Diagnosis of Coma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Forensic Medicine
YEREVAN STATE MEDICAL UNIVERSITY AFTER M. HERATSI DEPARTMENT OF Sh. Vardanyan K. Avagyan S. Hakobyan FORENSIC MEDICINE Handout for foreign students YEREVAN 2007 This handbook is adopted by the Methodical Council of Foreign Students of the University DEATH AND ITS CAUSES Thanatology deals with death in all its aspects. Death is of two types: (1) somatic, systemic or clinical, and (2) molecular or cellular. Somatic Death: It is the complete and irreversible stoppage of the circulation, respiration and brain functions, but there is no legal definition of death. THE MOMENT OF DEATH: Historically (medically and legally), the concept of death was that of "heart and respiration death", i.e. stoppage of spontaneous heart and breathing functions. Heart-lung bypass machines, mechanical respirators, and other devices, however have changed this medically in favor of a new concept "brain death", that is, irreversible loss of Cerebral function. Brain death is of three types: (1) Cortical or cerebral death with an intact brain stem. This produces a vegetative state in which respiration continues, but there is total loss of power of perception by the senses. This state of deep coma can be produced by cerebral hypoxia, toxic conditions or widespread brain injury. (2) Brain stem death, where the cerebrum may be intact, though cut off functionally by the stem lesion. The loss of the vital centers that control respiration, and of the ascending reticular activating system that sustains consciousness, cause the victim to be irreversibly comatose and incapable of spontaneous breathing. This can be produced by raised intracranial pressure, cerebral oedema, intracranial haemorrhage, etc.(3) Whole brain death (combination of 1 and 2). -

Coma Stimulation: Suggested Activities
Coma stimulation: suggested activities Headway’s publications are all available to freely download from the information library on the charity’s website, while individuals and families can request hard copies of the booklets via the helpline. As a charity, we rely on donations from people like you to continue providing free information to people affected by brain injury. Donate today: www.headway.org.uk/donate. Introduction It is quite common for family members to feel ‘useless’ when a relative is in a coma, and to be desperate to do something to help. A coma stimulation programme (sometimes called a coma arousal programme) is an approach based on stimulating the unconscious person’s senses of hearing, touch, smell, taste and vision individually in order to help their recovery. There is still controversy over how effective it is to try to stimulate a person in coma. However, most would say that such programmes have some beneficial effect, even if only to provide something constructive for the family to do. It is very important that the activities used would have been enjoyable for the patient before the injury. For example, only play music they like and talk to them about subjects they are interested in. Try not to do anything for too long in order to avoid tiring the person out. A stimulation programme must only be started after discussion with the clinical staff, who will advise you what might be appropriate at any particular stage in the recovery process. Activity suggestions Here are some examples of activities that could form part of a coma stimulation programme: • Make sure that a few friends and family members visit regularly, rather than in large groups at a time. -

