5 • Modified Rankin Scale (Mrs)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Research Brief March 2017 Publication #2017-16
Research Brief March 2017 Publication #2017-16 Flourishing From the Start: What Is It and How Can It Be Measured? Kristin Anderson Moore, PhD, Child Trends Christina D. Bethell, PhD, The Child and Adolescent Health Measurement Introduction Initiative, Johns Hopkins Bloomberg School of Every parent wants their child to flourish, and every community wants its Public Health children to thrive. It is not sufficient for children to avoid negative outcomes. Rather, from their earliest years, we should foster positive outcomes for David Murphey, PhD, children. Substantial evidence indicates that early investments to foster positive child development can reap large and lasting gains.1 But in order to Child Trends implement and sustain policies and programs that help children flourish, we need to accurately define, measure, and then monitor, “flourishing.”a Miranda Carver Martin, BA, Child Trends By comparing the available child development research literature with the data currently being collected by health researchers and other practitioners, Martha Beltz, BA, we have identified important gaps in our definition of flourishing.2 In formerly of Child Trends particular, the field lacks a set of brief, robust, and culturally sensitive measures of “thriving” constructs critical for young children.3 This is also true for measures of the promotive and protective factors that contribute to thriving. Even when measures do exist, there are serious concerns regarding their validity and utility. We instead recommend these high-priority measures of flourishing -
Forensic Medicine
YEREVAN STATE MEDICAL UNIVERSITY AFTER M. HERATSI DEPARTMENT OF Sh. Vardanyan K. Avagyan S. Hakobyan FORENSIC MEDICINE Handout for foreign students YEREVAN 2007 This handbook is adopted by the Methodical Council of Foreign Students of the University DEATH AND ITS CAUSES Thanatology deals with death in all its aspects. Death is of two types: (1) somatic, systemic or clinical, and (2) molecular or cellular. Somatic Death: It is the complete and irreversible stoppage of the circulation, respiration and brain functions, but there is no legal definition of death. THE MOMENT OF DEATH: Historically (medically and legally), the concept of death was that of "heart and respiration death", i.e. stoppage of spontaneous heart and breathing functions. Heart-lung bypass machines, mechanical respirators, and other devices, however have changed this medically in favor of a new concept "brain death", that is, irreversible loss of Cerebral function. Brain death is of three types: (1) Cortical or cerebral death with an intact brain stem. This produces a vegetative state in which respiration continues, but there is total loss of power of perception by the senses. This state of deep coma can be produced by cerebral hypoxia, toxic conditions or widespread brain injury. (2) Brain stem death, where the cerebrum may be intact, though cut off functionally by the stem lesion. The loss of the vital centers that control respiration, and of the ascending reticular activating system that sustains consciousness, cause the victim to be irreversibly comatose and incapable of spontaneous breathing. This can be produced by raised intracranial pressure, cerebral oedema, intracranial haemorrhage, etc.(3) Whole brain death (combination of 1 and 2). -

Coma Stimulation: Suggested Activities
Coma stimulation: suggested activities Headway’s publications are all available to freely download from the information library on the charity’s website, while individuals and families can request hard copies of the booklets via the helpline. As a charity, we rely on donations from people like you to continue providing free information to people affected by brain injury. Donate today: www.headway.org.uk/donate. Introduction It is quite common for family members to feel ‘useless’ when a relative is in a coma, and to be desperate to do something to help. A coma stimulation programme (sometimes called a coma arousal programme) is an approach based on stimulating the unconscious person’s senses of hearing, touch, smell, taste and vision individually in order to help their recovery. There is still controversy over how effective it is to try to stimulate a person in coma. However, most would say that such programmes have some beneficial effect, even if only to provide something constructive for the family to do. It is very important that the activities used would have been enjoyable for the patient before the injury. For example, only play music they like and talk to them about subjects they are interested in. Try not to do anything for too long in order to avoid tiring the person out. A stimulation programme must only be started after discussion with the clinical staff, who will advise you what might be appropriate at any particular stage in the recovery process. Activity suggestions Here are some examples of activities that could form part of a coma stimulation programme: • Make sure that a few friends and family members visit regularly, rather than in large groups at a time. -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

How Can We Create Environments Where Hate Cannot Flourish?
