Improving Meal Context in Nursing Homes. Impact of Four Strategies on Food Intake and Meal Pleasure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Simple Vinaigrette
Simple Vinaigrette The usual ratio is 1 part vinegar to 3 parts oil, but I prefer 1 part vinegar to 2 parts oil. The important thing is to play around until you find your favorite ratio. • 1 large spoon Red Wine Vinegar • Any red wine vinegar will do, but if you can find unpasteurized red wine vinegar, it will have more flavor • Plus, since it contains the mother, you can use it to make your own vinegar. Just add wine (I use red wine, whatever remnants we have) and let is sit a few months. Taste it periodically. • Sherry Wine Vinegar is also exceptionally good • 2 large spoons Extra Virgin Olive Oil • When you buy olive oil, check to see if there is a harvest date. Olive oil is good for you. You get the most nutritional value in the year after harvest *** Put a little salt in a bowl I recommend unrefined coarse grey salt because it has a high mineral content, but any salt will do; you can also add pepper Add 1 large spoon Red Wine Vinegar Plus a little Dijon mustard (Maille, Amora, Edmond Fallot, Grey Poupon) Stir it and let sit a few minutes Optional, classic additions, to add to the vinegar, salt, mustard: • Garlic: • Either as a clove you let sit in vinegar for gentle flavor • Or pounded to a paste in mortar/grated in a suribachi for a stronger flavor • You can also mince it or microplane it • Shallot • Sliced thinly; if your shallot is very large, use a quarter of half The vinegar will soften the garlic and shallot flavor; you can use either alone/or both garlic and shallot together I usually let this sit 5 or so minutes, while I prepare something else. -

28St Brunch 07-20.Pages
brunch TARALLUCCI E VINO UOVA ETC. PIATTI PREZZO FISSO INSALATA 15 BOSTON BIBB LETTUCE, HAZELNUTS, RADISH, 1 UOVA ETC. ITEM UOVA AL TARTUFO 15 UOVA E PROSCIUTTO 12 PARMIGIANO, HOUSE VINAIGRETTE 1 PASTRY ITEM HOUSEMADE BRIOCHE, SCRAMBLED EGGS, SCRAMBLED EGGS, PROSCIUTTO DI PARMA, 1 MIMOSA OR BELLINI ROSEMARY HAM, PROVOLONE, AIOLI, TOMATOES, PARMIGIANO, INSALATA DI SALMONE 23 COFFEE OR ESPRESSO TRUFFLE AIOLI, HOME FRIES HOUSEMADE BRIOCHE OR CROISSANT SEARED SALMON, KALE, SHAVED FENNEL, RADISH, LEMON VINAIGRETTE 24 YOGURT E CEREALI 10 QUICHE 12 RUCOLA 14 HOUSEMADE GRANOLA, YOGURT, BACON OR VEGETARIAN QUICHE, BABY ARUGULA, SHAVED FENNEL, WALNUTS, MIXED BERRIES BABY GREEN SALAD SALUMI E FORMAGGI POMEGRANATE SEEDS, ITALIAN FETA CHEF’S SELECTION OF UOVA E PANCETTA 12 UOVA E ASPARAGI 14 BURRATA 18 5 SALUMI & CHEESES BURRATA, ROASTED BABY BEETS, SUNNY-SIDE UP EGGS, SMOKED BACON, POACHED EGGS, ASPARAGUS, PISTACHIOS, ACETO BALSAMICO 30 ARUGULA, TOMATOES, AIOLI POTATOES, PARMIGIANO, HERBS POLIPO 20 OMELETTE 12 FRENCH TOAST 15 CHARRED OCTOPUS, CELERY, PASTICCERIA FILLED WITH CHOICE OF TWO: HOUSEMADE BRIOCHE FRENCH TOAST, CHERRY TOMATOES, POTATOES All our pastries are baked in house ZUCCHINI, MUSHROOM, SPINACH, TOMATO, BANANAS, WALNUTS, BACON, GOAT CHEESE, PARMIGIANO MASCARPON POLPETTINE 15 FRENCH CROISSANT 3.25 HOUSEMADE BEEF MEATBALLS, SAN MARZANO TOMATOES, PARMIGIANO ALMOND CROISSANT 3.75 UOVA E POLENTA 14 UOVA E SALMONE 14 OTTO FILE POLENTA, POACHED EGGS, BABY KALE, PAIN AU CHOCOLAT 3.25 SPAGHETTI AL POMODORO 19 POACHED EGGS, WILD MUSHROOMS, SMOKED -