Evaluation and Management in an Urgent Care Setting
Syncope Evaluation and Management in an Urgent Care Setting Urgent message: When a patient presents to urgent care after a syncopal event, the clinician’s charge is to determine whether the episode was of benign or potentially life-threatening etiology and whether the patient should be transferred for further evaluation. Kenneth V. Iserson, MD, MBA, FACEP, FAAEM, Professor of Emergency Medicine, The University of Arizona, Tucson, AZ Introduction yncope is a sudden, transient loss of consciousness with a loss of postural tone (typically, falling). It results from an abrupt, transient, and diffuse cerebral Smalfunction and is quickly followed by sponta- neous recovery. The term syncope excludes seizures, coma, shock, or other states of altered consciousness. Many patients will ascribe their syncopal episode to a sit- uationally mediated vasovagal episode. Despite this, the goals in the urgent care setting include the following: Ⅲ Determining whether the patient’s episode was actually a syncopal or presyncopal event, and if it could have a life-threatening etiology Ⅲ Stabilizing the patient Ⅲ Transferring those patients who need further diag- nostic studies or therapeutic interventions © John Bolesky, Artville © John Bolesky, Epidemiology Syncope accounts for up to 3% of emergency depart- common in young adults, while cardiac syncope ment (ED) visits and up to 6% of hospital admissions becomes increasingly more frequent with advancing each year in the United States.1,2 At some time in their age.4 The chance of having at least one syncopal episode lives, up to about half the population (12% to 48%) of in childhood is between 15% and 50%.5 Though a people may experience syncope.3 benign cause is usually found, syncope in children war- Syncope occurs in all age groups, but it is most com- rants prompt detailed evaluation.6 mon in adults. -
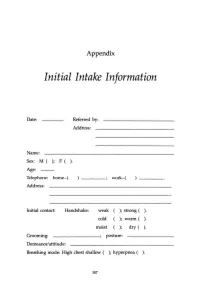
Initial Intake Information
Appendix Initial Intake Information Date: Referred by: Address: Name: Sex: M ( ); F ( ). Age: Telephone: home-( work-( Address: Initial contact: Handshake: weak ); strong ( ). cold ); warm ( ). moist ); dry ( ). Grooming: ________; posture: Demeanor/attitude: Breathing mode: High chest shallow ( ); hyperpnea ( ). 307 308 APPENDIX Sighing: frequent ( ); occasional ( ); absent ( ). Occupation: Contact with: dust ( ); fibers (); paints ( ); solvents ( ); sprays ( ); detergents ( ). Other chemicals or airborne particles: Status: Married ( ); single ( ); divorced ( ); other: children: No. Boys ( ); No. Girls ( ). Physician(s) of record: Last medical examination: _________,199__ Diagnos(e)s: 'Ireatmentts): Medication(s): Do you now have, have you ever had, or has any family member related to you by blood (mother, father, sister, brother, familial grandparents or uncles and aunts) had: ( ) High blood pressure () Heart disease APPENDIX 309 ) Low blood pressure ) Angina ) Diabetes (insulin-dependent) ) Anemia ) Diabetes (non-insulin- ) Allergies dependent) ) Dermatitis ) Colitis ) Muscle spasms ) Gastritis ) Tingling in hands and/or feet ) Ulcer ) Fainting (syncope) ) Shortness of breath ) Dizziness (vertigo) ) Asthma ) Stroke ) Emphysema ) Headache ) Hyperventilation ) TMJlbruxism ) Mitral valve prolapse ) Chronic low backache ) Other heart murmur ) EB virus (mononucl.) ) Heart arrhythmia ) PMS ) Chronic vaginal yeast ) Chronic tiredness ) Cystitis ) Menstrual irregul. ) Raynaud's disease ) Tinnitus ) Chronic pain ) Hyperthyroid ) Eating disorder -

The Vegetative State: Guidance on Diagnosis and Management
n CLINICAL GUIDANCE The vegetative state: guidance on diagnosis and management A report of a working party of the Royal College of Physicians contrasts with sleep, a state of eye closure and motor Clin Med 1INTRODUCTION quiescence. There are degrees of wakefulness. 2003;3:249–54 Wakefulness is normally associated with conscious awareness, but the VS indicates that wakefulness and Background awareness can be dissociated. This can occur because 1.1 This guidance has been compiled to replace the brain systems controlling wakefulness, in the the recommendations published by the Royal College upper brainstem and thalamus, are largely distinct of Physicians in 1996, 1 in response to requests for from those which mediate awareness. 6 clarification from the Official Solicitor. The guidance applies primarily to adult patients and older children Awareness in whom it is possible to apply the criteria for diagnosis discussed below. 1.6 Awareness refers to the ability to have, and the having of, experience of any kind. We are typically aware of our surroundings and of bodily sensations, Wakefulness without awareness but the contents of awareness can also include our 1.2 Consciousness is an ambiguous term, encom- memories, thoughts, emotions and intentions. passing both wakefulness and awareness. This dis- Although understanding of the brain mechanisms of tinction is crucial to the concept of the vegetative awareness is incomplete, structures in the cerebral state, in which wakefulness recovers after brain hemispheres clearly play a key role. Awareness is not injury without recovery of awareness. 2–5 a single indivisible capacity: brain damage can selectively impair some aspects of awareness, leaving others intact. -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department -

