BIOCHEMISTRY of TRYPTOPHAN in HEALTH and DISEASE Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Joosten, Han M.L.J.; Herst, Patricia M.; Drift, Chris Van Der
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Groningen University of Groningen Characterization of Glutamine-Requiring Mutants of Pseudomonas aeruginosa Janssen, Dick B.; Joosten, Han M.L.J.; Herst, Patricia M.; Drift, Chris van der Published in: Archives of Microbiology IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 1982 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Janssen, D. B., Joosten, H. M. L. J., Herst, P. M., & Drift, C. V. D. (1982). Characterization of Glutamine- Requiring Mutants of Pseudomonas aeruginosa. Archives of Microbiology, 131(4). Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 12-11-2019 JOURNAL OF BACTERIOLOGY, Sept. 1982, p. 1176-1183 Vol. 151, No. -

METABOLIC EVOLUTION in GALDIERIA SULPHURARIA By
METABOLIC EVOLUTION IN GALDIERIA SULPHURARIA By CHAD M. TERNES Bachelor of Science in Botany Oklahoma State University Stillwater, Oklahoma 2009 Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY May, 2015 METABOLIC EVOLUTION IN GALDIERIA SUPHURARIA Dissertation Approved: Dr. Gerald Schoenknecht Dissertation Adviser Dr. David Meinke Dr. Andrew Doust Dr. Patricia Canaan ii Name: CHAD M. TERNES Date of Degree: MAY, 2015 Title of Study: METABOLIC EVOLUTION IN GALDIERIA SULPHURARIA Major Field: PLANT SCIENCE Abstract: The thermoacidophilic, unicellular, red alga Galdieria sulphuraria possesses characteristics, including salt and heavy metal tolerance, unsurpassed by any other alga. Like most plastid bearing eukaryotes, G. sulphuraria can grow photoautotrophically. Additionally, it can also grow solely as a heterotroph, which results in the cessation of photosynthetic pigment biosynthesis. The ability to grow heterotrophically is likely correlated with G. sulphuraria ’s broad capacity for carbon metabolism, which rivals that of fungi. Annotation of the metabolic pathways encoded by the genome of G. sulphuraria revealed several pathways that are uncharacteristic for plants and algae, even red algae. Phylogenetic analyses of the enzymes underlying the metabolic pathways suggest multiple instances of horizontal gene transfer, in addition to endosymbiotic gene transfer and conservation through ancestry. Although some metabolic pathways as a whole appear to be retained through ancestry, genes encoding individual enzymes within a pathway were substituted by genes that were acquired horizontally from other domains of life. Thus, metabolic pathways in G. sulphuraria appear to be composed of a ‘metabolic patchwork’, underscored by a mosaic of genes resulting from multiple evolutionary processes. -
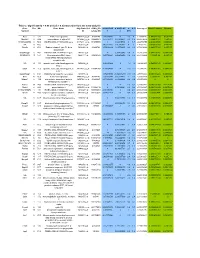
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Amino Acid Disorders 105
AMINO ACID DISORDERS 105 Massaro, A. S. (1995). Trypanosomiasis. In Guide to Clinical tions in biological fluids relatively easy. These Neurology (J. P. Mohrand and J. C. Gautier, Eds.), pp. 663– analyzers separate amino acids either by ion-ex- 667. Churchill Livingstone, New York. Nussenzweig, V., Sonntag, R., Biancalana, A., et al. (1953). Ac¸a˜o change chromatography or by high-pressure liquid de corantes tri-fenil-metaˆnicos sobre o Trypanosoma cruzi in chromatography. The results are plotted as a graph vitro: Emprego da violeta de genciana na profilaxia da (Fig. 1). The concentration of each amino acid can transmissa˜o da mole´stia de chagas por transfusa˜o de sangue. then be calculated from the size of the corresponding O Hospital (Rio de Janeiro) 44, 731–744. peak on the graph. Pagano, M. A., Segura, M. J., DiLorenzo, G. A., et al. (1999). Cerebral tumor-like American trypanosomiasis in Most amino acid disorders can be diagnosed by acquired immunodeficiency syndrome. Ann. Neurol. 45, measuring the concentrations of amino acids in 403–406. blood plasma; however, some disorders of amino Rassi, A., Trancesi, J., and Tranchesi, B. (1982). Doenc¸ade acid transport are more easily recognized through the Chagas. In Doenc¸as Infecciosas e Parasita´rias (R. Veroesi, Ed.), analysis of urine amino acids. Therefore, screening 7th ed., pp. 674–712. Guanabara Koogan, Sa˜o Paulo, Brazil. Spina-Franc¸a, A., and Mattosinho-Franc¸a, L. C. (1988). for amino acid disorders is best done using both South American trypanosomiasis (Chagas’ disease). In blood and urine specimens. Occasionally, analysis of Handbook of Clinical Neurology (P. -

