Pneumonia Treatment Algorithm with Aspiration Addendum 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ceftazidime for Injection) PHARMACY BULK PACKAGE – NOT for DIRECT INFUSION
PRESCRIBING INFORMATION FORTAZ® (ceftazidime for injection) PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of FORTAZ and other antibacterial drugs, FORTAZ should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ceftazidime is a semisynthetic, broad-spectrum, beta-lactam antibacterial drug for parenteral administration. It is the pentahydrate of pyridinium, 1-[[7-[[(2-amino-4 thiazolyl)[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-2-carboxy-8-oxo-5-thia-1 azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-, hydroxide, inner salt, [6R-[6α,7β(Z)]]. It has the following structure: The molecular formula is C22H32N6O12S2, representing a molecular weight of 636.6. FORTAZ is a sterile, dry-powdered mixture of ceftazidime pentahydrate and sodium carbonate. The sodium carbonate at a concentration of 118 mg/g of ceftazidime activity has been admixed to facilitate dissolution. The total sodium content of the mixture is approximately 54 mg (2.3 mEq)/g of ceftazidime activity. The Pharmacy Bulk Package vial contains 709 mg of sodium carbonate. The sodium content is approximately 54 mg (2.3mEq) per gram of ceftazidime. FORTAZ in sterile crystalline form is supplied in Pharmacy Bulk Packages equivalent to 6g of anhydrous ceftazidime. The Pharmacy Bulk Package bottle is a container of sterile preparation for parenteral use that contains many single doses. The contents are intended for use in a pharmacy admixture program and are restricted to the preparation of admixtures for intravenous use. THE PHARMACY BULK PACKAGE IS NOT FOR DIRECT INFUSION, FURTHER DILUTION IS REQUIRED BEFORE USE. -

Severe Sepsis and Septic Shock Antibiotic Guide
Stanford Health Issue Date: 05/2017 Stanford Antimicrobial Safety and Sustainability Program Severe Sepsis and Septic Shock Antibiotic Guide Table 1: Antibiotic selection options for healthcare associated and/or immunocompromised patients • Healthcare associated: intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days, residence in a nursing home or other long-term care facility, hospitalization in an acute care hospital for two or more days within the prior 90 days, attendance at a hospital or hemodialysis clinic within the prior 30 days • Immunocompromised: Receiving chemotherapy, known systemic cancer not in remission, ANC <500, severe cell-mediated immune deficiency Table 2: Antibiotic selection options for community acquired, immunocompetent patients Table 3: Antibiotic selection options for patients with simple sepsis, community acquired, immunocompetent patients requiring hospitalization. Risk Factors for Select Organisms P. aeruginosa MRSA Invasive Candidiasis VRE (and other resistant GNR) Community acquired: • Known colonization with MDROs • Central venous catheter • Liver transplant • Prior IV antibiotics within 90 day • Recent MRSA infection • Broad-spectrum antibiotics • Known colonization • Known colonization with MDROs • Known MRSA colonization • + 1 of the following risk factors: • Prolonged broad antibacterial • Skin & Skin Structure and/or IV access site: ♦ Parenteral nutrition therapy Hospital acquired: ♦ Purulence ♦ Dialysis • Prolonged profound • Prior IV antibiotics within 90 days ♦ Abscess -