Factors Predicting Acute Brain Injury in Cases of Carbon Monoxide Poisoning: a Prospective Registry-Based Study
toxics Article Factors Predicting Acute Brain Injury in Cases of Carbon Monoxide Poisoning: A Prospective Registry-Based Study Hoon Lim 1,†, Young Hwan Lee 1,†, Sangun Nah 1 , Sungwoo Choi 1 , Young Soon Cho 1, Gi Woon Kim 1, Ji Eun Moon 2 and Sangsoo Han 1,* 1 Department of Emergency Medicine, Soonchunhyang University Bucheon Hospital, Bucheon 14584, Korea; [email protected] (H.L.); [email protected] (Y.H.L.); [email protected] (S.N.); [email protected] (S.C.); [email protected] (Y.S.C.); [email protected] (G.W.K.) 2 Department of Biostatistics, Clinical Trial Center, Soonchunhyang University Bucheon Hospital, Bucheon 14584, Korea; [email protected] * Correspondence: [email protected] † Hoon Lim and Young Hwan Lee contributed equally to this work. Abstract: Carbon monoxide (CO) is one of the most common poisoning substances worldwide. Since acute brain injury (ABI) is an important determinant of the neurological outcome in CO poisoning, screening for patients at a high risk of developing ABI is essential for the proper treatment. This study identified predictors of ABI in patients with CO poisoning. This prospective registry-based study was conducted in patients who visited a tertiary care hospital for CO poisoning from August 2016 to June 2020. ABI was defined as the presence of acute hypoxic lesions on diffusion-weighted magnetic resonance imaging. Multiple logistic regression analysis was performed to identify the predictors of ABI. Of 231 patients, 64 (27.7%) showed ABI. Multiple logistic regression analysis showed that a Citation: Lim, H.; Lee, Y.H.; Nah, S.; Glasgow Coma Scale (GCS) score <9 at presentation (odds ratio [OR] 3.28, 95% confidence interval Choi, S.; Cho, Y.S.; Kim, G.W.; Moon, (CI) 1.08–10.01), creatinine level >1.2 mg/dL (OR 3.04, 95% CI 1.16–8.01), and C-reactive protein J.E.; Han, S. -

EMS Quick Study Guide NOTICE: You DO NOT Have the Right to Reprint Or Resell This Publication
Presents The EMS Quick Study Guide NOTICE: You DO NOT Have the Right to Reprint or Resell this Publication. You Also MAY NOT Give Away, Sell or Share the Content Herein. If you purchased this book/ebook from anywhere other than http://www.ems-safety.com , you have a pirated copy. Please help stop Internet crime by reporting this to: [email protected] © Copyright The EMS Professional ALL RIGHTS RESERVED. No part of this publication may be reproduced or transmitted in any form whatsoever, electronic, or mechanical, including photocopying, recording, or by any informational storage or retrieval system without the expressed written, dated and signed permission from the author. DISCLAIMER AND/OR LEGAL NOTICES: The information presented herein represents the views of the author as of the date of publication. Because of the rate with which conditions change, the author reserves the right to alter and update this information based on the new conditions. The publication is for informational purposes only. While every attempt has been made to verify the information provided in this publication, neither the author nor its affiliates/partners assume any responsibility for errors, inaccuracies or omissions. Any slights of people or organizations are unintentional. If advice concerning medical, legal or related matters is needed, the services of a fully qualified professional should be sought. You should be aware of any laws/practices or local policies which govern emergency care or other pre hospital care practices in your country and state. -

Pdfs/Brainstemdeath.Pdf Disturbances Must Be Excluded As the Cause of Continuation of 12 Wijdicks EF
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.suppl_3.iii16 on 21 August 2003. Downloaded from NEUROLOGICAL CONSULTATIONS IN THE MEDICAL INTENSIVE CARE UNIT Saif S M Razvi, Ian Bone iii16* J Neurol Neurosurg Psychiatry 2003;74(Suppl III):iii16–iii23 ritical care therapy has advanced over the past two decades, treating more patients and pro- viding more complex care. However, the improved survival from septic shock, adult respira- Ctory distress syndrome (ARDS), and multiple organ system failure results in critically ill patients facing a spectrum of new complications secondary to both illness and treatment. A third of intensive care unit (ICU) admissions have a neurological complication detrimental to outcome.1 Neurological status (mainly depressed consciousness) is the major contributor to prolonged ventilation in a third of those who need it and is a significant factor in an additional 40%. Neurological complications double both the length of stay in hospital and the likelihood of death; the mortality rate for patients with neurological complications is 55% compared to 29% for those without. It is therefore unsurprising that neurologists are being increasingly called upon to review patients on the medical intensive care unit (MICU). A neurological opinion is usually requested: c to assess neurological manifestations of the primary disease process c to evaluate the consequences of critical care therapy c to offer a prognosis, or c determine brain death. The neurologist must approach these complex patients in a logical, -