Upregulated Kynurenine Pathway Enzymes in Aortic Atherosclerotic Aneurysm: Macrophage Kynureninase Downregulates Inflammation
The official journal of the Japan Atherosclerosis Society and the Asian Pacific Society of Atherosclerosis and Vascular Diseases Original Article J Atheroscler Thromb, 2021; 28: 000-000. http://doi.org/10.5551/jat.58248 Upregulated Kynurenine Pathway Enzymes in Aortic Atherosclerotic Aneurysm: Macrophage Kynureninase Downregulates Inflammation Masanori Nishimura1, 2, Atsushi Yamashita2, Yunosuke Matsuura3, Junichi Okutsu4, Aiko Fukahori4, Tsuyoshi Hirata4, Tomohiro Nishizawa5, Hirohito Ishii1, Kazunari Maekawa2, Eriko Nakamura2, Kazuo Kitamura3, Kunihide Nakamura1 and Yujiro Asada2 1Division of Cardiovascular Surgery, Department of Surgery, Faculty of Medicine, University of Miyazaki, Miyazaki, Japan 2Department of Pathology, Faculty of Medicine, University of Miyazaki, Miyazaki, Japan 3Department of Internal Medicine, Faculty of Medicine, University of Miyazaki, Miyazaki, Japan 4Translational Research Department, Daiichi Sankyo RD Novare Co., Ltd., Tokyo, Japan 5Specialty Medicine Research Laboratories I, Daiichi Sankyo Co., Ltd., Tokyo, Japan Aims: Inflammation and hypertension contribute to the progression of atherosclerotic aneurysm in the aorta. Vascular cell metabolism is regarded to modulate atherogenesis, but the metabolic alterations that occur in ath- erosclerotic aneurysm remain unknown. The present study aimed to identify metabolic pathways and metabo- lites in aneurysmal walls and examine their roles in atherogenesis. Methods: Gene expression using microarray and metabolite levels in the early atherosclerotic lesions and aneu- rysmal walls obtained from 42 patients undergoing aortic surgery were investigated (early lesion n=11, aneu- rysm n=35) and capillary electrophoresis–time-of-flight mass spectrometry (early lesion n=14, aneurysm n=38). Using immunohistochemistry, the protein expression and localization of the identified factors were examined (early lesion n=11, non-aneurysmal advanced lesion n=8, aneurysm n=11). -

HIV-1 Envelope Mimicry of Host Enzyme Kynureninase Does Not Disrupt Tryptophan Metabolism
HIV-1 Envelope Mimicry of Host Enzyme Kynureninase Does Not Disrupt Tryptophan Metabolism This information is current as Todd Bradley, Guang Yang, Olga Ilkayeva, T. Matt Holl, of September 29, 2021. Ruijun Zhang, Jinsong Zhang, Sampa Santra, Christopher B. Fox, Steve G. Reed, Robert Parks, Cindy M. Bowman, Hilary Bouton-Verville, Laura L. Sutherland, Richard M. Scearce, Nathan Vandergrift, Thomas B. Kepler, M. Anthony Moody, Hua-Xin Liao, S. Munir Alam, Roger McLendon, Jeffrey I. Everitt, Christopher B. Newgard, Downloaded from Laurent Verkoczy, Garnett Kelsoe and Barton F. Haynes J Immunol 2016; 197:4663-4673; Prepublished online 14 November 2016; doi: 10.4049/jimmunol.1601484 http://www.jimmunol.org/content/197/12/4663 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2016/11/12/jimmunol.160148 Material 4.DCSupplemental References This article cites 67 articles, 31 of which you can access for free at: http://www.jimmunol.org/content/197/12/4663.full#ref-list-1 by guest on September 29, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. -

