Scientific Report 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TESE Thaisa Francis César Sampaio Sarmento.Pdf
UNIVERSIDADE FEDERAL DE PERNAMBUCO CENTRO DE ARTES E COMUNICAÇÃO DEPARTAMENTO DE DESIGN PROGRAMA DE PÓS-GRADUAÇÃO EM DESIGN Thaisa Francis César Sampaio Sarmento MODELO CONCEITUAL DE AMBIENTE DE APRENDIZAGEM ADEQUADO A PRÁTICAS COM BLENDED LEARNING PARA ESCOLAS DE ENSINO MÉDIO Recife 2017 THAISA FRANCIS CÉSAR SAMPAIO SARMENTO MODELO CONCEITUAL DE AMBIENTE DE APRENDIZAGEM ADEQUADO A PRÁTICAS COM BLENDED LEARNING PARA ESCOLAS DE ENSINO MÉDIO Tese apresentada à Coordenação do Programa de PósGraduação em Design da Universidade Federal de Pernambuco, para a obtenção do grau de Doutor em Design, sob orientação da Prof.ª Drª Vilma Villarouco e do coorientador Prof. Dr. Alex Sandro Gomes. Recife 2017 Catalogação na fonte Bibliotecário Jonas Lucas Vieira, CRB4-1204 S246m Sarmento, Thaisa Francis César Sampaio Modelo conceitual de ambiente de aprendizagem adequado a práticas com blended learning para escolas de ensino médio / Thaisa Francis César Sampaio Sarmento. – Recife, 2017. 261 f.: il., fig. Orientadora: Vilma Villarouco dos Santos. Tese (Doutorado) – Universidade Federal de Pernambuco, Centro de Artes e Comunicação. Design, 2018. Inclui referências e apêndices. 1. Ambiente de aprendizagem. 2. Ergonomia do ambiente construído. 3. Design de interiores. 4. Design Science Research. I. Santos, Vilma Villarouco dos (Orientadora). II. Título. 745.2 CDD (22.ed.) UFPE (CAC 2018-29) UNIVERSIDADE FEDERAL DE PERNAMBUCO PROGRAMA DE PÓS-GRADUAÇÃO EM DESIGN PARECER DA COMISSÃO EXAMINADORA DE DEFESA DE TESE DE DOUTORADO ACADÊMICO DE Thaisa Francis César Sampaio Sarmento "MODELO CONCEITUAL DE AMBIENTE DE APRENDIZAGEM ADEQUADO À PRÁTICAS COM BLENDED LEARNING PARA ESCOLAS DE ENSINO MÉDIO." ÁREA DE CONCENTRAÇÃO: Planejamento e Contextualização de Artefatos. A comissão examinadora, composta pelos professores abaixo, considera o(a) candidato(a) Thaisa Francis César Sampaio Sarmento _APROVAD(A)__. -
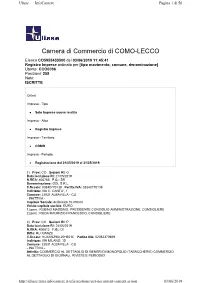
Camera Di Commercio Di COMO-LECCO
Ulisse — InfoCamere Pagina 1 di 56 Camera di Commercio di COMO-LECCO Elenco CO5955433500 del 03/06/2019 11:45:41 Registro Imprese ordinato per [tipo movimento, comune, denominazione] Utente: CCO0096 Posizioni: 258 Note: ISCRITTE Criteri: Impresa - Tipo Solo Imprese nuove iscritte Impresa - Albo Registro Imprese Impresa - Territorio COMO Impresa - Periodo Registrazione dal 01/05/2019 al 31/05/2019. 