Physical Examination of the Adult Patient with Respiratory Diseases: Inspection and Palpation
Eur Respir J, 1995, 8, 1584–1593 Copyright ERS Journals Ltd 1995 DOI: 10.1183/09031936.95.08091584 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 SERIES 'CHEST PHYSICAL EXAMINATION' Edited by J.C. Yernault Physical examination of the adult patient with respiratory diseases: inspection and palpation B. Maitre, T. Similowski, J-P. Derenne Physical examination of the adult patient with respiratory diseases: inspection and pal- Service de Pneumologie et de Réanimation, pation. B. Maitre, T. Similowski, J-P. Derenne. ©ERS Journals Ltd 1995. Groupe Hospitalier Pitié-Salpêtrière, Paris, ABSTRACT: Inspection of the thorax identifies the breathing position adopted by France. the patient, the shape of the thorax, the dynamics of respiration (breathing pat- tern, symmetry of expansion, mechanics and synchrony of rib cage and abdominal Correspondence: T. Similowski movements). Inspection of the neck adds useful information, particularly with Service de Pneumologie et de Réanimation respect to the dynamics of breathing. Palpation ascertains the signs suggested by Groupe Hospitalier Pitié-Salpêtrière inspection with respect to the mechanics of breathing. It also assesses the state of 47-83 Bd de l'Hôpital 75651 Paris Cedex 13 the pleura and pulmonary parenchyma by studying the tactile fremitus. It inte- France grates extrarespiratory signs, such as enlarged lymph nodes or breast abnorma- lities. Extrathoracic respiratory signs should also be systematically looked for, Keywords: Clinical examination including cyanosis, finger deformation, pulsus paradoxus, and pursed lips breath- inspection ing. palpation Interobserver agreement about respiratory signs has repeatedly been studied, and respiratory system generally found to be low, as are clinical-functional correlations. -

Guidelines for the Management of Severe Traumatic Brain Injury 4Th Edition
Guidelines for the Management of Severe Traumatic Brain Injury 4th Edition Nancy Carney, PhD Oregon Health & Science University, Portland, OR Annette M. Totten, PhD Oregon Health & Science University, Portland, OR Cindy O'Reilly, BS Oregon Health & Science University, Portland, OR Jamie S. Ullman, MD Hofstra North Shore-LIJ School of Medicine, Hempstead, NY Gregory W. J. Hawryluk, MD, PhD University of Utah, Salt Lake City, UT Michael J. Bell, MD University of Pittsburgh, Pittsburgh, PA Susan L. Bratton, MD University of Utah, Salt Lake City, UT Randall Chesnut, MD University of Washington, Seattle, WA Odette A. Harris, MD, MPH Stanford University, Stanford, CA Niranjan Kissoon, MD University of British Columbia, Vancouver, BC Andres M. Rubiano, MD El Bosque University, Bogota, Colombia; MEDITECH Foundation, Neiva, Colombia Lori Shutter, MD University of Pittsburgh, Pittsburgh, PA Robert C. Tasker, MBBS, MD Harvard Medical School & Boston Children’s Hospital, Boston, MA Monica S. Vavilala, MD University of Washington, Seattle, WA Jack Wilberger, MD Drexel University, Pittsburgh, PA David W. Wright, MD Emory University, Atlanta, GA Jamshid Ghajar, MD, PhD Stanford University, Stanford, CA Reviewed for evidence-based integrity and endorsed by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. September 2016 TABLE OF CONTENTS PREFACE ...................................................................................................................................... 5 ACKNOWLEDGEMENTS ............................................................................................................................................. -

Life After Subarachnoid Hemorrhage
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1281 Life after Subarachnoid Hemorrhage SVANTE WALLMARK ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-554-9762-0 UPPSALA urn:nbn:se:uu:diva-307949 2016 Dissertation presented at Uppsala University to be publicly examined in Rudbecksalen, Rudbecklaboratoriet, Dag Hammarskjölds väg 20, Uppsala, Friday, 13 January 2017 at 09:15 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in Swedish. Faculty examiner: Peter Appelros (Faculty of Medicine and Health, Örebro University, Örebro, Sweden). Abstract Wallmark, S. 2016. Life after Subarachnoid Hemorrhage. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1281. 97 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9762-0. Aneurysmal subarachnoid hemorrhage (SAH) is a devastating disease with mean age of 59 years. SAH accounts for 5% of all stroke and more than one quarter of potential life years lost through stroke. With the advanced neurosurgical methods of today two thirds of the patients survive. We know, however, that various cognitive, psychiatric and physical impairments are common that affect quality of life, social life, and the ability to work in the aftermath of SAH. The overall aim constituting this PhD dissertation is to better understand some of the challenges often faced by those surviving SAH. Two SAH patient cohorts have been studied. The first followed 96 consecutively included patients during the first year after ictus. Spasticity and cognitive impairment was assessed after 6 months and the Swedish stroke register follow-up form was used to investigate family support and the use of medical and social services.