Quadratus Lumborum Blocks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Netter's Anatomy Flash Cards – Section 7 – List 4Th Edition
Netter's Anatomy Flash Cards – Section 7 – List 4th Edition https://www.memrise.com/course/1577594/ Section 7 Lower Limb (72 cards) Plate 7-1 Hip (Coxal) Bone: Lateral View 1.1 Posterior superior iliac spine 1.2 Posterior inferior iliac spine 1.3 Greater sciatic notch 1.4 Body of ilium 1.5 Body of ischium 1.6 Ischial tuberosity 1.7 Pubic tubercle 1.8 Acetabulum 1.9 Iliac crest Plate 7-2 Hip (Coxal) Bone: Medial View 2.1 Wing (ala) of ilium (iliac fossa) 2.2 Pecten pubis (pectineal line) 2.3 Ramus of ischium 2.4 Lesser sciatic notch 2.5 Ischial spine 2.6 Articular surface (for sacrum) 2.7 Iliac tuberosity Plate 7-3 Hip Joint: Lateral View 3.1 Lunate (articular) surface of acetabulum 3.2 Articular cartilage 3.3 Head of femur 3.4 Ligament of head of femur (cut) 3.5 Obturator membrane 3.6 Acetabular labrum (fibrocartilaginous) Plate 7-4 Hip Joint: Anterior and Posterior Views 4.1 Iliofemoral ligament (Y ligament of Bigelow) 4.2 Pubofemoral ligament 4.3 Iliofemoral ligament 4.4 Ischiofemoral ligament Plate 7-5 Femur 5.1 Greater trochanter 5.2 Shaft (body) 5.3 Lateral epicondyle 5.4 Lateral condyle 5.5 Medial condyle 5.6 Medial epicondyle 5.7 Adductor tubercle 5.8 Linea aspera (Medial lip; Lateral lip) 5.9 Lesser trochanter 5.10 Intertrochanteric crest 5.11 Neck 5.12 Head Plate 7-6 Tibia and Fibula 6.1 Lateral condyle 6.2 Apex, Head, and Neck of fibula 6.3 Fibula 6.4 Lateral malleolus 6.5 Medial malleolus 6.6 Tibia 6.7 Tibial tuberosity 6.8 Medial condyle 6.9 Superior articular surfaces (medial and lateral facets) 6.10 Malleolar fossa of lateral -
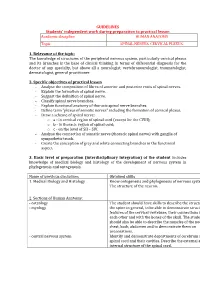
33. Spinal Nerves. Cervical Plexus
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Indications and Treatment of Myofascial Pain
2/25/2017 Indications and Treatment of Myofascial Pain Lisa DeStefano, DO Associate Professor and Chair Department of Osteopathic Manipulative Medicine College of Osteopathic Medicine Michigan State University Common Myofascial Pain Syndromes 1 2/25/2017 2 2/25/2017 Greater Occipital Nerve Impingement Sites . 1: Origin of the third occipital nerve and proximal connection with the greater occipital nerve. 2: Greater occipital nerve as it courses inferior to the inferior oblique muscle. 3: Greater occipital nerve coursing through the semispinalis capitis muscle. 4: Greater occipital nerve exiting the aponeurosis of the trapezius muscle. 5: Greater occipital nerve traveling with the occipital artery. 6: Origin of the greater occipital nerve and relationship to the descending branch of the occipital artery. 7: Suboccipital nerve relation to the vertebral artery and the descending branch of the occipital artery and this nerves interconnection to the greater occipital nerve. 8: Relationship between the third occipital nerve and the C2‐C3 joint complex. Common Treatment Approaches • MFR • MET • Soft Tissue Release • Counterstain • HVLA Etiology of Head and Neck Myofascial Pain Syndromes • Overuse • Posture –Head over the pelvis • Posture – Scapular function • Occlusion –how the teeth control for the proper placement of the mandibular condyle. 3 2/25/2017 Stabilization of the torsobegins with spinotransverse muscle transmission of force onto the epaxial fascia or vertebral aponeurosis. 4 2/25/2017 This then transmits tension into the serratus posterior superior and inferior, which then lifts the upper four ribs and sternum and lowers the lower ribs respectively. In response a force‐ couple is generated between the serratus posterior inferior fascia, external oblique fascia, and the rectus sheath. -