Port, Sherry, Sp~R~T5, Vermouth Ete Wines and Coolers Cakes, Buns and Pastr~Es Miscellaneous Pasta, Rice and Gra~Ns Preserves An
51241 ADULT DIETARY SURVEY BRAND CODE LIST Round 4: July 1987 Page Brands for Food Group Alcohol~c dr~nks Bl07 Beer. lager and c~der B 116 Port, sherry, sp~r~t5, vermouth ete B 113 Wines and coolers B94 Beverages B15 B~Bcuits B8 Bread and rolls B12 Breakfast cereals B29 cakes, buns and pastr~es B39 Cheese B46 Cheese d~shes B86 Confect~onery B46 Egg d~shes B47 Fat.s B61 F~sh and f~sh products B76 Fru~t B32 Meat and neat products B34 Milk and cream B126 Miscellaneous B79 Nuts Bl o.m brands B4 Pasta, rice and gra~ns B83 Preserves and sweet sauces B31 Pudd,ngs and fru~t p~es B120 Sauces. p~ckles and savoury spreads B98 Soft dr~nks. fru~t and vegetable Ju~ces B125 Soups B81 Sugars and artif~c~al sweeteners B65 vegetables B 106 Water B42 Yoghurt and ~ce cream 1 The follow~ng ~tems do not have brand names and should be coded 9999 ~n the 'brand cod~ng column' ~. Items wh~ch are sold loose, not pre-packed. Fresh pasta, sold loose unwrapped bread and rolls; unbranded bread and rolls Fresh cakes, buns and pastr~es, NOT pre-packed Fresh fru~t p1es and pudd1ngs, NOT pre-packed Cheese, NOT pre-packed Fresh egg dishes, and fresh cheese d1shes (ie not frozen), NOT pre-packed; includes fresh ~tems purchased from del~catessen counter Fresh meat and meat products, NOT pre-packed; ~ncludes fresh items purchased from del~catessen counter Fresh f1sh and f~sh products, NOT pre-packed Fish cakes, f1sh fingers and frozen fish SOLD LOOSE Nuts, sold loose, NOT pre-packed 1~. -

Harvest Bristol Delivery Pricelist Printed On:
Harvest Bristol Delivery Pricelist Printed on: ############# Prices are correct at time of printing but can change without notification Price per unit or Kilo if Bulk BABY & CHILD 60791 BABY NEUTRAL HAIR BODY SHAMPOO - LAVERA £8.99 60794 BABY NEUTRAL NAPPY CREAM - LAVERA £8.45 T059P BABY WIPES ORGANIC COTTON - NATRACARE £3.95 HS880781 BEDTIME BUBBLE BATH MILD-ORG- MUMMA LOVE £4.99 X613P BUBBLE BATH (ORG) - BEAMING BABY £6.45 WEL088 CALENDULA NAPPY CREAM £7.20 G45113 COTTON PATCHES FOR KIDS -ORG- ORGANII £3.95 X640P DEGRADABLE NAPPY SACKS - BEAMING BABY £2.99 X379P JUNIOR NAPPIES - BEAMING BABY £13.99 X377P MAXI NAPPIES - BEAMING BABY £12.99 X378P MAXI PLUS NAPPIES - BEAMING BABY £14.45 X376P MIDI NAPPIES - BEAMING BABY £12.99 X375P MINI NAPPIES - BEAMING BABY £5.98 ENV030 TOOTHBRUSH ENVIRONMENTAL CHILD £2.99 KVV030 VITAL VITS KIDS MULTI 