Inconsistent Descriptions of Lumbar Multifidus Morphology: a Scoping Review Anke Hofste1,2*, Remko Soer1,2, Hermie J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Thoracic and Lumbar Spine Anatomy
ThoracicThoracic andand LumbarLumbar SpineSpine AnatomyAnatomy www.fisiokinesiterapia.biz ThoracicThoracic VertebraeVertebrae Bodies Pedicles Laminae Spinous Processes Transverse Processes Inferior & Superior Facets Distinguishing Feature – Costal Fovea T1 T2-T8 T9-12 ThoracicThoracic VertebraeVertebrae andand RibRib JunctionJunction FunctionsFunctions ofof ThoracicThoracic SpineSpine – Costovertebral Joint – Costotransverse Joint MotionsMotions – All available – Flexion and extension limited – T7-T12 LumbarLumbar SpineSpine BodiesBodies PediclesPedicles LaminaeLaminae TransverseTransverse ProcessProcess SpinousSpinous ProcessProcess ArticularArticular FacetsFacets LumbarLumbar SpineSpine ThoracolumbarThoracolumbar FasciaFascia LumbarLumbar SpineSpine IliolumbarIliolumbar LigamentsLigaments FunctionsFunctions ofof LumbarLumbar SpineSpine – Resistance of anterior translation – Resisting Rotation – Weight Support – Motion IntervertebralIntervertebral DisksDisks RatioRatio betweenbetween diskdisk thicknessthickness andand vertebralvertebral bodybody heightheight DiskDisk CompositionComposition – Nucleus pulposis – Annulus Fibrosis SpinalSpinal LigamentsLigaments AnteriorAnterior LongitudinalLongitudinal PosteriorPosterior LongitudinalLongitudinal LigamentumLigamentum FlavumFlavum InterspinousInterspinous LigamentsLigaments SupraspinousSupraspinous LigamentsLigaments IntertransverseIntertransverse LigamentsLigaments SpinalSpinal CurvesCurves PosteriorPosterior ViewView SagittalSagittal ViewView – Primary – Secondary -

Trunk Control During Gait: Walking with Wide and Narrow Step Widths Present Distinct 4 Challenges 5 6 Hai-Jung Steffi Shih, James Gordon, Kornelia Kulig
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.30.274423; this version posted November 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Original Article 2 3 Trunk Control during Gait: Walking with Wide and Narrow Step Widths Present Distinct 4 Challenges 5 6 Hai-Jung Steffi Shih, James Gordon, Kornelia Kulig 7 Division of Biokinesiology and Physical Therapy, University of Southern California, Los Angeles, 8 CA, USA 9 10 11 Corresponding Author: 12 Hai-Jung Steffi Shih 13 Address: 1540 E. Alcazar St, CHP 155, Los Angeles, CA, 90033 14 Telephone: +1 (323)442-2089 15 Fax: +1 (323)442-1515 16 Email: [email protected] 17 18 19 Keywords: Gait stability, Lateral stability, Trunk coordination, Muscle activation, Foot placement 20 Word count (intro-discussion): 3519 21 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.30.274423; this version posted November 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 22 Abstract 23 The active control of the trunk plays an important role in frontal plane gait stability. We 24 characterized trunk control in response to different step widths using a novel feedback system 25 and examined the different effects of wide and narrow step widths as they each present unique 26 task demands. -

Indications and Treatment of Myofascial Pain
2/25/2017 Indications and Treatment of Myofascial Pain Lisa DeStefano, DO Associate Professor and Chair Department of Osteopathic Manipulative Medicine College of Osteopathic Medicine Michigan State University Common Myofascial Pain Syndromes 1 2/25/2017 2 2/25/2017 Greater Occipital Nerve Impingement Sites . 1: Origin of the third occipital nerve and proximal connection with the greater occipital nerve. 2: Greater occipital nerve as it courses inferior to the inferior oblique muscle. 3: Greater occipital nerve coursing through the semispinalis capitis muscle. 4: Greater occipital nerve exiting the aponeurosis of the trapezius muscle. 5: Greater occipital nerve traveling with the occipital artery. 6: Origin of the greater occipital nerve and relationship to the descending branch of the occipital artery. 7: Suboccipital nerve relation to the vertebral artery and the descending branch of the occipital artery and this nerves interconnection to the greater occipital nerve. 8: Relationship between the third occipital nerve and the C2‐C3 joint complex. Common Treatment Approaches • MFR • MET • Soft Tissue Release • Counterstain • HVLA Etiology of Head and Neck Myofascial Pain Syndromes • Overuse • Posture –Head over the pelvis • Posture – Scapular function • Occlusion –how the teeth control for the proper placement of the mandibular condyle. 3 2/25/2017 Stabilization of the torsobegins with spinotransverse muscle transmission of force onto the epaxial fascia or vertebral aponeurosis. 4 2/25/2017 This then transmits tension into the serratus posterior superior and inferior, which then lifts the upper four ribs and sternum and lowers the lower ribs respectively. In response a force‐ couple is generated between the serratus posterior inferior fascia, external oblique fascia, and the rectus sheath. -

