35. Lumbar Plexus. Sacral Plexus. Coccygeal Plexus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -

4-Brachial Plexus and Lumbosacral Plexus (Edited).Pdf
Color Code Brachial Plexus and Lumbosacral Important Doctors Notes Plexus Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of this lecture, the students should be able to : Describe the formation of brachial plexus (site, roots) List the main branches of brachial plexus Describe the formation of lumbosacral plexus (site, roots) List the main branches of lumbosacral plexus Describe the important Applied Anatomy related to the brachial & lumbosacral plexuses. Brachial Plexus Formation Playlist o It is formed in the posterior triangle of the neck. o It is the union of the anterior rami (or ventral) of the 5th ,6th ,7th ,8th cervical and the 1st thoracic spinal nerves. o The plexus is divided into 5 stages: • Roots • Trunks • Divisions • Cords • Terminal branches Really Tired? Drink Coffee! Brachial Plexus A P A P P A Brachial Plexus Trunks Divisions Cords o Upper (superior) trunk o o Union of the roots of Each trunk divides into Posterior cord: C5 & C6 anterior and posterior From the 3 posterior division divisions of the 3 trunks o o Middle trunk Lateral cord: From the anterior Continuation of the divisions of the upper root of C7 Branches and middle trunks o All three cords will give o Medial cord: o Lower (inferior) trunk branches in the axilla, It is the continuation of Union of the roots of the anterior division of C8 & T1 those will supply their respective regions. the lower trunk The Brachial Plexus Long Thoracic (C5,6,7) Anterior divisions Nerve to Subclavius(C5,6) Posterior divisions Dorsal Scapular(C5) Suprascapular(C5,6) upper C5 trunk Lateral Cord C6 middle (2LM) trunk C7 lower C8 trunk T1 Posterior Cord (ULTRA) Medial Cord (4MU) In the PowerPoint presentation this slide is animated. -

Netter's Anatomy Flash Cards – Section 7 – List 4Th Edition
Netter's Anatomy Flash Cards – Section 7 – List 4th Edition https://www.memrise.com/course/1577594/ Section 7 Lower Limb (72 cards) Plate 7-1 Hip (Coxal) Bone: Lateral View 1.1 Posterior superior iliac spine 1.2 Posterior inferior iliac spine 1.3 Greater sciatic notch 1.4 Body of ilium 1.5 Body of ischium 1.6 Ischial tuberosity 1.7 Pubic tubercle 1.8 Acetabulum 1.9 Iliac crest Plate 7-2 Hip (Coxal) Bone: Medial View 2.1 Wing (ala) of ilium (iliac fossa) 2.2 Pecten pubis (pectineal line) 2.3 Ramus of ischium 2.4 Lesser sciatic notch 2.5 Ischial spine 2.6 Articular surface (for sacrum) 2.7 Iliac tuberosity Plate 7-3 Hip Joint: Lateral View 3.1 Lunate (articular) surface of acetabulum 3.2 Articular cartilage 3.3 Head of femur 3.4 Ligament of head of femur (cut) 3.5 Obturator membrane 3.6 Acetabular labrum (fibrocartilaginous) Plate 7-4 Hip Joint: Anterior and Posterior Views 4.1 Iliofemoral ligament (Y ligament of Bigelow) 4.2 Pubofemoral ligament 4.3 Iliofemoral ligament 4.4 Ischiofemoral ligament Plate 7-5 Femur 5.1 Greater trochanter 5.2 Shaft (body) 5.3 Lateral epicondyle 5.4 Lateral condyle 5.5 Medial condyle 5.6 Medial epicondyle 5.7 Adductor tubercle 5.8 Linea aspera (Medial lip; Lateral lip) 5.9 Lesser trochanter 5.10 Intertrochanteric crest 5.11 Neck 5.12 Head Plate 7-6 Tibia and Fibula 6.1 Lateral condyle 6.2 Apex, Head, and Neck of fibula 6.3 Fibula 6.4 Lateral malleolus 6.5 Medial malleolus 6.6 Tibia 6.7 Tibial tuberosity 6.8 Medial condyle 6.9 Superior articular surfaces (medial and lateral facets) 6.10 Malleolar fossa of lateral -
33. Spinal Nerves. Cervical Plexus
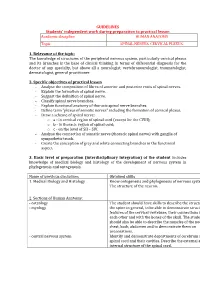
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