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

Synermox 500 Mg/125 Mg Tablets
New Zealand Data Sheet 1. PRODUCT NAME Synermox 500 mg/125 mg Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Synermox 500 mg/125 mg Tablets: Each film‐coated tablet contains amoxicillin trihydrate equivalent to 500 mg amoxicillin, with potassium clavulanate equivalent to 125 mg clavulanic acid. Excipient(s) with known effect For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Synermox 500 mg/125 mg Tablets: White to off‐white, oval shaped film‐coated tablets, debossed with “RX713” on one side and plain on the other. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Synermox is indicated in adults and children (see sections 4.2, 4.4 and 5.1) for short term treatment of common bacterial infections such as: Upper Respiratory Tract Infections (including ENT) e.g. Tonsillitis, sinusitis, otitis media. Lower Respiratory Tract Infection e.g. acute exacerbations of chronic bronchitis, lobar and broncho‐pneumonia. Genito‐urinary Tract Infections e.g. Cystitis, urethritis, pyelonephritis, female genital infections. Skin and Soft Tissue Infections. Bone and Joint Infections e.g. Osteomyelitis. Other Infections e.g. septic abortion, puerperal sepsis, intra‐abdominal sepsis, septicaemia, peritonitis, post‐surgical infections. Synermox is indicated for prophylaxis against infection which may be associated with major surgical procedures such as those involving: Gastro‐intestinal tract Pelvic cavity 1 | Page Head and neck Cardiac Renal Joint replacement Biliary tract surgery Infections caused by amoxicillin susceptible organisms are amenable to Synermox treatment due to its amoxicillin content. Mixed infections caused by amoxicillin susceptible organisms in conjunction with Synermox‐susceptible beta‐lactamase‐producing organisms may therefore be treated by Synermox. -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -
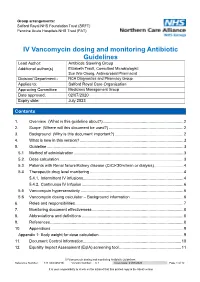
IV Vancomycin Dosing and Monitoring Antibiotic Guidelines Reference Number: 144TD(C)25(H3) Version Number: 6.1 Issue Date: 21/07/2020 Page 1 of 12
Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) IV Vancomycin dosing and monitoring Antibiotic Guidelines Lead Author: Antibiotic Steering Group Additional author(s) Elizabeth Trautt, Consultant Microbiologist; Sue Wei Chong, Antimicrobial Pharmacist Division/ Department:: NCA Diagnostics and Pharmacy Group Applies to: Salford Royal Care Organisation Approving Committee Medicines Management Group Date approved: 02/07/2020 Expiry date: July 2023 Contents Contents 1. Overview (What is this guideline about?) ....................................................................... 2 2. Scope (Where will this document be used?) .................................................................. 2 3. Background (Why is this document important?) ............................................................. 2 4. What is new in this version? ............................................................................................ 3 5. Guideline ......................................................................................................................... 3 5.1 Method of administration ................................................................................................. 3 5.2. Dose calculation .............................................................................................................. 3 5.3. Patients with Renal failure/Kidney disease (CrCl<30ml/min or dialysis) .......................... 4 5.4 Therapeutic drug level monitoring .................................................................................. -

Eml-2017-Antibacterials-Eng.Pdf
Consideration of antibacterial medicines as part of the revisions to 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee, 2017 and this summary should be read in conjunction with the full report (WHO Technical Report Series, No. 1006; http://apps.who.int/iris/bitstream/10665/259481/1/9789241210157-eng.pdf?ua=1). The revised lists of essential medicines (in English) are available as follows: 2017 WHO Model List of Essential Medicines for adults (EML) http://www.who.int/medicines/publications/essentialmedicines/20th_EML2017_FINAL_amend edAug2017.pdf?ua=1 2017 Model List of Essential Medicines for children (EMLc) http://www.who.int/medicines/publications/essentialmedicines/6th_EMLc2017_FINAL_amend edAug2017.pdf?ua=1 Summary of changes to Section 6.2 Antibacterials: Section 6 of the EML covers anti-infective medicines. Disease-specific subsections within Section 6, such as those covering medicines for tuberculosis, HIV, hepatitis and malaria, have been regularly reviewed and updated, taking into consideration relevant WHO treatment guidelines. -