1) Prov: CO Sezioni RI: O Data iscrizione RI: 21/05/2019 N.REA: 400765 F.G.: SR Denominazione: GDL S.R.L. C.fiscale: 03840770139 Partita IVA: 03840770139 Indirizzo: VIA C. CANTU', 1 Comune: 22031 ALBAVILLA - CO - INATTIVA - Capitale Sociale: deliberato 10.000,00 Valuta capitale sociale: EURO 1) pers.: RUBINO MASSIMO, PRESIDENTE CONSIGLIO AMMINISTRAZIONE, CONSIGLIERE 2) pers.: RODA MAURIZIO FRANCESCO, CONSIGLIERE 2) Prov: CO Sezioni RI: P Data iscrizione RI: 24/05/2019 N.REA: 400812 F.G.: DI Ditta: HU XIANZE C.fiscale: HUXXNZ96L20H501C Partita IVA: 02062370669 Indirizzo: VIA MILANO, 15 Comune: 22031 ALBAVILLA - CO - INATTIVA - Attività: COMMERCIO AL DETTAGLIO DI GENERI DI MONOPOLIO (TABACCHERIE) COMMERCIO AL DETTAGLIO DI GIORNALI, RIVISTE E PERIODICI http://ulisse.intra.infocamere.it/ulis/gestione/get -document -content.action 03/ 06/ 2019 Ulisse — InfoCamere Pagina 2 di 56 1) pers.: HU XIANZE, TITOLARE FIRMATARIO 3) Prov: CO Sezioni RI: P - A Data iscrizione RI: 23/05/2019 N.REA: 400781 F.G.: DI Ditta: POLETTI GIORGIO C.fiscale: PLTGRG71T21C933L Partita IVA: 03838110132 Indirizzo: VIA ROMA, 83 Comune: 22032 ALBESE CON CASSANO - CO Data dom./accert.: 21/05/2019 Data inizio attività: 21/05/2019 Attività: INTONACATURA E TINTEGGIATURA C. Attività: 43.34 I / 43.34 A 1) pers.: POLETTI GIORGIO, TITOLARE FIRMATARIO 4) Prov: CO Sezioni RI: P - C Data iscrizione RI: 07/05/2019 N.REA: 400576 F.G.: DI Ditta: AZIENDA AGRICOLA LOLO DI BOVETTI FRANCESCO C.fiscale: BVTFNC84S01F205Q Partita IVA: 03839240136 Indirizzo: LOCALITA' RONDANINO SN Comune: 22024 ALTA VALLE INTELVI - CO Data inizio attività: 02/05/2019 Attività: ALLEVAMENTO DI EQUINI, COLTIVAZIONI FORAGGERE E SILVICOLTURA. -

BUCO DEL PIOMBO Accesso: Dalla Statale Arosio-Canzo (SP40), Salire
BUCO DEL PIOMBO Accesso: dalla statale Arosio-Canzo (SP40), salire a Crevenna in direzione Canzo, poi seguire le indicazioni per il ristorante Canova dove si parcheggia. Avvicinamento: dal ristorante Canova salire per la mulattiera fino all’eremo di San Salvatore. Prendere la strada sterrata che attraversa il prato a sinistra e seguirla fino a un torrente generalmente secco, poco sotto la parete con cascata. Salire direttamente per una traccia nel bosco fino alla base delle vie. 20’ dall’eremo. In alternativa da Albavilla si può salire in auto fino allo Zoccolo, indicazioni per trattoria Alpina, e dalla grotta scendere a valle fino alle vie. Soluzione sconsigliata a causa della scomparsa del sentiero La parete è esposta a est, si può scalare sempre nelle mezze stagioni, ottimo in inverno al mattino. La roccia asciuga molto in fretta. In primavera alcuni settori sono proibiti a causa della nidificazione del falco pellegrino. SETTORE BRACCIA DI PIOMBO Tre vie ben pulite e attrezzate dall’alto a fix da Saverio De Toffol sul pilastro bianco ben visibile dal sentiero. La roccia stratificata affatica velocemente gli avambracci ma offre molte prese e appoggi. Portare: corda due mezze corde se si scende in doppia, 14 rinvii Discesa: in doppia da Braccia di Piombo o a piedi seguendo il sentiero in cima alla fascia di roccia verso la scala di legno Giurassica 2005 80m 6b+ (6b obb.) Inizia in cima ad un breve zoccolo con corda fissa, è la via di sinistra L1: 5c L2: 6a+ L3: 6b+ L4: 6a Braccia di Piombo 2004 80m 6b+ (6b obb.) Inizia in cima ad un breve zoccolo con corda fissa, è la via di destra L1: 6b L2: 6a L3: 6b+ L4: 4 Mario Imperial 2009 100m 7a (6b obb.) Inizia a destra dello zoccolo con corda fissa, pochi metri sopra il sentiero, fix alla base. -