LECTURE (SACRAL PLEXUS, SCIATIC NERVE and FEMORAL NERVE) Done By: Manar Al-Eid Reviewed By: Abdullah Alanazi
CNS-432 LECTURE (SACRAL PLEXUS, SCIATIC NERVE AND FEMORAL NERVE) Done by: Manar Al-Eid Reviewed by: Abdullah Alanazi If there is any mistake please feel free to contact us: [email protected] Both - Black Male Notes - BLUE Female Notes - GREEN Explanation and additional notes - ORANGE Very Important note - Red CNS-432 Objectives: By the end of the lecture, students should be able to: . Describe the formation of sacral plexus (site & root value). List the main branches of sacral plexus. Describe the course of the femoral & the sciatic nerves . List the motor and sensory distribution of femoral & sciatic nerves. Describe the effects of lesion of the femoral & the sciatic nerves (motor & sensory). CNS-432 The Mind Maps Lumber Plexus 1 Branches Iliohypogastric - obturator ilioinguinal Femoral Cutaneous branches Muscular branches to abdomen and lower limb 2 Sacral Plexus Branches Pudendal nerve. Pelvic Splanchnic Sciatic nerve (largest nerves nerve), divides into: Tibial and divides Fibular and divides into : into: Medial and lateral Deep peroneal Superficial planter nerves . peroneal CNS-432 Remember !! gastrocnemius Planter flexion – knee flexion. soleus Planter flexion Iliacus –sartorius- pectineus – Hip flexion psoas major Quadriceps femoris Knee extension Hamstring muscles Knee flexion and hip extension gracilis Hip flexion and aids in knee flexion *popliteal fossa structures (superficial to deep): 1-tibial nerve 2-popliteal vein 3-popliteal artery. *foot drop : planter flexed position Common peroneal nerve injury leads to Equinovarus Tibial nerve injury leads to Calcaneovalgus CNS-432 Lumbar Plexus Formation Ventral (anterior) rami of the upper 4 lumbar spinal nerves (L1,2,3 and L4). Site Within the substance of the psoas major muscle. -

The Supra-Iliac Anterior Quadratus Lumborum Block
Can J Anesth/J Can Anesth https://doi.org/10.1007/s12630-019-01312-z REPORTS OF ORIGINAL INVESTIGATIONS The supra-iliac anterior quadratus lumborum block: a cadaveric study and case series Le bloc du muscle carre´ des lombes ante´rieur par approche supra-iliaque : une e´tude cadave´rique et une se´rie de cas Hesham Elsharkawy, MD, MBA, MSc . Kariem El-Boghdadly, MBBS, BSc, FRCA, EDRA, MSc . Theresa J. Barnes, MD, MPH . Richard Drake, PhD . Kamal Maheshwari, MD, MPH . Loran Mounir Soliman, MD . Jean-Louis Horn, MD . Ki Jinn Chin, MD, FRCPC Received: 9 July 2018 / Revised: 10 December 2018 / Accepted: 10 December 2018 Ó Canadian Anesthesiologists’ Society 2019 Abstract Methods Ultrasound-guided bilateral supra-iliac anterior Purpose The local anesthetic injectate spread with fascial QL blocks were performed with 30 mL of India ink dye in plane blocks and corresponding clinical outcomes may six fresh adult cadavers. Cadavers were subsequently vary depending on the site of injection. We developed and dissected to determine distribution of the dye. In five evaluated a supra-iliac approach to the anterior quadratus patients undergoing hip surgery, a unilateral supra-iliac lumborum (QL) block and hypothesized that this single anterior QL block with 25 mL ropivacaine 0.5% followed injection might successfully block the lumbar and sacral by a continuous catheter infusion was performed. Patients plexus in cadavers and provide analgesia for patients were clinically assessed daily for block efficacy. undergoing hip surgery. Results The cadaveric injections showed consistent dye involvement of the majority of the branches of the lumbar plexus, including the femoral nerve, lateral femoral cutaneous nerve, ilioinguinal nerve, and iliohypogastric Permission to use images was obtained from the Cleveland Clinic nerve. -

Spinal Nerves, Ganglia, and Nerve Plexus Spinal Nerves
Chapter 13 Spinal Nerves, Ganglia, and Nerve Plexus Spinal Nerves Posterior Spinous process of vertebra Posterior root Deep muscles of back Posterior ramus Spinal cord Transverse process of vertebra Posterior root ganglion Spinal nerve Anterior ramus Meningeal branch Communicating rami Anterior root Vertebral body Sympathetic ganglion Anterior General Anatomy of Nerves and Ganglia • Spinal cord communicates with the rest of the body by way of spinal nerves • nerve = a cordlike organ composed of numerous nerve fibers (axons) bound together by connective tissue – mixed nerves contain both afferent (sensory) and efferent (motor) fibers – composed of thousands of fibers carrying currents in opposite directions Anatomy of a Nerve Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Epineurium Perineurium Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Endoneurium Nerve Rootlets fiber Posterior root Fascicle Posterior root ganglion Anterior Blood root vessels Spinal nerve (b) Copyright by R.G. Kessel and R.H. Kardon, Tissues and Organs: A Text-Atlas of Scanning Electron Microscopy, 1979, W.H. Freeman, All rights reserved Blood vessels Fascicle Epineurium Perineurium Unmyelinated nerve fibers Myelinated nerve fibers (a) Endoneurium Myelin General Anatomy of Nerves and Ganglia • nerves of peripheral nervous system are ensheathed in Schwann cells – forms neurilemma and often a myelin sheath around the axon – external to neurilemma, each fiber is surrounded by -