Quantification of the Elastic Moduli of Lumbar Erector Spinae And
applied sciences Article Quantification of the Elastic Moduli of Lumbar Erector Spinae and Multifidus Muscles Using Shear-Wave Ultrasound Elastography Tae Hyun Lim 1, Deukhee Lee 2,3 , Olga Kim 1,3 and Song Joo Lee 1,3,* 1 Center for Bionics, Biomedical Research Institute, Korea Institute of Science and Technology, Seoul 02792, Korea; [email protected] (T.H.L.); [email protected] (O.K.) 2 Center for Healthcare Robotics, AI and Robot Institute, Korea Institute of Science and Technology, Seoul 02792, Korea; [email protected] 3 Division of Bio-Medical Science and Technology, KIST School, Korea University of Science and Technology, Seoul 02792, Korea * Correspondence: [email protected]; Tel.: +82-2-958-5645 Featured Application: The findings and approach can potentially be used to guide surgical train- ing and planning for developing a minimal-incision surgical procedure by considering surgical position-dependent muscle material properties. Abstract: Although spinal surgeries with minimal incisions and a minimal amount of X-ray exposure (MIMA) mostly occur in a prone posture on a Wilson table, the prone posture’s effects on spinal muscles have not been investigated. Thus, this study used ultrasound shear-wave elastography (SWE) to compare the material properties of the erector spinae and multifidus muscles when subjects lay on the Wilson table used for spinal surgery and the flat table as a control condition. Thirteen male subjects participated in the study. Using ultrasound SWE, the shear elastic moduli (SEM) of the Citation: Lim, T.H.; Lee, D.; Kim, O.; Lee, S.J. Quantification of the Elastic erector spinae and multifidus muscles were investigated. -

Meat Quality Workshop: Know Your Muscle, Know Your Meat BEEF
2/6/2017 Meat Quality Workshop: Know Your Muscle, Know Your Meat Principles of Muscle Profiling, Aging, and Nutrition Dale R. Woerner, Ph.D., Colorado State University BEEF- Determining Value 1 2/6/2017 Slight00 Small00 Modest00 Moderate00 SLAB00 MAB00 ACE ABC Maturity Group Approximate Age A 9‐30 months B 30‐42 months C 42‐72 months D E 72‐96 months 96 months or older Augmentation of USDA Grade Application 2 2/6/2017 Effect of Marbling Degree on Probability of a Positive Sensory Experience Probability of a Positive Sensory Experience 0.99a 0.98a 1 0.88b 0.9 0.82b 0.8 0.7 0.62c 0.6 0.5 0.4 0.29d 0.3 0.2 0.15e 0.1 0 TR SL SM MT MD SA MA Colorado State University M.S. Thesis: M. R. Emerson (2011) 3 2/6/2017 Carcass Weight Trend 900 All Fed Cattle CAB® 875 850 +55 lbs. in 5 years 825 +11 lbs. / year 800 775 750 +117 lbs. in 20 years Hot Carcass (lbs.) Weight +5.8 lbs. / year 725 Year 4 2/6/2017 Further Problems • Food service portion cutting problems = 8 oz. • Steak preparation problems = 8 oz. A 1,300‐pound, Yield Grade 3 steer yields 639 pounds of retail cuts from an 806‐pound carcass. Of the retail cuts, 62% are roasts and steaks (396 pounds) and 38% are ground beef and stew meat (243 pounds). 5 2/6/2017 Objective of Innovative Fabrication • Use quality-based break points during fabrication • Add value to beef by optimizing use of high-quality cuts • Add value to beef cuts by improving leanness and portion size $2.25 $7.56 $2.75 $4.66 $2.50 $12.73 $2.31 $2.85 $3.57 $1.99 Aging Response Premium USDA Choice USDA Select Muscle Aging response -