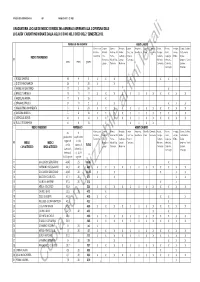
Copia Non Utilizzabile Ai Fini Legali
Allegato alla deliberazione n. del composto da n. 2 fogli GRADUATORIA LOCALE DEI MEDICI DI MEDICINA GENERALE ASPIRANTI ALLA COPERTURA DELLE LOCALITA' CARENTI INDIVIDUATE DALLA ASL DI COMO NEL CORSO DEL 2° SEMESTRE 2013. PUNTEGGIO DA ANZIANITA' AMBITI CARENTI Albese con Cassina Alserio, Fenegrò, Lurate Bregnano, Rovello Cirimido, Arosio, Brenna, Inverigo, Canzo, Caslino, Cassano, Rizzardi, Anzano del Limido Caccivio, Rovellasca. Porro. Lomazzo. Carugo, Cantù, Lurago Castelmarte, MEDICI TRASFERENDI Tavernerio. Fino Parco, Comasco, Olgiate Cabiate, Capiago d'Erba. Eupilio, N° Mornasco, Alzate B.za, Lurago Comasco. Mariano Intimiano, Longone, Ponte anni mesi giorni Luisago. Orsenigo. Marinone. Comense. Carimate, Lambro, Cucciago. Proserpio. 1 ROSSI SAVERIO 60 9 0 XXX X XXX 2 DI STEFANO MARISA 29 3 28 XX 3 ANGELINO GAETANO 17 2 24 X 4 BRACUTI ANGELA 13 11 11 XXXXXXXXXXXX 5 ANDOLINA MARIA 11 8 16 X 6 SPAGNOLI PAOLA 9112XX XXX 7 MALACRINO ANNUNZIATA 8824XXXXXXXXXXXX 8 ANCONA ANGELA 5818XXXXXXXXXXXX 9 CETKOVIC BORIS 4614XXXXXXXXXXXX 10 RULLO ROSAMARIA 4418 XXXXX MEDICI INSERENDI PUNTEGGIO AMBITI CARENTI da in Albese con Cassina Alserio, Fenegrò, Lurate Bregnano, Rovello Cirimido, Arosio, Brenna, Inverigo, Canzo, Caslino, Cassano, Rizzardi, Anzano del Limido Caccivio, Rovellasca. Porro. Lomazzo. Carugo, Cantù, Lurago Castelmarte, graduatoria applicazione Tavernerio. Fino Parco, Comasco, Olgiate Cabiate, Capiago d'Erba. Eupilio, regionale art.34, N° MEDICI MEDICI Mornasco, Alzate B.za, Lurago Comasco. Mariano Intimiano, Longone, Ponte art.34, comma -

Seleção Feminina Nos Jogos Olímpicos 25 Women’S National Team in the Olympic’S Cidades-Sede | Host-Cities 26
ÍNDICE SUMMARY インデックス COORDENADORa DE SELEÇÕES FEMININAS 03 Duda Luizelli | Women’s National Teams Coordinator TÉCNICA PIA SUNDHAGE | Head Coach 04 jogadoras | Players 06 numeração | Team Jersey numbers 12 Comissão Técnica | Coaching Staff 13 Caminho para Tóquio 2020 | Road to Tokyo 2020 14 Fase de Grupos Tóquio 2020 | Group Phase 18 CHAVEAMENTO | Knockout Phase 24 Seleção Feminina nos Jogos Olímpicos 25 Women’s National Team In the Olympic’s Cidades-Sede | Host-Cities 26 Curiosidades | Trivia 33 Redes Sociais | Social 35 2 ”35 ANOS DEDICADOS AO FUTEBOL FEMININO ” Ex-atleta da Seleção Brasileira Feminina, Duda Luizelli é a primeira mulher a liderar a Coordenação das Seleções Brasileiras Femininas. Anunciada em setembro de 2020, a contratação da gaúcha de 49 anos faz parte de um novo momento do futebol feminino na CBF, que conta com maior participação das mulheres. São 35 anos dedicados à modalidade, desde os tempos