Study of Anatomical Pattern of Lumbar Plexus in Human (Cadaveric Study)
54 Az. J. Pharm Sci. Vol. 54, September, 2016. STUDY OF ANATOMICAL PATTERN OF LUMBAR PLEXUS IN HUMAN (CADAVERIC STUDY) BY Prof. Gamal S Desouki, prof. Maged S Alansary,dr Ahmed K Elbana and Mohammad H Mandor FROM Professor Anatomy and Embryology Faculty of Medicine - Al-Azhar University professor of anesthesia Faculty of Medicine - Al-Azhar University Anatomy and Embryology Faculty of Medicine - Al-Azhar University Department of Anatomy and Embryology Faculty of Medicine of Al-Azhar University, Cairo Abstract The lumbar plexus is situated within the substance of the posterior part of psoas major muscle. It is formed by the ventral rami of the frist three nerves and greater part of the fourth lumbar nerve with or without a contribution from the ventral ramus of last thoracic nerve. The pattern of formation of lumbar plexus is altered if the plexus is prefixed (if the third lumbar is the lowest nerve which enters the lumbar plexus) or postfixed (if there is contribution from the 5th lumbar nerve). The branches of the lumbar plexus may be injured during lumbar plexus block and certain surgical procedures, particularly in the lower abdominal region (appendectomy, inguinal hernia repair, iliac crest bone graft harvesting and gynecologic procedures through transverse incisions). Thus, a better knowledge of the regional anatomy and its variations is essential for preventing the lesions of the branches of the lumbar plexus. Key Words: Anatomical variations, Lumbar plexus. Introduction The lumbar plexus formed by the ventral rami of the upper three nerves and most of the fourth lumbar nerve with or without a contribution from the ventral ramous of last thoracic nerve. -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

New Insights in Lumbosacral Plexopathy
New Insights in Lumbosacral Plexopathy Kerry H. Levin, MD Gérard Said, MD, FRCP P. James B. Dyck, MD Suraj A. Muley, MD Kurt A. Jaeckle, MD 2006 COURSE C AANEM 53rd Annual Meeting Washington, DC Copyright © October 2006 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 PRINTED BY JOHNSON PRINTING COMPANY, INC. C-ii New Insights in Lumbosacral Plexopathy Faculty Kerry H. Levin, MD P. James. B. Dyck, MD Vice-Chairman Associate Professor Department of Neurology Department of Neurology Head Mayo Clinic Section of Neuromuscular Disease/Electromyography Rochester, Minnesota Cleveland Clinic Dr. Dyck received his medical degree from the University of Minnesota Cleveland, Ohio School of Medicine, performed an internship at Virginia Mason Hospital Dr. Levin received his bachelor of arts degree and his medical degree from in Seattle, Washington, and a residency at Barnes Hospital and Washington Johns Hopkins University in Baltimore, Maryland. He then performed University in Saint Louis, Missouri. He then performed fellowships at a residency in internal medicine at the University of Chicago Hospitals, the Mayo Clinic in peripheral nerve and electromyography. He is cur- where he later became the chief resident in neurology. He is currently Vice- rently Associate Professor of Neurology at the Mayo Clinic. Dr. Dyck is chairman of the Department of Neurology and Head of the Section of a member of several professional societies, including the AANEM, the Neuromuscular Disease/Electromyography at Cleveland Clinic. Dr. Levin American Academy of Neurology, the Peripheral Nerve Society, and the is also a professor of medicine at the Cleveland Clinic College of Medicine American Neurological Association. -

A Step Towards Stereotactic Navigation During Pelvic Surgery: 3D Nerve Topography
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Surgical Endoscopy and Other Interventional Techniques https://doi.org/10.1007/s00464-018-6086-3 A step towards stereotactic navigation during pelvic surgery: 3D nerve topography A. R. Wijsmuller1,2 · C. Giraudeau3 · J. Leroy4 · G. J. Kleinrensink5 · E. Rociu6 · L. G. Romagnolo7 · A. G. F. Melani7,8,9 · V. Agnus2 · M. Diana3 · L. Soler3 · B. Dallemagne2 · J. Marescaux2 · D. Mutter2 Received: 10 May 2017 / Accepted: 1 February 2018 © The Author(s) 2018. This article is an open access publication Abstract Background Long-term morbidity after multimodal treatment for rectal cancer is suggested to be mainly made up by nerve- injury-related dysfunctions. Stereotactic navigation for rectal surgery was shown to be feasible and will be facilitated by highlighting structures at risk of iatrogenic damage. The aim of this study was to investigate the ability to make a 3D map of the pelvic nerves with magnetic resonance imaging (MRI). Methods A systematic review was performed to identify a main positional reference for each pelvic nerve and plexus. The nerves were manually delineated in 20 volunteers who were scanned with a 3-T MRI. The nerve identifiability rate and the likelihood of nerve identification correctness were determined. Results The analysis included 61 studies on pelvic nerve anatomy. A main positional reference was defined for each nerve. On MRI, the sacral nerves, the lumbosacral plexus, and the obturator nerve could be identified bilaterally in all volunteers. The sympathetic trunk could be identified in 19 of 20 volunteers bilaterally (95%).