The Supra-Iliac Anterior Quadratus Lumborum Block
Can J Anesth/J Can Anesth https://doi.org/10.1007/s12630-019-01312-z REPORTS OF ORIGINAL INVESTIGATIONS The supra-iliac anterior quadratus lumborum block: a cadaveric study and case series Le bloc du muscle carre´ des lombes ante´rieur par approche supra-iliaque : une e´tude cadave´rique et une se´rie de cas Hesham Elsharkawy, MD, MBA, MSc . Kariem El-Boghdadly, MBBS, BSc, FRCA, EDRA, MSc . Theresa J. Barnes, MD, MPH . Richard Drake, PhD . Kamal Maheshwari, MD, MPH . Loran Mounir Soliman, MD . Jean-Louis Horn, MD . Ki Jinn Chin, MD, FRCPC Received: 9 July 2018 / Revised: 10 December 2018 / Accepted: 10 December 2018 Ó Canadian Anesthesiologists’ Society 2019 Abstract Methods Ultrasound-guided bilateral supra-iliac anterior Purpose The local anesthetic injectate spread with fascial QL blocks were performed with 30 mL of India ink dye in plane blocks and corresponding clinical outcomes may six fresh adult cadavers. Cadavers were subsequently vary depending on the site of injection. We developed and dissected to determine distribution of the dye. In five evaluated a supra-iliac approach to the anterior quadratus patients undergoing hip surgery, a unilateral supra-iliac lumborum (QL) block and hypothesized that this single anterior QL block with 25 mL ropivacaine 0.5% followed injection might successfully block the lumbar and sacral by a continuous catheter infusion was performed. Patients plexus in cadavers and provide analgesia for patients were clinically assessed daily for block efficacy. undergoing hip surgery. Results The cadaveric injections showed consistent dye involvement of the majority of the branches of the lumbar plexus, including the femoral nerve, lateral femoral cutaneous nerve, ilioinguinal nerve, and iliohypogastric Permission to use images was obtained from the Cleveland Clinic nerve. -

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

Review Article Ovariohysterectomy in the Bitch
Hindawi Publishing Corporation Obstetrics and Gynecology International Volume 2010, Article ID 542693, 7 pages doi:10.1155/2010/542693 Review Article Ovariohysterectomy in the Bitch Djemil Bencharif, Lamia Amirat, Annabelle Garand, and Daniel Tainturier Department of Reproductive Pathology, ONIRIS: Nantes-Atlantic National College of Veterinary Medicine, Food Science and Engineering, Site de la Chantrerie, B.P:40706, 44307 Nantes Cedex, France Correspondence should be addressed to Djemil Bencharif, [email protected] Received 31 October 2009; Accepted 7 January 2010 Academic Editor: Liselotte Mettler Copyright © 2010 Djemil Bencharif et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Ovariohysterectomy is a surgical procedure widely employed in practice by vets. It is indicated in cases of pyometra, uterine tumours, or other pathologies. This procedure should only be undertaken if the bitch is in a fit state to withstand general anaesthesia. However, the procedure is contradicated if the bitch presents a generalised condition with hypothermia, dehydration, and mydriasis. Ovariohysterectomy is generally performed via the linea alba. Per-vaginal hysterectomy can also be performed in the event of uterine prolapse, if the latter cannot be reduced or if has been traumatised to such an extent that it cannot be replaced safely. Specific and nonspecific complictions can occur as hemorrhage, adherences, urinary incontinence, return to oestrus including repeat surgery. After an ovariectomy, bitches tend to put on weight, it is therefore important to inform the owner and to reduce the daily ration by 10%. -

Review Article Ovariohysterectomy in the Bitch
Hindawi Publishing Corporation Obstetrics and Gynecology International Volume 2010, Article ID 542693, 7 pages doi:10.1155/2010/542693 Review Article Ovariohysterectomy in the Bitch Djemil Bencharif, Lamia Amirat, Annabelle Garand, and Daniel Tainturier Department of Reproductive Pathology, ONIRIS: Nantes-Atlantic National College of Veterinary Medicine, Food Science and Engineering, Site de la Chantrerie, B.P:40706, 44307 Nantes Cedex, France Correspondence should be addressed to Djemil Bencharif, [email protected] Received 31 October 2009; Accepted 7 January 2010 Academic Editor: Liselotte Mettler Copyright © 2010 Djemil Bencharif et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Ovariohysterectomy is a surgical procedure widely employed in practice by vets. It is indicated in cases of pyometra, uterine tumours, or other pathologies. This procedure should only be undertaken if the bitch is in a fit state to withstand general anaesthesia. However, the procedure is contradicated if the bitch presents a generalised condition with hypothermia, dehydration, and mydriasis. Ovariohysterectomy is generally performed via the linea alba. Per-vaginal hysterectomy can also be performed in the event of uterine prolapse, if the latter cannot be reduced or if has been traumatised to such an extent that it cannot be replaced safely. Specific and nonspecific complictions can occur as hemorrhage, adherences, urinary incontinence, return to oestrus including repeat surgery. After an ovariectomy, bitches tend to put on weight, it is therefore important to inform the owner and to reduce the daily ration by 10%. -