de atleta até a coordenação das Seleções Femininas Principal, Sub-20 e Sub-17. O despertar como jogadora foi aos 14 anos no Internacional-RS. Foi no duda luizelli clube colorado que a meia ganhou notoriedade e chegou à Seleção Brasileira. A estreia com a camisa Canarinho foi aos 20 anos. No total, COORDENADORA DAS SELEÇÕES foram oito anos vestindo o uniforme verde e amarelo, tendo no BRASILEIRAS FEMININAS currículo a conquista do bicampeonato Sul-Americano, em 1995. Na década de 90, Duda foi uma das primeiras brasileiras a atuar no futebol internacional. Com a camisa do Milan e do Verona, da Itália, a meia brilhou no campeonato italiano por duas temporadas. Ao retornar ao Brasil, voltou a vestir a camisa 10 do Internacional, e foi com o time colorado que encerrou a carreira aos 30 anos, somando conquistas importantes, como o pentacampeonato do Campeonato Gaúcho, o tricampeonato da Copa Sul e o Torneio de CIVATE (Itália). -

Adi Merone – Ente Gestore Cooperativa Sociale Quadrifoglio S.C
ENTI EROGATORI ADI Distretto Brianza • PAXME ASSISTANCE • ALE.MAR. COOPERATIVA SOCIALE ONLUS Como (CO) Via Castelnuovo, 1 Vigevano (PV) Via SS. Crispino e Crispiniano, 2 Tel. 031.4490272 / 340.2323524 Tel. 0381/73703 – fax 0381/76908 e-mail: [email protected] e-mail: [email protected] Anche cure palliative • PUNTO SERVICE C/O RSA Croce di Malta • ASSOCIAZIONE A.QU.A. ONLUS Canzo (CO) Via Brusa, 20 Milano (MI) Via Panale, 66 Tel. 346.2314311 - fax 031.681787 Tel. 02.36552585 - fax 02.36551907 e-mail: [email protected] e-mail: [email protected] • SAN CAMILLO - PROGETTO ASSISTENZA s.r.l. • ASSOCIAZIONE ÀNCORA Varese (VA) Via Lungolago di Calcinate, 88 Longone al Segrino (CO) Via Diaz, 4 Tel. 0332.264820 - fax 0332.341682 Tel/fax 031.3357127 e-mail: [email protected] e-mail: [email protected] Anche cure palliative Solo cure palliative • VIVISOL Solo per i Comuni di: Albavilla, Alserio, Alzate Sesto San Giovanni (MI) Via Manin, 167 Brianza, Anzano del Parco, Asso, Barni, Caglio, Tel. 800.990.161 – fax 02.26223985 Canzo, Caslino d’Erba, Castelmarte, Civenna, e-mail: [email protected] Erba, Eupilio, Lambrugo, Lasnigo, Longone al Anche cure palliative Segrino, Magreglio, Merone, Monguzzo,Orsenigo, Ponte Lambro, Proserpio, Pusiano, Rezzago, Sormano, Valbrona. • ATHENA CENTRO MEDICO Ferno (VA) Via De Gasperi, 1 Tel. 0331.726361 – Fax 0331.728270 e-mail: [email protected] Anche cure palliative • ADI MERONE – ENTE GESTORE COOPERATIVA SOCIALE QUADRIFOGLIO S.C. ONLUS Merone (CO) Via Leopardi, 5/1 Tel 031.651781 - 329.2318205 -

Ai Sig. Sindaci COMUNE AROSIO Email: [email protected]