How can we create environments where hate cannot flourish? Saturday, February 1 9:30 a.m. – 10:00 a.m. Check-In and Registration Location: Field Museum West Entrance 10:00 a.m. – 10:30 a.m. Introductions and Program Kick-Off JoAnna Wasserman, USHMM Education Initiatives Manager Location: Lecture Hall 1 10:30 a.m. – 11:30 a.m. Watch “The Path to Nazi Genocide” and Reflections JoAnna Wasserman, USHMM Education Initiatives Manager Location: Lecture Hall 1 11:30 a.m. – 11:45 a.m. Break and walk to State of Deception 11:45 a.m. – 12:30 p.m. Visit State of Deception Interpretation by Holocaust Survivor Volunteers from the Illinois Holocaust Museum Location: Upper level 12:30 p.m. – 1:00 p.m. Breakout Session: Reflections on Exhibit Tim Kaiser, USHMM Director, Education Initiatives David Klevan, USHMM Digital Learning Strategist JoAnna Wasserman, USHMM Education Initiatives Manager Location: Lecture Hall 1, Classrooms A and B Saturday, February 2 (continued) 1:00 p.m. – 1:45 p.m. Lunch 1:45 p.m. – 2:45 p.m. A Survivor’s Personal Story Bob Behr, USHMM Survivor Volunteer Interviewed by: Ann Weber, USHMM Program Coordinator Location: Lecture Hall 1 2:45 p.m. – 3:00 p.m. Break 3:00 p.m. – 3:45 p.m. Student Panel: Beyond Indifference Location: Lecture Hall 1 Moderator: Emma Pettit, Sustained Dialogue Campus Network Student/Alumni Panelists: Jazzy Johnson, Northwestern University Mary Giardina, The Ohio State University Nory Kaplan-Kelly, University of Chicago 3:45 p.m. – 4:30 p.m. Breakout Session: Sharing Personal Reflections Tim Kaiser, USHMM Director, Education Initiatives David Klevan, USHMM Digital Learning Strategist JoAnna Wasserman, USHMM Education Initiatives Manager Location: Lecture Hall 1, Classrooms A and B 4:30 p.m. -
The Utility of Genetic Risk Scores in Predicting the Onset of Stroke March 2021 6
DOT/FAA/AM-21/24 Office of Aerospace Medicine Washington, DC 20591 The Utility of Genetic Risk Scores in Predicting the Onset of Stroke Diana Judith Monroy Rios, M.D1 and Scott J. Nicholson, Ph.D.2 1. KR 30 # 45-03 University Campus, Building 471, 5th Floor, Office 510 Bogotá D.C. Colombia 2. FAA Civil Aerospace Medical Institute, 6500 S. MacArthur Blvd Rm. 354, Oklahoma City, OK 73125 March 2021 NOTICE This document is disseminated under the sponsorship of the U.S. Department of Transportation in the interest of information exchange. The United States Government assumes no liability for the contents thereof. _________________ This publication and all Office of Aerospace Medicine technical reports are available in full-text from the Civil Aerospace Medical Institute’s publications Web site: (www.faa.gov/go/oamtechreports) Technical Report Documentation Page 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. DOT/FAA/AM-21/24 4. Title and Subtitle 5. Report Date March 2021 The Utility of Genetic Risk Scores in Predicting the Onset of Stroke 6. Performing Organization Code 7. Author(s) 8. Performing Organization Report No. Diana Judith Monroy Rios M.D1, and Scott J. Nicholson, Ph.D.2 9. Performing Organization Name and Address 10. Work Unit No. (TRAIS) 1 KR 30 # 45-03 University Campus, Building 471, 5th Floor, Office 510, Bogotá D.C. Colombia 11. Contract or Grant No. 2 FAA Civil Aerospace Medical Institute, 6500 S. MacArthur Blvd Rm. 354, Oklahoma City, OK 73125 12. Sponsoring Agency name and Address 13. Type of Report and Period Covered Office of Aerospace Medicine Federal Aviation Administration 800 Independence Ave., S.W. -

FC = Mac V2 R V = 2Πr T F = T 1
Circular Motion Gravitron Cars Car Turning (has a curse) Rope Skip There must be a net inward force: Centripetal Force v2 F = maC a = C C R Centripetal acceleration 2πR v v v = R v T v 1 f = T The motorcycle rider does 13 laps in 150 s. What is his period? Frequency? R = 30 m [11.5 s, 0.087 Hz] What is his velocity? [16.3 m/s] What is his aC? [8.9 m/s2] If the mass is 180 kg, what is his FC? [1600 N] The child rotates 5 times every 22 seconds... What is the period? 60 kg [4.4 s] What is the velocity? [2.86 m/s] What is the acceleration? Which way does it point? [4.1 m/s2] What must be the force on the child? [245 N] Revolutions Per Minute (n)2πR v = 60 s An Ipod's hard drive rotates at 4200 RPM. Its radius is 0.03 m. What is the velocity in m/s of its edge? 1 Airplane Turning v = 232 m/s (520 mph) aC = 7 g's What is the turn radius? [785 m = 2757 ft] 2 FC Solving Circular Motion Problems 1. Determine FC (FBD) 2 2. Set FC = m v R 3. Solve for unknowns The book's mass is 2 kg it is spun so that the tension is 45 N. What is the velocity of the book in m/s? In RPM? R = 0.75 m [4.11 m/s] [52 RPM] What is the period (T) of the book? [1.15 s] The car is traveling at 25 m/s and the turn's radius is 63 m. -