35. Lumbar Plexus. Sacral Plexus. Coccygeal Plexus
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic LUMBAR PLEXUS. SACRAL PLEXUS. COCCYGEAL PLEXUS 1. Relevance of the topic Lumbar, sacral and coccygeal plexuses innervate the skin of the abdomen, lower back and lower extremities and all the muscles of the lower limbs. Acquired knowledge is the basis for many fields of practical medicine, such as neurology, surgery and traumatology. 2. Specific objectives After the lesson the student should know and be able to: - describe the sources of the formation of the lumbar plexus; - classify the nerves of the lumbar plexus; - to be able to demonstrate and define the branches of the lumbar plexus; - describe sources of sacral plexus formation; - classify sacral plexus nerves; - be able to demonstrate and identify short and long branches of the sacral plexus; - describe the sources of formation coccygeal plexus; - classify coccygeal plexus nerves; - be able to demonstrate and identify branches of coccygeal plexus; - to explain the innervation of muscles and skin in the areas of the lower back and lower extremity. 3. Basic level of preparation For practical this lesson a student should know and be able: - to know the anatomy of the spine, pelvis, lower extremities; - to analyze and show large and small pelvis, their bones; - to analyze and demonstrate bones and joints of the lower limbs; - to demonstrate muscles of the abdomen, perineum, pelvic girdle and lower limbs; - to know the anatomy (external and internal structure) of the spinal cord; - to know the spinal nerve anatomy. 4. Tasks for independent work during preparation for the classes 4.1. -

Anatomy of Abdominal Incisions
ANATOMY FOR THE MRCS but is time-consuming. A lower midline incision is needed for an Anatomy of abdominal emergency Caesarean section (where minutes may be crucial for baby and mother). The surgeon must also be sure of the pathol- incisions ogy before performing this approach. Close the Pfannenstiel and start again with a lower midline if the ‘pelvic mass’ proves to be Harold Ellis a carcinoma of the sigmoid colon! There are more than one dozen abdominal incisions quoted in surgical textbooks, but the ones in common use today (and which the candidate must know in detail) are discussed below. The midline incision (Figures 1–4) Opening the abdomen is the essential preliminary to the per- formance of a laparotomy. A correctly performed abdominal The midline abdominal incision has many advantages because it: exposure is based on sound anatomical knowledge, hence it is a • is very quick to perform common question in the Operative Surgery section of the MRCS • is relatively easy to close examination. • is virtually bloodless (no muscles are cut or nerves divided). • affords excellent access to the abdominal cavity and retroperi- toneal structures Incisions • can be extended from the xiphoid to the pubic symphysis. Essential features If closure is performed using the mass closure technique, pros- The surgeon needs ready and direct access to the organ requir- pective randomized clinical trials have shown no difference in ing investigation and treatment, so the incision must provide the incidence of wound dehiscence or incisional hernia com- sufficient room for the procedure to be performed. The incision pared with transverse or paramedian incisions.1 should (if possible): The upper midline incision is placed exactly in the midline • be capable of easy extension (to allow for any enlargement of and extends from the tip of the xiphoid to about 1 cm above the scope of the operation) the umbilicus. -

Divarication of Rectus Abdominis Muscle Postpartum Information And
Divarication of rectus abdominis muscle éçëíé~êíìã Information and advice What is divarication and why do I have it? For some women, pregnancy can cause separation of the stomach muscles which can also be referred to as Diastasis Recti. The right and left sides of the rectus abdominis muscle (‘six pack muscle’) separate at the linea alba which connects the two sides of the muscle together. Rectus Abdominis Abdominal Separation (approximate representation) (approximate representation) It is normal in pregnancy for the stomach muscles to separate as the uterus continues to grow and push on the abdominal wall. This only becomes problematic in pregnancy when the abdominal wall is weak. The abdominal muscles are an important muscle group in supporting your back. If they remain weak after pregnancy, it can increase your risk of suffering from back pain. Diagnosis – how do I know if I have a separation? Most pregnant women will have a separation of one or two fingers width after pregnancy and this is normal. In most cases this will spontaneously recover and will not cause you any problems. However if the gap is more than two fingers width and you have a visible doming at the midline, you may have a divarication of the abdominis muscle and would benefit from seeing a physiotherapist. You can measure this yourself by lying with your knees bent and using your fingers as a guide at the level of your belly button. What can I do to help myself? Try to avoid all activities which place a lot of pressure on your abdominal wall, or cause an over stretch to your stomach. -