30S HIGHER NATURE £8.39 BODY PRODUCTS T665P 1N BLACK - HERBATINT £9.45 T666P 2N BROWN - HERBATINT £9.49 T727P 3N DARK CHESTNUT - HERBATINT £9.49 T670P 4N CHESTNUT- HERBATINT £9.49 T675P 5N LIGHT CHESTNUT HERBATINT £9.50 T677P 6D DARK GOLDEN BLONDE- HERBATINT £8.85 T678P 6N DARK BLONDE - HERBATINT £10.08 T679P 7D GOLDEN BLONDE HAIR DYE- HERBATINT £9.49 T684P 8N LIGHT BLONDE- HERBATINT £8.85 G11103 AFTER SUN CREAM 50ML -ORG- ORGANII £3.50 T150P ALMOND SOAP (ROUND) - RAMPAL LATOU £3.85 WEL144 ALMOND SOOTHING FACIAL LOTION - WELEDA £17.95 GP414 ALOE CALENDULA AFTER SUN - GREEN PEOPLE £15.95 G11081 ALOE EUCALYPTUS MOUTHWASH-ORG- ORGANII £5.59 URT630 ALOE VERA BODY LOTION -ORG- URTEKRAM £6.99 T671P ALOE VERA -

28Th St. Brunch 5.15
UOVA ETC. UOVA AL TARTUFO 15 UOVA E PROSCIUTTO 10 SCRAMBLED EGGS, HERB-COOKED HAM, SCRAMBLED EGGS, PROSCIUTTO DI PARMA, PROVOLONE, BLACK TRUFFLE AIOLI, AIOLI, TOMATOES, PARMIGIANO, HOUSE BRIOCHE, HOME FRIES HOUSE MADE BRIOCHE OR CROISSANT UOVA E ASPARAGI 12 OMELETTE 12 FILLED WITH CHOICE OF TWO: 44 East 28th St. POACHED EGGS, ASPARAGUS, POTATOES, ZUCCHINI, MUSHROOM, SPINACH, TOMATO, PARMIGIANO, HERBS 212.779.1100 BACON, GOAT CHEESE, PARMIGIANO www.taralluccievino.net UOVA E PANCETTA 12 QUICHE 10 SUNNY-SIDE UP EGGS, SMOKED BACON, BACON OR VEGETARIAN QUICHE SERVED WITH ARUGULA, TOMATOES, AIOLI SIDE SALAD PREZZO FISSO FRUTTA 10 YOGURT E CEREALI 10 SEASONAL FRUIT PLATE GRANOLA, YOGURT, HONEY, SEASONAL FRUIT 1 UOVA ETC. ITEM 1 PASTRY ITEM FRITTATA ALLA NORCINA 14 FRENCH TOAST 14 COFFEE OR ESPRESSO SWEET SAUSAGE, POTATOES, HOUSE BRIOCHE FRENCH TOAST, BANANAS, 19 BLACK TRUFFLE WALNUTS, MASCARPONE BRUNCH COCKTAILS SALUMI E FORMAGGI AMORA 12 THE ZIPPER 12 CHEF’S SELECTION OF 5 CACHACA, SAGE BLACKBERRIES TEQUILA, TOUCH OF CAMPARI, SALUMI & CHEESES PINEAPPLE, JALAPEÑO AGAVE 30 SUNDOWN 12 THE GONDOLA 12 CAMPARI, GRAPEFRUIT, LIME, RASPBERRIES, SELECT, ORANGE PROSECCO JUICE, PROSECCO ROSÉ SANGRIA 40 PASTICCERIA Pitcher serves four ROSÉ WINE, ROSATO VERMOUTH, SEASONAL FRUIT CESTINO DI PASTICCERIA 10 BASKET OF FOUR PASTRIES FRENCH CROISSANT 3 INSALATE ALMOND CROISSANT 3.5 CAVOLO NERO 14 QUINOA 14 PAIN AU CHOCOLAT 3 KALE, SHAVED FENNEL, DRY CRANBERRIES, WHITE QUINOA, ROASTED BABY CARROTS, LEMON CITRONETTE, PINOLI NUTS YOGURT VINAIGRETTE, HERBS WHOLE WHEAT -

FRENCH FEAST PRODUCT LIST Fall 2013 Contents Pommery Mustards and Vinegars
FRENCH FEAST PRODUCT LIST Fall 2013 Contents Pommery Mustards and Vinegars..............................................................................................................4 Amora Mustard..........................................................................................................................................7 Melfor Alsatian Vinegars...........................................................................................................................8 Domaine du Siorac Verjus (Verjuice).........................................................................................................9 Gonet Yellow Wine Vinegar.....................................................................................................................10 Vilux Vinegars, Cornichons, Onions, and Capers....................................................................................11 La Marne Champagne Vinegar................................................................................................................12 Bénédicta Sauces......................................................................................................................................13 Hénaff Pâtés.............................................................................................................................................14 Rougié Duck Confit, Duck Fat, and Pâtés...............................................................................................15 Elevages Périgord Foie Gras and Pâtés....................................................................................................16 -
In Stock Product List April 8, 2020
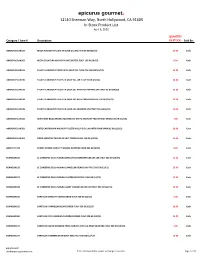
epicurus gourmet. 12140 Sherman Way, North Hollywood, CA 91605 In Stock Product List April 8, 2020 QUANTITY Category / Item # Description: IN STOCK: Sold By: ANCHOVIES:AN155 RECCA ANCHOVY FILLETS IN OLIVE OIL ITALY TIN 56 GR (25/CS) 20.00 Each ANCHOVIES:AN163 RECCA COLATURA ANCHOVY JUICE BOTTLE ITALY 100 ML (6/CS) 6.00 Each ANCHOVIES:AN185 TALATTA ANCHOVY PASTE WITH OLIVE OIL TUBE ITALY 60 GR (24/CS) 38.00 Each ANCHOVIES:AN190 TALATTA ANCHOVY FILLETS IN OLIVE OIL JAR ITALY 95 GR (24/CS) 28.00 Each ANCHOVIES:AN191 TALATTA ANCHOVY FILLETS IN OLIVE OIL WITH HOT PEPPERS JAR ITALY 95 GR (24/CS) 23.00 Each ANCHOVIES:AN192 TALATTA ANCHOVY FILLETS IN OLIVE OIL WITH CAPERS JAR ITALY 95 GR (24/CS) 12.00 Each ANCHOVIES:AN195 TALATTA ANCHOVY FILLETS IN OLIVE OIL HERMETIC JAR ITALY 235 GR (6/CS) 10.00 Each ANCHOVIES:AN325 BENFUMAT BOQUERONES MARINATED WHITE ANCHOVY FILLETS TRAY SPAIN 130 GR (10/CS) 7.00 Each ANCHOVIES:AN350 ORTIZ CANTABRIAN ANCHOVY FILLETS IN OLIVE OIL JAR WITH FORK SPAIN 95 GR (15/CS) 29.00 Each ANCHOVIES:AN365 ORTIZ ANCHOVY PACKED IN SALT POUCH SPAIN 120 GR (12/CS) 16.00 Each BARLEY:TL175 PURPLE PRAIRIE BARLEY TIMELESS NATURAL FOOD 454 GR (8/CS) 8.00 Each BEANS:BN125 LE CONSERVE DELLA NONNA BORLOTTI (CRANBERRY) BEANS JAR ITALY 360 GR (12/CS) 11.00 Each BEANS:BN126 LE CONSERVE DELLA NONNA CANNELLINI BEANS JAR ITALY 360 GR (12/CS) 25.00 Each BEANS:BN127 LE CONSERVE DELLA NONNA CHICKPEAS JAR ITALY 360 GR (12/CS) 17.00 Each BEANS:BN128 LE CONSERVE DELLA NONNA GIANT CORONA BEANS JAR ITALY 360 GR (12/CS) 13.00 Each BEANS:BN150 BARTOLINI BORLOTTI BEANS DRIED ITALY 500 GR (12/CS) 1.00 Each BEANS:BN155 BARTOLINI CANNELLINI BEANS DRIED ITALY 500 GR (12/CS) 18.00 Each BEANS:BN160 BARTOLINI CECI UMBRIAN CHICKPEAS DRIED ITALY 500 GR (12/CS) 24.00 Each BEANS:BN170 BARTOLINI QUICK COOKING PEARL BARLEY, LENTIL & BEAN SOUP MIX ITALY 500 GR (12/CS) 4.00 Each BEANS:BN175 BARTOLINI FARMERS BEAN SOUP MIX ITALY 500 GR (12/CS) 14.00 Each 818-658-3637 [email protected] Prices and availability subject to change at anytime. -