Towards Defining Muscular Regions of Interest from Axial Magnetic Resonance Imaging with Anatomical Cross-Reference: Part II - Cervical Spine Musculature James M
Elliott et al. BMC Musculoskeletal Disorders (2018) 19:171 https://doi.org/10.1186/s12891-018-2074-y TECHNICAL ADVANCE Open Access Towards defining muscular regions of interest from axial magnetic resonance imaging with anatomical cross-reference: part II - cervical spine musculature James M. Elliott1,2,3* , Jon Cornwall4, Ewan Kennedy5, Rebecca Abbott2 and Rebecca J. Crawford6 Abstract Background: It has been suggested that the quantification of paravertebral muscle composition and morphology (e.g. size/shape/structure) with magnetic resonance imaging (MRI) has diagnostic, prognostic, and therapeutic potential in contributing to overall musculoskeletal health. If this is to be realised, then consensus towards standardised MRI methods for measuring muscular size/shape/structure are crucial to allow the translation of such measurements towards management of, and hopefully improved health for, those with some musculoskeletal conditions. Following on from an original paper detailing methods for measuring muscles traversing the lumbar spine, we propose new methods based on anatomical cross-reference that strive towards standardising MRI-based quantification of anterior and posterior cervical spine muscle composition. Methods: In this descriptive technical advance paper we expand our methods from the lumbar spine by providing a detailed examination of regional cervical spine muscle morphology, followed by a comprehensive description of the proposed technique defining muscle ROI from axial MRI. Cross-referencing cervical musculature and vertebral -

Effect of Latissimus Dorsi Muscle Strengthening in Mechanical Low Back Pain
International Journal of Science and Research (IJSR) ISSN: 2319-7064 ResearchGate Impact Factor (2018): 0.28 | SJIF (2019): 7.583 Effect of Latissimus Dorsi Muscle Strengthening in Mechanical Low Back Pain 1 2 Vishakha Vishwakarma , Dr. P. R. Suresh 1, 2PCPS & RC, People’s University, Bhopal (M.P.), India Abstract: Mechanical low back pain (MLBP) is one of the most common musculoskeletal pain syndromes, affecting up to 80% of people at some point during their lifetime. Sources of back pain are numerous, usually sought in as lesion of disc or facet joints at L4- L5 and L5-S1 levels. Studies have shown that 40% of all back pain is of thoracolumbar origin. The term meachnical low back pain also gives reassurance that there is no damage to the nerves or spinal pathology. The clinical presentation of mechanical low back pain usually the ages 18-55 years is in the lumbo sacral region. A study was conducted to evaluate the designed to check the effectiveness of Conventional Exercises alone in Mechanical low back pain and along with the latissimus dorsi muscle strengthening, data was collected from People’s hospital, Bhopal (age group-30-45 yr both male and female randomly) Keywords: Visual analog scale, Assessment chart, Treatment table, Data collection sheets, Essential stationery materials, Computer, SPSS Software etc. 1. Introduction Back pain is a primary to seek medical advice considering 80% of people suffering from back pain. Mechanical low back pain is defined as a result of minor intervertebral dysfunction and referred pain in the low back The latissimus dorsi is a large, flat muscle on the back that and hip region, and can often be confused with the other stretches to the sides, behind the arm, and is partly covered pathologies that may cause these symptoms.18 by the trapezius on the back near the midline, the word latissimus dorsi comes from Latin and its means, broadest muscle of the back dorsum means back. -
Muscles of Mastication Muscles That Move the Head
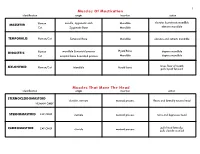
1 Muscles Of Mastication identification origin insertion action maxilla, zygomatic arch Mandible elevates & protracts mandible MASSETER Human Cat Zygomatic Bone Mandible elevates mandible TEMPORALIS Human/Cat Temporal Bone Mandible elevates and retracts mandible Hyoid Bone DIGASTRIC Human mandible & mastoid process depress mandible Cat occipital bone & mastoid process Mandible depress mandible raises floor of mouth; MYLOHYOID Human/Cat Mandible Hyoid bone pulls hyoid forward Muscles That Move The Head identification origin insertion action STERNOCLEIDOMAStoID clavicle, sternum mastoid process flexes and laterally rotates head HUMAN ONLY STERNOMAStoID CAT ONLY sternum mastoid process turns and depresses head pulls head laterally; CLEIDOMAStoID CAT ONLY clavicle mastoid process pulls clavicle craniad 2 Muscles Of The Hyoid, Larynx And Tongue identification origin insertion action Human Sternum Hyoid depresses hyoid bone STERNOHYOID Cat costal cartilage 1st rib Hyoid pulls hyoid caudally; raises ribs and sternum sternum Throid cartilage of larynx Human depresses thyroid cartilage STERNothYROID Cat costal cartilage 1st rib Throid cartilage of larynx pulls larynx caudad elevates thyroid cartilage and Human thyroid cartilage of larynx Hyoid THYROHYOID depresses hyoid bone Cat thyroid cartilage of larynx Hyoid raises larynx GENIOHYOID Human/Cat Mandible Hyoid pulls hyoid craniad 3 Muscles That Attach Pectoral Appendages To Vertebral Column identification origin insertion action Human Occipital bone; Thoracic and Cervical raises clavicle; adducts, -