Giunta Regionale DIREZIONE GENERALE AMBIENTE, ENERGIA E RETI PREVENZIONE INQUINAMENTO ATMOSFERICO PROTEZIONE ARIA E PREVENZIONE INQUINAMENTI FISICI Piazza Città di Lombardia n.1 www.regione.lombardia.it 20124 Milano [email protected] Tel 02 6765.1 Ai Sig. Sindaci COMUNE AROSIO Email: [email protected] COMUNE DI CABIATE Email: [email protected] COMUNE DI CANTU' Email: [email protected] COMUNE DI CAPIAGO INTIMIANO Email: [email protected] COMUNE DI CARUGO Email: [email protected] COMUNE DI CASNATE CON BERNATE Email: [email protected] COMUNE DI FIGINO SERENZA Email: [email protected] COMUNE DI FINO MORNASCO Email: [email protected] COMUNE DI GRANDATE Email: [email protected] COMUNE DI LIPOMO Email: [email protected] COMUNE DI MARIANO COMENSE Email: [email protected] Referente per l'istruttoria della pratica: GIAN LUCA GURRIERI Tel. 02/6765.5461 COMUNE DI NOVEDRATE Email: [email protected] COMUNE DI SENNA COMASCO Email: [email protected] LORO SEDI Oggetto : Disposizioni in ordine al fermo programmato del traffico feriale, ai sensi della d.G.R. 11/07/2008, n. VIII/7635 “Misure prioritarie di limitazione alla circolazione e all’utilizzo dei veicoli. Terzo provvedimento attuativo inerente i veicoli previsti dall’articolo 22, commi 1, 2, 5 ed ai sensi dell’art. 13, L.R. 11 dicembre 2006, n. 24. Ulteriori misure per il contenimento dell’inquinamento da combustione di biomasse legnose ai sensi dell’art. 11, L.R. -

GIRO D'italia
GIRO d’ITALIA THE STORY OF THE WORLD’S MOST BEAUTIFUL BIKE RACE COLIN O’BRIEN giro 4th proof.indd 3 22/2/17 17:33:35 First published in Great Britain in 2017 by PURSUIT BOOKS An imprint of Profile Books Ltd 3 Holford Yard Bevin Way London w c 1x 9h d www.profilebooks.com Copyright © Colin O’Brien, 2017 1 3 5 7 9 10 8 6 4 2 Designed and typeset by [email protected] Printed and bound in Great Britain by Clays, St Ives plc The moral right of the author has been asserted. All rights reserved. Without limiting the rights under copyright reserved above, no part of this publication may be reproduced, stored or introduced into a retrieval system, or transmitted, in any form or by any means (electronic, mechanical, photocopying, recording or otherwise), without the prior written permission of both the copyright owner and the publisher of this book. A CIP catalogue record for this book is available from the British Library. ISBN 978 1 78125 716 6 eISBN 978 1 78283 290 4 giro 4th proof.indd 4 22/2/17 17:33:35 CONTENTS Preface // vii Introduction // 1 1 The Giro is born // 7 2 The early years // 17 SALITA FAMOSA Roccaraso, Abruzzo // 26 3 Alfredo Binda: Il Grande Antipatico // 29 4 The Devil wears wool shorts // 40 SALITA FAMOSA Croce d’Aune, Veneto // 45 5 Fascism and the Giro // 48 6 Bartali and Coppi, Coppi and Bartali // 62 7 Magni: Il Terzo Uomo // 80 SALITA FAMOSA Passo dello Stelvio, Trentino-Alto Adige // 98 8 Gracious Gimondi and merciless Merckx // 102 SALITA FAMOSA Blockhaus, Abruzzo // 112 9 The Sheriff and the Rifle Shot // -

COVID-19, Women, Girls and Sport: Build Back Better
