bodies of the dorsal root ganglia are “clumped” together, and one cannot see any processes entering or leaving the cell bodies. The processes (axons and dendrites) are seen towards the edge/periphery of the group of cell bodies. SPINAL (DORSAL ROOT) GANGLIA Satellite cells (arranged in ring like fashion around the cell body) Cell Body Nucleolus Vesicular Fine Granular Nucleus Nissl Substance Nucleus of Satellite cell PERIPHERAL BRANCH OF A SPINAL NERVE • Slide 32 Median Nerve Stain: Mallory’s Technique NOTE: Three dyes are used in Mallory’s technique, which results in collagen fibres (such as connective tissue) staining blue, the “neurokeratin” staining red, and nuclei staining reddish-orange PERIPHERAL NERVE Myelinated Axons Vein L.S. -

School of Physical Education and Sports Science
ARISTOTELIAN UNIVERSITY OF THESSALONIKI School of Physical Education and Sports Science Bachelor's Thesis: "MYOFASCIAL NETWORK IN PHYSICAL ACTIVITY AND TRAINING" Name: Tsourvakas Konstantinos Supervisor: Papadopoulos Panagiotis PhD Thessaloniki, June 2018 1 ABSTRACT Physical activity can lead people, regardless of age, to a healthier and more quality life. Especially nowadays, that most people follow an intense routine, good physical condition is an essential factor to take care of in order to achieve health and well- being. This project refers to the myofascial system of the human body. It is about a scientific review whose purpose is to highlight the importance of self myofascial release (SMR), to quote the process of SMR through the use of specific tools and methods, and the analysis of its effects to the human body. In the first place, the fascial network of the human body is described, along with the properties, the function and the usefulness of the fascia. Subsequently, the assignment focuses on the significance of self myofascial release for the human body and mostly the way it increases and improves the range of motion. In addition, there is a presentation of SMR's techniques and methods with the application of tools such as foam rollers, roller massagers and tennis balls. The assignment ends up with conclusions and suggestions on further improvement of range of motion. 2 TABLE OF CONTENTS Abstract……………………………………………………………………….………2 Table of Contents ……………………….......………………………………………...3 1. Introduction...………………………………………………………………..……...4 2. The Fascial System………………………………………………..………………..5 2.1 Definition….…………………………………………………..…………………..5 2.2 Structure….……………………………………………………………..…………5 2.3 Function………………………………………………………………..…………22 3. Importance of training fascia …………….....……………………………………..27 3.1 Principles of training fascia....................................................................................27 3.2 Fascia and elastic recoil.........................................................................................31 4. -
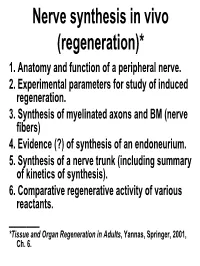
Lecture 19: Nerve Synthesis in Vivo (Regeneration)
Nerve synthesis in vivo (regeneration)* 1. Anatomy and function of a peripheral nerve. 2. Experimental parameters for study of induced regeneration. 3. Synthesis of myelinated axons and BM (nerve fibers) 4. Evidence (?) of synthesis of an endoneurium. 5. Synthesis of a nerve trunk (including summary of kinetics of synthesis). 6. Comparative regenerative activity of various reactants. _______ *Tissue and Organ Regeneration in Adults, Yannas, Springer, 2001, Ch. 6. 1. Anatomy and function of a peripheral nerve. I Nervous system = central nervous system (CNS) + peripheral nervous system (PNS) Image: public domain (by Wikipedia User: Persion Poet Gal) Nervous System: CNS and PNS CNS PNS Chamberlain, Yannas, et al., 1998 Landstrom, Aria. “Nerve Regeneration Induced by Collagen-GAG Matrix in Collagen Tubes.” MS Thesis, MIT, 1994. Focus of interest: nerve fibers and axons Nerve fibers comprise axons wrapped in a myelin sheath, itself surrounded by BM (diam. 10-30 μm in rat sciatic nerve). Axons are extensions (long processes) of neurons located in spinal cord. They comprise endoplasmic reticulum and microtubules. 1. Anatomy and function of a peripheral nerve. II Myelinated axons (diam. 1-15 μm) are wrapped in a myelin sheath; nonmyelinated axons also exist. They are the elementary units for conduction of electric signals in the body. Myelin formed by wrapping a Schwann cell membrane many times around axon perimeter. No ECM inside nerve fibers. Myelin sheath is a wrapping of Schwann cell membranes around certain axons. 1. Anatomy and function of a peripheral nerve. III Nonmyelinated axons (diam. <1 μm) function in small pain nerves. Although surrounded by Schwann cells, they lack myelin sheath; Schwann cells are around them but have retained their cytoplasm.