Differences in Electromyographic Activity in the Multifidus Muscle And
Eur Spine J (2002) 11:13–19 DOI 10.1007/s005860100314 ORIGINAL ARTICLE L. A. Danneels Differences in electromyographic activity P. L. Coorevits A. M. Cools in the multifidus muscle G. G. Vanderstraeten D. C. Cambier and the iliocostalis lumborum E. E. Witvrouw H. J. De Cuyper between healthy subjects and patients with sub-acute and chronic low back pain Abstract The present study was differences between patients and Received: 2 February 2001 Revised: 12 May 2001 carried out to examine possible controls were found for the nor- Accepted: 28 May 2001 mechanisms of back muscle dysfunc- malised EMG activity of the two Published online: 14 July 2001 tion by assessing a stabilising and a muscles. These findings indicated © Springer-Verlag 2001 torque-producing back muscle, the that, during low-load exercises, no multifidus (MF) and the iliocostalis insufficiencies in back muscle re- lumborum pars thoracis (ICLT), re- cruitment were evident in either sub- spectively, in order to identify acute or chronic back pain patients. whether back pain patients showed During the strength exercises, the altered recruitment patterns during normalised activity of both back different types of exercise. In a muscles was significantly lower group of healthy subjects (n=77) and in chronic low back pain patients patients with sub-acute (n=24) and (P=0.017 and 0.003 for the MF and chronic (51) low back pain, the nor- ICLT, respectively) than in healthy malised electromyographic (EMG) controls. Pain, pain avoidance and activity of the MF and the ICLT (as deconditioning may have contributed a percentage of maximal voluntary to these lower levels of EMG activ- contraction) were analysed during ity during intensive back muscle coordination, stabilisation and contraction. -

Lumbar Muscle Function and Dysfunction in Low Back Pain - Markku Kankaanpää
PHYSIOLOGY AND MAINTENANCE – Vol. IV - Lumbar Muscle Function and Dysfunction in Low Back Pain - Markku Kankaanpää LUMBAR MUSCLE FUNCTION AND DYSFUNCTION IN LOW BACK PAIN Markku Kankaanpää Department of Physical Medicine and Rehabilitation, Kuopio University Hospital, and Department of Physiology, University of Kuopio, Finland Keywords: Low back pain, trunk muscles, muscle coordination, dysfunction, biomechanics, deconditioning syndrome. Contents 1. Anatomy and Function of the Trunk Extensor and Flexor Muscles 1.1. Functional Properties of Lumbar Spine 1.2. Anatomy of Lumbar and Abdominal Muscles 1.3. Control Properties of Lumbar and Abdominal Muscles 2. Epidemiological Aspects of LBP 2.1. Physical Risk Factors of LBP 3. Structural and Pathophysiological Aspects in LBP 4. Lumbar Muscle Dysfunction in LBP 4.1. Loss of Strength 4.2. Excessive Lumbar Muscle Fatigue 4.3. Loss of Co-ordination and Muscle Control 4.4. Active Rehabilitation and Back Extensor Muscle Functional Assessment Glossary Bibliography Biographical Sketch Summary Low back pain is one of the most common health problems. The reason for back pain is most often unknown. Some of the models that help in explaining the origin of low back pain are introduced. The lumbar structure and muscle functions and dysfunctions in relation to low back pain are reviewed. Complex central and peripheral elements control the biomechanics of the lumbar spine and ensure optimal spinal loading in normal everyday life situations.UNESCO Low back pain leads to acute – and EOLSS chronic changes in paraspinal muscles and their control mechanisms. Acute changes are observed as impaired reflexive functions of paraspinal muscles. Pain in spinal structures results from reflexive activities that protect the spine from excessiveSAMPLE and harmful loading. -

The Anatomy and Function of the Equine Thoracolumbar Longissimus Dorsi Muscle
Aus dem Veterinärwissenschaftlichen Department der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Lehrstuhl für Anatomie, Histologie und Embryologie Vorstand: Prof. Dr. Dr. Fred Sinowatz Arbeit angefertigt unter der Leitung von Dr. Renate Weller, PhD, MRCVS The Anatomy and Function of the equine thoracolumbar Longissimus dorsi muscle Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Vorgelegt von Christina Carla Annette von Scheven aus Düsseldorf München 2010 2 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Priv.-Doz. Dr. Johann Maierl Korreferentin: Priv.-Doz. Dr. Bettina Wollanke Tag der Promotion: 24. Juli 2010 3 Für meine Familie 4 Table of Contents I. Introduction................................................................................................................ 8 II. Literature review...................................................................................................... 10 II.1 Macroscopic anatomy ............................................................................................. 10 II.1.1 Comparative evolution of the body axis ............................................................ 10 II.1.2 Axis of the equine body ..................................................................................... 12 II.1.2.1 Vertebral column of the horse....................................................................