Photo: pcruciatti / Shutterstock.com COVID-19, Women, Girls and Sport: Build Back Better Introduction Over the past year, women in sport have gained centre and address their specific needs in response unprecedented attention. Events like the Women´s and recovery plans. World Cup, the Cricket T20, record attendance at The impacts of COVID-19 are already being felt harder women’s games and the expectations for Tokyo Olympic by women and girls in many areas of life due to Games to achieve gender parity raised awareness and gender inequalities, i and we see this mirrored in sport. mobilized action around women´s participation and This brief is informed by the Sports for Generation leadership in sport, equal pay, safeguarding policies, Equality Frameworkii, launched by UN Women and representation in the media and incentives for girls the International Olympic Committee in March 2020. to play. The pandemic of COVID-19 now threatens to It focuses on the impacts of COVID-19 on women and erase this momentum as the sport world has been girls in sports in five areas: Leadership, Gender-Based forced to cancel or postpone events, schools have Violence, Economic Opportunities, Media Participation closed, and people are staying home. Existing gaps and Representation, and Girls Participation in Sport. It between women and men, girls and boys in both elite presents key recommendations to different actors in the and grassroots sport may widen if governments, sport sport ecosystem that go beyond mitigating the impact of organizations, sponsors, civil society, athletes, media the crisis on women and girls, and create a future in and and UN agencies do not put women and girls at the through sport that builds back better. -

Juniores Prov Girone B SS2021
CALENDARIO Stagione 2020 - 2021 JUNIORES UNDER 19 COMO Girone B 1a Giornata 2a Giornata 3a Giornata 10 Ott - 30 Gen 17 Ott - 6 Feb 24 Ott - 13 Feb ARDITA COMO 1934 PONTELAMBRESE ALBAVILLA ARDITA COMO 1934 ARDITA COMO 1934 CITTADELLA 1945 CALCIO MENAGGIO 1920 STELLA AZZURRA AROSIO ALTABRIANZA TAVERNERIO CARUGO ACADEMY CALCIO MENAGGIO 1920 ALTABRIANZA TAVERNERIO CARUGO ACADEMY FC CABIATE FC CABIATE CALCIO MENAGGIO 1920 CARUGO ACADEMY ORATORIO FIGINO CALCIO CITTADELLA 1945 ALBAVILLA GIOVANILE CANZESE INVERIGO FC CABIATE STELLA AZZURRA AROSIO INVERIGO ORATORIO FIGINO CALCIO ORATORIO FIGINO CALCIO TAVERNOLA INVERIGO PONTELAMBRESE NOVEDRATE sq.B GIOVANILE CANZESE PONTELAMBRESE NOVEDRATE sq.B NOVEDRATE sq.B ALBAVILLA TAVERNOLA ALTABRIANZA TAVERNERIO STELLA AZZURRA AROSIO CITTADELLA 1945 TAVERNOLA GIOVANILE CANZESE 4a Giornata 5a Giornata 6a Giornata 7a Giornata 31 Ott - 20 Feb 2001 7 Nov - 27 Feb 14 Nov - 6 Mar 21 Nov - 13 Mar ALBAVILLA INVERIGO ALTABRIANZA TAVERNERIO STELLA AZZURRA AROSIO ALBAVILLA CARUGO ACADEMY ALTABRIANZA TAVERNERIO GIOVANILE CANZESE ALTABRIANZA TAVERNERIO FC CABIATE CALCIO MENAGGIO 1920 GIOVANILE CANZESE ARDITA COMO 1934 INVERIGO CALCIO MENAGGIO 1920 ALBAVILLA CITTADELLA 1945 NOVEDRATE sq.B CARUGO ACADEMY PONTELAMBRESE CITTADELLA 1945 TAVERNOLA CARUGO ACADEMY CITTADELLA 1945 GIOVANILE CANZESE CARUGO ACADEMY FC CABIATE ORATORIO FIGINO CALCIO GIOVANILE CANZESE FC CABIATE FC CABIATE PONTELAMBRESE ORATORIO FIGINO CALCIO CALCIO MENAGGIO 1920 INVERIGO CITTADELLA 1945 ORATORIO FIGINO CALCIO ALTABRIANZA TAVERNERIO INVERIGO NOVEDRATE -