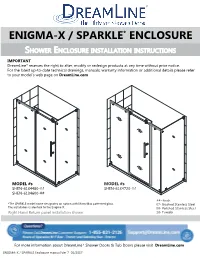
ENIGMA X Aka SPARKLE Enclosure Manual Ver 7 012017
ENIGMA-X / SPARKLE* ENCLOSURE SHOWER ENCLOSURE INSTALLATION INSTRUCTIONS IMPORTANT DreamLine® reserves the right to alter, modify or redesign products at any time without prior notice. For the latest up-to-date technical drawings, manuals, warranty information or additional details please refer to your model’s web page on DreamLine.com MODEL #s MODEL #s SHEN-6134480-## SHEN-6134720-## SHEN-6134600-## ##=finish *The SPARKLE model name designates an option with MirrorMax patterned glass. 07- Brushed Stainless Steel The installation is identical to the Enigma-X. 08- Polished Stainless Steel Right Hand Return panel installation shown 18- Tuxedo For more information about DreamLine® Shower Doors & Tub Doors please visit DreamLine.com ENIGMA-X / SPARKLE Enclosure manual Ver 7 01/2017 This model is treated with DreamLine’s exclusive ClearMaxTM Glass technology. This is a specially formulated coating that prevents the build up of soap and water spots. Install the surface with the ClearMaxTM label towards the inside of the shower. Please note that depending on the model, the glass may be coated on either one or both surfaces. For best results, squeegee the glass after each use and dry with a soft cloth. ENIGMA-X / SPARKLE Enclosure manual Ver 7 01/2017 2 B B A A C ! E IMPORTANT INFORMATION REGARDING THE INSTALLATION OF THIS SHOWER DOOR D PANEL DOOR F Right hand door installation shown as an example A Guide Rail Brackets must be firmly D Roller Guards must be postioned and attached to the wall. Installation into a secured within 1/16” of Upper Guide Rail. stud is strongly recommended. -

Primary Screening for Breast Cancer with Conventional Mammography: Clinical Summary
Primary Screening for Breast Cancer With Conventional Mammography: Clinical Summary Population Women aged 40 to 49 y Women aged 50 to 74 y Women aged ≥75 y The decision to start screening should be No recommendation. Recommendation Screen every 2 years. an individual one. Grade: I statement Grade: B Grade: C (insufficient evidence) These recommendations apply to asymptomatic women aged ≥40 y who do not have preexisting breast cancer or a previously diagnosed high-risk breast lesion and who are not at high risk for breast cancer because of a known underlying genetic mutation Risk Assessment (such as a BRCA1 or BRCA2 gene mutation or other familial breast cancer syndrome) or a history of chest radiation at a young age. Increasing age is the most important risk factor for most women. Conventional digital mammography has essentially replaced film mammography as the primary method for breast cancer screening Screening Tests in the United States. Conventional digital screening mammography has about the same diagnostic accuracy as film overall, although digital screening seems to have comparatively higher sensitivity but the same or lower specificity in women age <50 y. For women who are at average risk for breast cancer, most of the benefit of mammography results from biennial screening during Starting and ages 50 to 74 y. While screening mammography in women aged 40 to 49 y may reduce the risk for breast cancer death, the Stopping Ages number of deaths averted is smaller than that in older women and the number of false-positive results and unnecessary biopsies is larger. The balance of benefits and harms is likely to improve as women move from their early to late 40s. -
National Rappel Operations Guide
National Rappel Operations Guide 2019 NATIONAL RAPPEL OPERATIONS GUIDE USDA FOREST SERVICE National Rappel Operations Guide i Page Intentionally Left Blank National Rappel Operations Guide ii Table of Contents Table of Contents ..........................................................................................................................ii USDA Forest Service - National Rappel Operations Guide Approval .............................................. iv USDA Forest Service - National Rappel Operations Guide Overview ............................................... vi USDA Forest Service Helicopter Rappel Mission Statement ........................................................ viii NROG Revision Summary ............................................................................................................... x Introduction ...................................................................................................... 1—1 Administration .................................................................................................. 2—1 Rappel Position Standards ................................................................................. 2—6 Rappel and Cargo Letdown Equipment .............................................................. 4—1 Rappel and Cargo Letdown Operations .............................................................. 5—1 Rappel and Cargo Operations Emergency Procedures ........................................ 6—1 Documentation ................................................................................................ -

Evaluation and Management in an Urgent Care Setting
Syncope Evaluation and Management in an Urgent Care Setting Urgent message: When a patient presents to urgent care after a syncopal event, the clinician’s charge is to determine whether the episode was of benign or potentially life-threatening etiology and whether the patient should be transferred for further evaluation. Kenneth V. Iserson, MD, MBA, FACEP, FAAEM, Professor of Emergency Medicine, The University of Arizona, Tucson, AZ Introduction yncope is a sudden, transient loss of consciousness with a loss of postural tone (typically, falling). It results from an abrupt, transient, and diffuse cerebral Smalfunction and is quickly followed by sponta- neous recovery. The term syncope excludes seizures, coma, shock, or other states of altered consciousness. Many patients will ascribe their syncopal episode to a sit- uationally mediated vasovagal episode. Despite this, the goals in the urgent care setting include the following: Ⅲ Determining whether the patient’s episode was actually a syncopal or presyncopal event, and if it could have a life-threatening etiology Ⅲ Stabilizing the patient Ⅲ Transferring those patients who need further diag- nostic studies or therapeutic interventions © John Bolesky, Artville © John Bolesky, Epidemiology Syncope accounts for up to 3% of emergency depart- common in young adults, while cardiac syncope ment (ED) visits and up to 6% of hospital admissions becomes increasingly more frequent with advancing each year in the United States.1,2 At some time in their age.4 The chance of having at least one syncopal episode lives, up to about half the population (12% to 48%) of in childhood is between 15% and 50%.5 Though a people may experience syncope.3 benign cause is usually found, syncope in children war- Syncope occurs in all age groups, but it is most com- rants prompt detailed evaluation.6 mon in adults. -

Percent R, X and Z Based on Transformer KVA
SHORT CIRCUIT FAULT CALCULATIONS Short circuit fault calculations as required to be performed on all electrical service entrances by National Electrical Code 110-9, 110-10. These calculations are made to assure that the service equipment will clear a fault in case of short circuit. To perform the fault calculations the following information must be obtained: 1. Available Power Company Short circuit KVA at transformer primary : Contact Power Company, may also be given in terms of R + jX. 2. Length of service drop from transformer to building, Type and size of conductor, ie., 250 MCM, aluminum. 3. Impedance of transformer, KVA size. A. %R = Percent Resistance B. %X = Percent Reactance C. %Z = Percent Impedance D. KVA = Kilovoltamp size of transformer. ( Obtain for each transformer if in Bank of 2 or 3) 4. If service entrance consists of several different sizes of conductors, each must be adjusted by (Ohms for 1 conductor) (Number of conductors) This must be done for R and X Three Phase Systems Wye Systems: 120/208V 3∅, 4 wire 277/480V 3∅ 4 wire Delta Systems: 120/240V 3∅, 4 wire 240V 3∅, 3 wire 480 V 3∅, 3 wire Single Phase Systems: Voltage 120/240V 1∅, 3 wire. Separate line to line and line to neutral calculations must be done for single phase systems. Voltage in equations (KV) is the secondary transformer voltage, line to line. Base KVA is 10,000 in all examples. Only those components actually in the system have to be included, each component must have an X and an R value. Neutral size is assumed to be the same size as the phase conductors.