Effect of Latissimus Dorsi Muscle Strengthening in Mechanical Low Back Pain
International Journal of Science and Research (IJSR) ISSN: 2319-7064 ResearchGate Impact Factor (2018): 0.28 | SJIF (2019): 7.583 Effect of Latissimus Dorsi Muscle Strengthening in Mechanical Low Back Pain 1 2 Vishakha Vishwakarma , Dr. P. R. Suresh 1, 2PCPS & RC, People’s University, Bhopal (M.P.), India Abstract: Mechanical low back pain (MLBP) is one of the most common musculoskeletal pain syndromes, affecting up to 80% of people at some point during their lifetime. Sources of back pain are numerous, usually sought in as lesion of disc or facet joints at L4- L5 and L5-S1 levels. Studies have shown that 40% of all back pain is of thoracolumbar origin. The term meachnical low back pain also gives reassurance that there is no damage to the nerves or spinal pathology. The clinical presentation of mechanical low back pain usually the ages 18-55 years is in the lumbo sacral region. A study was conducted to evaluate the designed to check the effectiveness of Conventional Exercises alone in Mechanical low back pain and along with the latissimus dorsi muscle strengthening, data was collected from People’s hospital, Bhopal (age group-30-45 yr both male and female randomly) Keywords: Visual analog scale, Assessment chart, Treatment table, Data collection sheets, Essential stationery materials, Computer, SPSS Software etc. 1. Introduction Back pain is a primary to seek medical advice considering 80% of people suffering from back pain. Mechanical low back pain is defined as a result of minor intervertebral dysfunction and referred pain in the low back The latissimus dorsi is a large, flat muscle on the back that and hip region, and can often be confused with the other stretches to the sides, behind the arm, and is partly covered pathologies that may cause these symptoms.18 by the trapezius on the back near the midline, the word latissimus dorsi comes from Latin and its means, broadest muscle of the back dorsum means back. -

Lumbar Muscle Function and Dysfunction in Low Back Pain - Markku Kankaanpää
PHYSIOLOGY AND MAINTENANCE – Vol. IV - Lumbar Muscle Function and Dysfunction in Low Back Pain - Markku Kankaanpää LUMBAR MUSCLE FUNCTION AND DYSFUNCTION IN LOW BACK PAIN Markku Kankaanpää Department of Physical Medicine and Rehabilitation, Kuopio University Hospital, and Department of Physiology, University of Kuopio, Finland Keywords: Low back pain, trunk muscles, muscle coordination, dysfunction, biomechanics, deconditioning syndrome. Contents 1. Anatomy and Function of the Trunk Extensor and Flexor Muscles 1.1. Functional Properties of Lumbar Spine 1.2. Anatomy of Lumbar and Abdominal Muscles 1.3. Control Properties of Lumbar and Abdominal Muscles 2. Epidemiological Aspects of LBP 2.1. Physical Risk Factors of LBP 3. Structural and Pathophysiological Aspects in LBP 4. Lumbar Muscle Dysfunction in LBP 4.1. Loss of Strength 4.2. Excessive Lumbar Muscle Fatigue 4.3. Loss of Co-ordination and Muscle Control 4.4. Active Rehabilitation and Back Extensor Muscle Functional Assessment Glossary Bibliography Biographical Sketch Summary Low back pain is one of the most common health problems. The reason for back pain is most often unknown. Some of the models that help in explaining the origin of low back pain are introduced. The lumbar structure and muscle functions and dysfunctions in relation to low back pain are reviewed. Complex central and peripheral elements control the biomechanics of the lumbar spine and ensure optimal spinal loading in normal everyday life situations.UNESCO Low back pain leads to acute – and EOLSS chronic changes in paraspinal muscles and their control mechanisms. Acute changes are observed as impaired reflexive functions of paraspinal muscles. Pain in spinal structures results from reflexive activities that protect the spine from excessiveSAMPLE and harmful loading.