View Gift Guide
Your passport to Culinary Adventures READY FOR ADVENTURE? | We've packed this year's guide with our best and brightest mustards and gourmet essentials, ready to whisk you away on a world-wide mustard adventure. Mustard as an ingredient highlights the cuisines of Europe, Asia, Africa and the Americas. As a condiment, it’s the choice of chefs around the globe. Grab your passport and let’s explore together on this Incredible Tasteful Adventure! Bon voyage and bon appétit! — Patti B., owner of the Mustard Museum Gourmet Gift Shop and online store Mustard Bites photos by Focal Flame Photography MUSTARD BITES: A Tasteful Adventure THE EXPERIENCE | We are super proud to be launching our signature mustard & gourmet tasting bites. Inspired by nine of our best mustards, this one-of-a-kind culinary experience at the Mustard Museum pairs these 9 faves with 9 specifically-curated bites. Visit mustardmuseum.com/mustardbites! THE GIFT SET | Bring the experience home. Nine “Mustard Bites” mustards featuring information cards that include tasting notes, pairing advice, recipe ideas and mustard maker fun facts. Experience a tasteful adventure at home, or give as a gift! Mustard Bites gift box $84.95 MBA999 Or buy ‘Mustard Bites’ individually: Ringhands Beer Mustard $6.50 RHB100; Aunty Lilikoi Passion Fruit Wasabi Mustard $12.50 ALK100; Delicae Gourmet Sun-Dried Tomato & Olive Mustard $8.50 DCA144; Pommery Moutarde Royale $22 PMM125; Kelley’s Gourmet Stoneground Mustard $5.75 KGM100; Fox More Than A Mustard $7.75 FOX100; Cherchies Banana Pepper Mustard $7.75 CHC105; Daddy Cook’s Exotic Ginger Curry $8.50 DDC103; Dr. -

ENTRADAS STARTERS Codfish Cakes and “Aïoli” Sauce Tomato and Port Wine Reduction Saint John Sardine Croquettes with Toast
ENTRADAS STARTERS AS NOSSAS BEBIDAS OUR DRINKS COUVERT - 3,50€ WINES Pão, azeitona e amuse-bouche /Bread, olive and amuse-bouche ESPUMANTE / SPARKLING WINE DE BEBIDAS COMPLETA COMPLETA BEBIDAS DE CARTA NOSSA A CONSULTE POR PESSOA | PER PERSON MENU DRINKS COMPLETE OUR SEE MENU EXPRESS Monção e Melgaço | Soalheiro Bruto 2018 - 9€ / 32€ SELEÇÃO DE CHARCUTARIA BÍSARO/Bísaro charcuterie selection - 14€ / 22€ EXPRESS MENU CHAMPANHE / CHAMPAGNE BOLINHOS DE BACALHAU E MOLHO “AÏOLI” - 8€ Reims | Billecart-Salmon Brut Reserve NV - 16€ / 68€ Codfish cakes and “Aïoli” sauce Disponível das 12h00 às 15h00 / Available from 12h00 to 15h00 Reims | Billecart-Salmon Brut Rosé NV - 25€ / 122€ BURRATA - 14€ VINHO ROSÉ / ROSE WINE Tomate coração de boi e redução de Vinho do Porto ENTRADA E PRATO PRINCIPAL Provence | M de Minuty 2018 - 7€ / 25€ Tomato and Port Wine reduction OU PRATO