Can Amoxicillin Clavulanate Be Used for Treating MRSA?
ORIGINAL ARTICLE Can amoxicillin clavulanate be used for treating MRSA? Sana Jamil1, Uzma Saad2, Saleem Hafiz1 Jamil S, Saad U, Hafiz S. Can amoxicillin clavulanate be used for treating positive for Beta lactamase production 52.1% of these Beta lactamase MRSA? J Pharmacol Res December-2017;1(1):21-23. producing MRSA were sensitive to amoxicillin-clavulanate and the remaining (47.9%) were resistant. Objective: To determine the frequency of beta lactamase producing Conclusion: If beta lactamase producing Staphlococcus aureus are tested Staphlococcus aureus and their sensitivity to Amoxicillin clavulanate in against beta-lactam antimicrobial agents in combination with clavulanic major cities of Pakistan. acid or sulbactam (Beta-lactamase inhibitors), they become susceptible to Setting: Various laboratories of the country with one as the central the Beta-lactam antimicrobial agents. This might have therapeutic and Laboratory. epidemiological implications in near future. Materials and Methods: Seven hundred and ninety two consecutive Key Words: Methicillin resistant Staphylococcus aureus; Vancomycin clinical isolates of Staphylococcus aureus were collected from 8 intermediate Staphylococcus aureus; Vancomycin resistant Staphylococcus laboratories all over Pakistan i.e. Karachi, Peshawar, Lahore, Sukkhur, aureus; Clinical laboratory standard institute; Penicillinase resistant Islamabad, Quetta, and Mirpur, Azad Kashmir. Antibiotic sensitivity was penicillins; Minimum inhibitory concentration; Penicillin binding proteins; done by Kirby Bauer disc diffusion method and Beta lactamase production Center of disease control was identified by using Nitrocefin test. Results: Forty two percent of the isolates were found to be Methicillin resistant Staphylococcus aureus (MRSA) out of which 87.9% were INTRODUCTION lactamase producing MRSA in Pakistan and its sensitivity to Amoxicillin clavulanate. -

Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F
Philadelphia College of Osteopathic Medicine DigitalCommons@PCOM PCOM Scholarly Papers 2014 Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F. DeBellis Kimberly L. Barefield Philadelphia College of Osteopathic Medicine, [email protected] Follow this and additional works at: https://digitalcommons.pcom.edu/scholarly_papers Part of the Medicine and Health Sciences Commons Recommended Citation DeBellis, Heather F. and Barefield, Kimberly L., "Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia" (2014). PCOM Scholarly Papers. 1913. https://digitalcommons.pcom.edu/scholarly_papers/1913 This Article is brought to you for free and open access by DigitalCommons@PCOM. It has been accepted for inclusion in PCOM Scholarly Papers by an authorized administrator of DigitalCommons@PCOM. For more information, please contact [email protected]. Open Access: Full open access to Clinical Medicine Reviews this and thousands of other papers at http://www.la-press.com. in Therapeutics Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia Heather F. DeBellis and Kimberly L. Tackett South University School of Pharmacy, Savannah, GA, USA. ABSTR ACT: Ceftaroline fosamil is a new fifth-generation cephalosporin indicated for the treatment of community-acquired bacterial pneumonia (CABP). It possesses antimicrobial effects against both Gram-positive and Gram-negative bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), but not against anaerobes. Organisms covered by this novel agent that are commonly associated with CABP are Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, and Klebsiella pneumoniae; however, ceftaroline fosamil lacks antimicrobial activity against Pseudomonas and Acinetobacter species. -

A New Trigger of Morbilliform Eruption in the Setting of Atypical Infectious
A New Trigger of Morbilliform Eruption in the Setting of Atypical Infectious Mononucleosis Roxanne Rajaii, DO,* Megan Furniss, DO,** John Pui, MD,*** Brett Bender, DO**** *Dermatology Resident, PGY2, Beaumont Hospital - Farmington Hills, Farmington Hills, MI **Dermatology Resident, PGY4, Beaumont Hospital - Farmington Hills, Farmington Hills, MI ***Dermatopathologist, Beaumont Hospital - Farmington Hills, Farmington Hills, MI ****Dermatologist, Beaumont Hospital - Farmington Hills, Farmington Hills, MI Disclosures: None Correspondence: Roxanne Rajaii, DO; [email protected] Abstract Morbilliform eruptions, also commonly referred to as exanthematous or maculopapular drug eruptions, are the most common type of hypersensitivity reaction and can vary in etiology. Antibiotics are a common trigger, most notably amoxicillin or ampicillin in the setting of a concomitant and acute Epstein-Barr virus (EBV) infection. However, other antibiotics have been identified to cause a similar reaction in the setting of EBV. Cephalexin, a commonly used cephalosporin, is the only antibiotic in its class that has been implicated in causing such a phenomenon. We present a unique case of a morbilliform eruption in the setting of EBV secondary to the use of cefepime, further outlining the importance of conservative antibiotic use and awareness of such a reaction in this specific patient population, not only with penicillins but also with a wider spectrum of antibiotics. Introduction acquired pyelonephritis, as she had been admitted Work-up included the following laboratory tests: Epstein-Barr virus (EBV) infects more than a month prior to that for status asthmaticus. complete blood count, complete metabolic panel, 98% of the world’s adult population and is the Four days later, she presented with an urticarial anti-nuclear antibody, creatinine phosphate kinase, most common cause of infectious mononucleosis morbilliform rash. -

