An in Silico Study of the Ligand Binding to Human Cytochrome P450 2D6
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Β-Phenylethylamines and the Isoquinoline Alkaloids
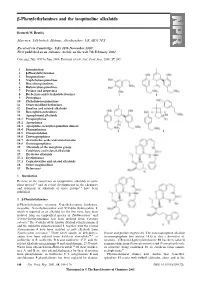
-Phenylethylamines and the isoquinoline alkaloids Kenneth W. Bentley Marrview, Tillybirloch, Midmar, Aberdeenshire, UK AB51 7PS Received (in Cambridge, UK) 28th November 2000 First published as an Advance Article on the web 7th February 2001 Covering: July 1999 to June 2000. Previous review: Nat. Prod. Rep., 2000, 17, 247. 1 Introduction 2 -Phenylethylamines 3 Isoquinolines 4 Naphthylisoquinolines 5 Benzylisoquinolines 6 Bisbenzylisoquinolines 7 Pavines and isopavines 8 Berberines and tetrahydoberberines 9 Protopines 10 Phthalide-isoquinolines 11 Other modified berberines 12 Emetine and related alkaloids 13 Benzophenanthridines 14 Aporphinoid alkaloids 14.1 Proaporphines 14.2 Aporphines 14.3 Aporphine–benzylisoquinoline dimers 14.4 Phenanthrenes 14.5 Oxoaporphines 14.6 Dioxoaporphines 14.7 Aristolochic acids and aristolactams 14.8 Oxoisoaporphines 15 Alkaloids of the morphine group 16 Colchicine and related alkaloids 17 Erythrina alkaloids 17.1 Erythrinanes 17.2 Cephalotaxine and related alkaloids 18 Other isoquinolines 19 References 1 Introduction Reviews of the occurrence of isoquinoline alkaloids in some plant species 1,2 and of recent developments in the chemistry and synthesis of alkaloids of these groups 3–6 have been published. 2 -Phenylethylamines β-Phenylethylamine, tyramine, N-methyltyramine, hordenine, mescaline, N-methylmescaline and N,N-dimethylmescaline 1, which is reported as an alkaloid for the first time, have been isolated from an unspecified species of Turbinocarpus 7 and N-trans-feruloyltyramine has been isolated from Cananga odorata.8 The N-oxides of the known alkaloid culantraramine 2 and the unknown culantraraminol 3, together with the related avicennamine 4 have been isolated as new alkaloids from Zanthoxylum avicennae.9 Three novel amides of dehydrotyr- leucine and proline respectively. -

Metabolism and Pharmacokinetics in the Development of New Therapeutics for Cocaine and Opioid Abuse
University of Mississippi eGrove Electronic Theses and Dissertations Graduate School 2012 Metabolism And Pharmacokinetics In The Development Of New Therapeutics For Cocaine And Opioid Abuse Pradeep Kumar Vuppala University of Mississippi Follow this and additional works at: https://egrove.olemiss.edu/etd Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Vuppala, Pradeep Kumar, "Metabolism And Pharmacokinetics In The Development Of New Therapeutics For Cocaine And Opioid Abuse" (2012). Electronic Theses and Dissertations. 731. https://egrove.olemiss.edu/etd/731 This Dissertation is brought to you for free and open access by the Graduate School at eGrove. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of eGrove. For more information, please contact [email protected]. METABOLISM AND PHARMACOKINETICS IN THE DEVELOPMENT OF NEW THERAPEUTICS FOR COCAINE AND OPIOID ABUSE A Dissertation presented in partial fulfillment of requirements for the degree of Doctor of Philosophy in Pharmaceutical Sciences in the Department of Pharmaceutics The University of Mississippi by PRADEEP KUMAR VUPPALA April 2012 Copyright © 2012 by Pradeep Kumar Vuppala All rights reserved ABSTRACT Cocaine and opioid abuse are a major public health concern and the cause of significant morbidity and mortality worldwide. The development of effective medication for cocaine and opioid abuse is necessary to reduce the impact of this issue upon the individual and society. The pharmacologic treatment for drug abuse has been based on one of the following strategies: agonist substitution, antagonist treatment, or symptomatic treatment. This dissertation is focused on the role of metabolism and pharmacokinetics in the development of new pharmacotherapies, CM304 (sigma-1 receptor antagonist), mitragynine and 7-hydroxymitragynine (µ-opioid receptor agonists), for the treatment of drug abuse. -