PRINCIPAL E SOBREMESA - 14€ VINHO BRANCO / WHITE WINE Starter and main or main and dessert CROQUETES DE SARDINHA DE SÃO JOÃO COM TOSTAS - 12€ Douro | Alves de Sousa Estação - 5€ / 18€ Saint John sardine croquettes with toast Trás-os-Montes | V Valpaços 2016 - 5€ / 18€ ENTRADA, PRATO PRINCIPAL E SOBREMESA - 16€ Dão | Quinta de Saes Encruzado 2016 - 9€ / 32€ WRAP DE ATUM E ABACATE COM BATATAS FRITAS - 9€ Starter, main and dessert Tuna and avocado wrap with french fries VINHO TINTO / RED WINE GASPACHO VERDE E TOSTA DE REQUEIJÃO - 8€ Douro | Quinta do Cidrô Rufete 2013 - 9€ / 32€ Green gazpacho and curd cheese toast Dão | Dom Bella 2013 - 11€ / 46€ Alentejo | Dona Maria Touriga Nacional -

Epicurus Gourmet. 12140 Sherman Way, North Hollywood, CA 91605 "In Stock" Product List March 5, 2019
epicurus gourmet. 12140 Sherman Way, North Hollywood, CA 91605 "In Stock" Product List March 5, 2019 Join our QTY In Sold Mailing List Item # Description: Stock: By: for Prices! ANCHOVIES:AN120 FLOTT ANCHOVY PASTE WITH OLIVE OIL TUBE ITALY 60 GR (45/CS) 5.00 Each ANCHOVIES:AN155 RECCA ANCHOVY FILLETS IN OLIVE OIL ITALY TIN 56 GR (25/CS) 20.00 Each ANCHOVIES:AN163 RECCA COLATURA ANCHOVY JUICE BOTTLE ITALY 100 ML (6/CS) 7.00 Each ANCHOVIES:AN185 TALATTA ANCHOVY PASTE WITH OLIVE OIL TUBE ITALY 60 GR (24/CS) 32.00 Each ANCHOVIES:AN190 TALATTA ANCHOVY FILLETS IN OLIVE OIL JAR ITALY 95 GR (24/CS) 42.00 Each ANCHOVIES:AN191 TALATTA ANCHOVY FILLETS IN OLIVE OIL WITH HOT PEPPERS JAR ITALY 95 GR (24/CS) 19.00 Each ANCHOVIES:AN325 BENFUMAT BOQUERONES MARINATED WHITE ANCHOVY FILLETS TRAY SPAIN 130 GR (10/CS) 4.00 Each ANCHOVIES:AN330 BOQUERONES MARINATED WHITE ANCHOVY FILLETS SPAIN 700 GR (8/CS) 7.00 Each ANCHOVIES:AN350 ORTIZ CANTABRIAN ANCHOVY FILLETS IN OLIVE OIL JAR WITH FORK SPAIN 95 GR (15/CS) 21.00 Each ANCHOVIES:AN365 ORTIZ ANCHOVY PACKED IN SALT POUCH SPAIN 120 GR (12/CS) 7.00 Each BBQ SAUCE:KZ270 KOZLIK'S CAROLINA BBQ SAUCE JAR CANADA 470 ML (6/CS) 13.00 Each BBQ SAUCE:KZ275 KOZLIK'S WHISKEY MAPLE BBQ SAUCE JAR CANADA 470 ML (6/CS) 3.00 Each BEANS:BN125 LE CONSERVE DELLA NONNA BORLOTTI (CRANBERRY) BEANS JAR ITALY 360 GR (12/CS) 10.00 Each BEANS:BN126 LE CONSERVE DELLA NONNA CANNELLINI BEANS JAR ITALY 360 GR (12/CS) 26.00 Each BEANS:BN127 LE CONSERVE DELLA NONNA CHICKPEAS JAR ITALY 360 GR (12/CS) 30.00 Each BEANS:BN128 LE CONSERVE DELLA -

Culinary Catalogue
CULINARY CATALOGUE CULINARY Chef Middle East takes pride in being an integrated part of bringing our customers food creativity the elements that makes their dish stand out – that “special something”, that flavour solution, the accompanying side, both the big and the small that in combination creates those intricate flavour experiences that makes consumers come back for more. The variety of ingredients that can be serviced to your food operation from Chef Middle East is in the thousands, accessed through our global sourcing network and brought