Cephalosporins Can Be Prescribed Safely for Penicillin-Allergic Patients ▲
JFP_0206_AE_Pichichero.Final 1/23/06 1:26 PM Page 106 APPLIED EVIDENCE New research findings that are changing clinical practice Michael E. Pichichero, MD University of Rochester Cephalosporins can be Medical Center, Rochester, NY prescribed safely for penicillin-allergic patients Practice recommendations an allergic reaction to cephalosporins, ■ The widely quoted cross-allergy risk compared with the incidence of a primary of 10% between penicillin and (and unrelated) cephalosporin allergy. cephalosporins is a myth (A). Most people produce IgG and IgM antibodies in response to exposure to ■ Cephalothin, cephalexin, cefadroxil, penicillin1 that may cross-react with and cefazolin confer an increased risk cephalosporin antigens.2 The presence of of allergic reaction among patients these antibodies does not predict allergic, with penicillin allergy (B). IgE cross-sensitivity to a cephalosporin. ■ Cefprozil, cefuroxime, cefpodoxime, Even penicillin skin testing is generally not ceftazidime, and ceftriaxone do not predictive of cephalosporin allergy.3 increase risk of an allergic reaction (B). Reliably predicting cross-reactivity ndoubtedly you have patients who A comprehensive review of the evidence say they are allergic to penicillin shows that the attributable risk of a cross- U but have difficulty recalling details reactive allergic reaction varies and is of the reactions they experienced. To be strongest when the chemical side chain of safe, we often label these patients as peni- the specific cephalosporin is similar to that cillin-allergic without further questioning of penicillin or amoxicillin. and withhold not only penicillins but Administration of cephalothin, cepha- cephalosporins due to concerns about lexin, cefadroxil, and cefazolin in penicillin- potential cross-reactivity and resultant IgE- allergic patients is associated with a mediated, type I reactions. -

ESBL Disc Tests - Rev.2 / 19.06.2014 ESBL Disc Tests Disc Tests for Detection of ESBL-Producing Enterobacteriaceae
© Liofilchem® - ESBL Disc Tests - Rev.2 / 19.06.2014 ESBL Disc Tests Disc tests for detection of ESBL-producing Enterobacteriaceae. DESCRIPTION Extended-spectrum β-lactamases (ESBLs) are enzymes hydrolyzing most penicillins and cephalosporins, including oxyimino- β-lactam compunds but not cephamycins and carbapenems. Most ESBLs belong to the Amber class A of β-lactamases and are inhibited by β-lactamases inhibitors: clavulanic acid, sulbatam and tazobactam. ESBL production has been observed mostly in Enterobacteriaceae, particularly Escherichia coli and Klebsiella pnuemoniae, but all other clinically-relevant Enterobacteriaceae species are also common ESBL-producers. In many areas, ESBL detection and characterization is recommended or mandatory for infection control purpose. ESBL detection involves two important steps. The first is a screening test with an indicator cephalosporin which looks for resistance or diminished susceptibility, thus identifying isolates likely to be harboring ESBLs. The second step is a confirmation test which evaluates the synergy between an oxyimino cephalosporin and clavulanic acid, distinguishing isolates with ESBLs from those that are resistant for other reasons. METHOD PRINCIPLE ESBL Disc Screening Disk-diffusion method for ESBL screening can be performed using cefpodoxime, ceftazidime, aztreonam, cefotaxime and ceftriaxone, according to EUCAST and/or CLSI guidelines (table 1). Since the affinity of ESBLs for different substrates is variable, the use of more than one of these agents for screening improves the sensitivity of detection. However, it is adequate to use the couple cefotaxime (or ceftriaxone) and ceftazidime. If only one drug can be used, cefpodoxime is the most sensitive indicator cephalosporin for detection of ESBL production may be used for screening.