Dati Sui Pagamenti Anno 2017 Per Trasparenza
LIQUIDAZIONI 2017 LIQUIDAZIONI 2017 DATA IMPORTO CAUSALE PAGAMENTO BENEFICIARIO SETTORE CAPITOLO LIQUIDAZION FORN. ENERGIA ELETTRICA MESE SETTORE FINANZE E 10/02/2017 61,03 NOVEMBRE 2016 CHIOSTRO IREN MERCATO S.P.A. 105010740 BILANCIO VOLTORRE GAVIRATE ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 50,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 50,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA ATTIVITA' DI QUALIFICA DEGLI IMPIANTI 13/01/2017 250,00 FOTOVOLTAICI - SISTEMI EFFICIENTI GSE SPA SETTORE EDILIZIA 104020200 UTENZA FT 28/2014 SERV.ASSISTENZA IMPIANTI 13/01/2017 527,22 FTV X LAVORI MANUTENZ. -

UNIVERSIDADE FEDERAL DO TRIÂNGULO MINEIRO Francielle
UNIVERSIDADE FEDERAL DO TRIÂNGULO MINEIRO Francielle Toniolo Nicodemos Furtado de Mendonça GRUPOS DE EDUCAÇÃO EM SAÚDE COM IDOSOS: EDUCAÇÃO PERMANENTE COM PROFISSIONAIS DA ATENÇÃO PRIMÁRIA UBERABA/MG 2015 Francielle Toniolo Nicodemos Furtado de Mendonça GRUPOS DE EDUCAÇÃO EM SAÚDE COM IDOSOS: EDUCAÇÃO PERMANENTE COM PROFISSIONAIS DA ATENÇÃO PRIMÁRIA Dissertação apresentada ao programa de Pós- Graduação Stricto Sensu em Atenção à Saúde da Universidade Federal do Triângulo Mineiro como requisito parcial para obtenção do título de mestre. Linha de pesquisa: atenção à saúde das populações. Eixo temático: Saúde do adulto e idoso. Orientador: Prof. Dr. Álvaro da Silva Santos. UBERABA/MG 2015 FRANCIELLE TONIOLO NICODEMOS FURTADO DE MENDONÇA Grupos de educação em saúde com idosos: Educação permanente com profissionais da atenção primária Dissertação apresentada ao Programa de Pós- Graduação Stricto Sensu em Atenção à Saúde da Universidade Federal do Triângulo Mineiro como requisito parcial para obtenção do título de mestre. Uberaba, 27 de novembro de 2015. Banca Examinadora ________________________________________________ Profo Dro Álvaro da Silva Santos – Orientador Universidade Federal do Triângulo Mineiro ________________________________________________ Profa Dra Leiner Resende Rodrigues Universidade Federal do Triângulo Mineiro ________________________________________________ Profa Dra Vânia Del’Arco Paschoal Faculdade de Medicina de São José do Rio Preto Dedico esse trabalho à minha mãe Denise, ao meu irmão Tiago e aos meus avós Maria e João, pelo amor e carinho com que sempre cuidaram de mim, e pelo incentivo e apoio aos estudos. Dedico também ao meu marido Marcelo, companheiro nesta jornada, que constantemente me incentiva a estudar mais e mais, e está sempre ao meu lado, oferecendo seu carinho, apoio e paciência em todos os momentos, principalmente naqueles em que eu mais precisei.