to your kitchen with the well-known Chef service. We will be more than happy to respond to your requests for specific ingredients, the products that are not depicted in this catalogue are almost with certainty within our reach and ability to source for you. Let Chef Middle East help you complete your product range! OUR BRANDS INDEX BEVERAGE SELECTION BEVERAGE STILL WATER STILL WATER 24018 24 x 500ml Antipodes 24022 12 x 1000ml Antipodes SPARKLING WATER SPARKLING WATER 24019 24 x 500ml Antipodes 24021 12 x 1000ml Antipodes 6 DRESSING, STOCK & SAUCES SELECTION DRESSING, STOCK & SAUCES BASE CHICKEN STOCK POWDER LOBSTER BASE BEEF BASE ARABIA 21476 1100g Knorr 10285 1lb Custom Culinary 24755 400g Custom Culinary BEEF STOCK POWDER ARABIA MIREPOIX BASE CHICKEN BASE 21813 1100g Knorr 10286 1lb Custom Culinary 10282 1lb Custom Culinary FISH STOCK POWDER MUSHROOM BASE CHICKEN POWDER (no added MSG) 20565 1100g Knorr 10287 1lb Custom Culinary 23997 1kg Knorr CHICKEN STOCK CUBES LIQUID CONCENTRATE VEGETABLE STOCK -

Bottle Conditioned Cocktails
BOTTLE CONDITIONED COCKTAILS Introducing our seasonal selection of bottle conditioned cocktails. Each of the below has been created for your enjoyment - rested in bottles and poured straight over ice. Available as a single drink £13 or bottle serve £120. CHERRY BLOSSOM NEGRONI Bombay Sapphire gin, Martini Riserva Speciale Rubino & Martini Riserva Speciale Bitter. Infused with cherry blossom. PIÑA COLADA OLD FASHIONED Bacardi Añejo Cuatro and Carta Negra rums. Infused with pineapple and burnt coconut with a touch of salted maple. COFFEE & CHOCOLATE BOULEVARDIER Monkey Shoulder Scotch whisky, Campari, Punt e Mes & chocolate bitters. Slow dripped through roasted Asháninka Peruvian coffee. COCKTAILS SIGNATURE SERVES Cocktails created over the years at our SUSHISAMBA locations, by our bar team – both past and present. SAMBA SOUR Fresh, Citrus, Velvety £15 A modern Pisco Sour, for the modern Pisco Sour drinker. BarSol Primera Quebranta pisco, Maraschino liqueur and turmeric, shaken hard with Japanese citrus and egg whites. CHUCUMBER Fresh, Light, Vegetal £14 Takara Yokaichi Imo shōchū, maraschino liqueur, plum sake and bitters. Shaken with fresh cucumber. TOM YAM Fresh, Fiery, Cooling £15 Hendrick’s gin, coriander infusion, chili, lemongrass and lime leaf. Churned through crushed ice, with ginger syrup and citrus juice. Served long. NINA FRESA® Fruity, Bitter, Sweet £14 Russian Standard Platinum vodka, strawberry, grapefruit and guava, shaken with rhubarb bitters, lime and sugar. NASHI MARTINI Light, Fresh £15 Grey Goose La Poire vodka, St. Germain elderflower liqueur and plum sake. Stirred with lychee water, passion fruit syrup and Japanese citrus. KAFFIRINHA Fragrant, Herbaceous £14 Our creative take on the Brazilian Classic. Fragrant Kaffir lime leaves infused in Velho Barreiro cachaça, churned with lime and sugar and served short, over crushed ice.