Amino Acid Catabolism in Staphylococcus Aureus
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-16-2016 Amino Acid Catabolism in Staphylococcus aureus Cortney Halsey University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Bacteriology Commons Recommended Citation Halsey, Cortney, "Amino Acid Catabolism in Staphylococcus aureus" (2016). Theses & Dissertations. 160. https://digitalcommons.unmc.edu/etd/160 This Dissertation is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. Amino Acid Catabolism in Staphylococcus aureus By Cortney R. Halsey A DISSERTATION Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of the Requirements For the Degree of Doctor of Philosophy Pathology and Microbiology Under the Supervision of Dr. Paul D. Fey University of Nebraska Medical Center Omaha, Nebraska October 2016 Supervisory Committee: Kenneth Bayles, Ph.D. Steven Carson, Ph.D. Paul Dunman, Ph.D. Rakesh Singh, Ph.D. ii Acknowledgements First and foremost, I would like to thank my mentor, Dr. Paul Fey, whose patience and support over the past six years has been critical to my success as a graduate student. Paul has given me opportunities to grow as a scientist and person, for which I will be forever thankful. I would also like to thank Dr. Ken Bayles, Dr. Steven Carson, Dr. Paul Dunman, and Dr. Rakesh Singh for serving on my supervisory committee. -

Supplementary Materials
Supplementary Materials COMPARATIVE ANALYSIS OF THE TRANSCRIPTOME, PROTEOME AND miRNA PROFILE OF KUPFFER CELLS AND MONOCYTES Andrey Elchaninov1,3*, Anastasiya Lokhonina1,3, Maria Nikitina2, Polina Vishnyakova1,3, Andrey Makarov1, Irina Arutyunyan1, Anastasiya Poltavets1, Evgeniya Kananykhina2, Sergey Kovalchuk4, Evgeny Karpulevich5,6, Galina Bolshakova2, Gennady Sukhikh1, Timur Fatkhudinov2,3 1 Laboratory of Regenerative Medicine, National Medical Research Center for Obstetrics, Gynecology and Perinatology Named after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia 2 Laboratory of Growth and Development, Scientific Research Institute of Human Morphology, Moscow, Russia 3 Histology Department, Medical Institute, Peoples' Friendship University of Russia, Moscow, Russia 4 Laboratory of Bioinformatic methods for Combinatorial Chemistry and Biology, Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry of the Russian Academy of Sciences, Moscow, Russia 5 Information Systems Department, Ivannikov Institute for System Programming of the Russian Academy of Sciences, Moscow, Russia 6 Genome Engineering Laboratory, Moscow Institute of Physics and Technology, Dolgoprudny, Moscow Region, Russia Figure S1. Flow cytometry analysis of unsorted blood sample. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S2. Flow cytometry analysis of unsorted liver stromal cells. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S3. MiRNAs expression analysis in monocytes and Kupffer cells. Full-length of heatmaps are presented. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
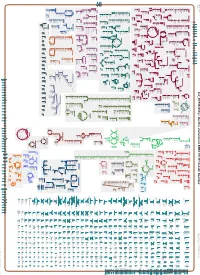
Generate Metabolic Map Poster
Authors: Pallavi Subhraveti Ron Caspi Peter Midford Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_001591825Cyc: Bacillus vietnamensis NBRC 101237 Cellular Overview Connections between pathways are omitted for legibility. Anamika Kothari sn-glycerol phosphate phosphate pro phosphate phosphate phosphate thiamine molybdate D-xylose D-ribose glutathione 3-phosphate D-mannitol L-cystine L-djenkolate lanthionine α,β-trehalose phosphate phosphate [+ 3 more] α,α-trehalose predicted predicted ABC ABC FliY ThiT XylF RbsB RS10935 UgpC TreP PutP RS10200 PstB PstB RS10385 RS03335 RS20030 RS19075 transporter transporter of molybdate of phosphate α,β-trehalose 6-phosphate L-cystine D-xylose D-ribose sn-glycerol D-mannitol phosphate phosphate thiamine glutathione α α phosphate phosphate phosphate phosphate L-djenkolate 3-phosphate , -trehalose 6-phosphate pro 1-phosphate lanthionine molybdate phosphate [+ 3 more] Metabolic Regulator Amino Acid Degradation Amine and Polyamine Biosynthesis Macromolecule Modification tRNA-uridine 2-thiolation Degradation ATP biosynthesis a mature peptidoglycan a nascent β an N-terminal- -

THE ROLE of KYNURENINE, a TRYPTOPHAN METABOLITE THAT INCREASES with AGE, in MUSCLE ATROPHY and LIPID PEROXIDATION) by Helen Eliz
THE ROLE OF KYNURENINE, A TRYPTOPHAN METABOLITE THAT INCREASES WITH AGE, IN MUSCLE ATROPHY AND LIPID PEROXIDATION) By Helen Elizabeth Kaiser Submitted to the Faculty of the Graduate School of Augusta University in partial fulfillment of the Requirements of the Degree of (Doctor of Philosophy in Cellular Biology and Anatomy) April 2020 COPYRIGHT© 2020 by Helen Kaiser ACKNOWLEDGEMENTS I wish to express my deepest gratitude to my mentor Dr. Mark Hamrick. His support and advice were invaluable to my learning and development as a scientist. I would like to especially recognize Dr. Hamrick’s honesty to data, and kindness to everyone around him. It was an honor to work as his student, and to be a part of this project. I would like to thank my committee members, Drs. Carlos Isales, Meghan McGee-Lawrence, and Yutao Liu, for their continued support, guidance, and helpful suggestions. They have helped to shape and focus this project, and have augmented my experience as a student during the development of my dissertation. Additionally, I want to recognize and thank Dr. Sadanand Fulzele for sharing his wealth of knowledge in techniques, and always keeping his door open for student’s questions. Next, a most heartfelt thanks to my lab mates: Andrew Khayrullin, Bharati Mendhe, Ling Ruan and Emily Parker. This project has been a team effort, all of them have been fundamental to its success. I further want to show my appreciation for the rest of the department of Cellular Biology and Anatomy at Augusta University. The histology core members Donna Kumiski and Penny Roon for their direct help in sectioning, and contributions to this project. -

Histidinaemia in Mouse and Man
Arch Dis Child: first published as 10.1136/adc.49.7.545 on 1 July 1974. Downloaded from Archives of Disease in Childhood, 1974, 49, 545. Histidinaemia in mouse and man GRAHAME BULFIELD and HENRIK KACSER From the Department of Genetics, University of Edinburgh Bulfield, G., and Kacser, H. (1974). Archives of Disease in Childhood, 49, 545. Histidinaemia in mouse and man. A recently discovered mutant in the mouse was found to have very low levels of histidase. It is an autosomal recessive. In its enzymic and metabolic properties it appears to be a homologue ofhuman histidinaemia. While the homozygous mouse mutants show no overt abnormalities, offspring of histidinaemic mothers display a balance defect resulting in circling behaviour. This is associated with vestibular damage during in utero development. Mental retardation caused by human maternal phenylketonuria may have a similar aetiology. There are well recognized advantages in studying histidine and its derivatives. The enzymic and animal models in the investigation of human metabolic changes in both mouse and human diseases. The increasing number of disorders in mutants appear to be the same. In addition, man which are reported to have a genetic basis maternal histidinaemia in the mouse has a terato- (McKusick, 1971; Raine, 1972) makes it desirable to genic effect on the developing inner ear which results find and investigate animal homologues with the in abnormal behaviour of the affected offspring. same genic lesions. The genetically most in- These findings may be relevant to the aetiology of vestigated laboratory mammal is the mouse, with human histidinaemia. over 500 known mutants (Green, 1966; Searle, 1973).