Alpha^ and Beta^Blocking Agents: Pharmacology and Properties
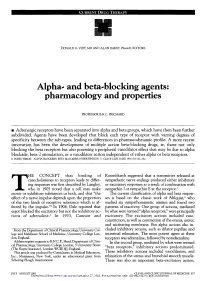
CURRENT DRUG THERAPY DONALD G. VIDT, MD AND ALAN BAKST, PharmD, EDITORS Alpha^ and beta^blocking agents: pharmacology and properties PROFESSOR B.N.C. PRICHARD • Adrenergic receptors have been separated into alpha and beta groups, which have then been further subdivided. Agents have been developed that block each type of receptor with varying degrees of specificity between the sub-types, leading to differences in pharmacodynamic profile. A more recent innovation has been the development of multiple action beta-blocking drugs, ie, those not only blocking the beta receptors but also posessing a peripheral vasodilator effect that may be due to alpha blockade, beta-2 stimulation, or a vasodilator action independent of either alpha or beta receptors. • INDEX TERMS: ALPHA BLOCKERS; BETA BLOCKERS; HYPERTENSION • CLEVE CLIN ] MED 1991; 58:33 7-350 HE CONCEPT that binding of Rosenblueth suggested that a transmitter released at catecholamines to receptors leads to differ- sympathetic nerve endings produced either inhibitory ing responses was first described by Langley, or excitatory responses as a result of combination with who in 1905 noted that a cell may make sympathin I or sympathin E at the receptor.3 Tmotor or inhibitory substances or both, and that "the The current classification of alpha and beta respon- effect of a nerve impulse depends upon the proportion ses is based on the classic work of Ahlquist,4 who of the two kinds of receptive substance which is af- studied six sympathomimetic amines and found two fected by the impulse."1 In 1906, Dale reported that patterns of reactivity. One group of actions, mediated ergot blocked the excitatory but not the inhibitory ac- by what were termed "alpha receptors," were principally tions of adrenaline.2 In 1933, Cannon and excitatory. -

Original Article Effect of GABA on Blood Pressure and Blood Dynamics of Anesthetic Rats
Int J Clin Exp Med 2015;8(8):14296-14302 www.ijcem.com /ISSN:1940-5901/IJCEM0008622 Original Article Effect of GABA on blood pressure and blood dynamics of anesthetic rats Pengju Ma1, Ting Li2, Fanceng Ji3, Haibo Wang4, Juntao Pang4 1Department of Anesthesiogy, Anqiu People’s Hospital, Anqiu 262100, China; 2Delivery Room, People’s Hospital of Anqiu, Anqiu 262100, China; 3Department of Anesthesiogy, Weifang People’s Hospital, Weifang 261041, China; 4Department of Critical Care Medicine of Weifang People’s Hospital, Weifang 261041, China Received March 31, 2015; Accepted August 13, 2015; Epub August 15, 2015; Published August 30, 2015 Abstract: Background: This study aimed to investigate GABA effects on blood pressure and blood dynamics of an- esthetic rats by observing spontaneously hypertensive rats under both anesthesia and waking state. Materials and methods: 72 male waking Wistar-Kyokos (WKY) rats and 72 male anesthetized spontaneously hypertensive (SHR) rats were randomly divided into control group and experimental group (N = 36 each). Rats were further divided into three subgroups (N = 12 each), which received 15 μmol GABA, 35 nmol muscimol, or 4 nmol dicentrine into uni- lateral paraventricular nucleus, respectively. Rats in the control group (WKY1) and experimental group (SHR1) were compared for the GABA effect on blood pressure (MAP), heart rate (HR), and arterial baroreceptor reflex function (BRS) changes under waking state. Anesthetic WKY rats (WKY2) and spontaneously hypertensive rats (SHR2) were compared for the GABA effect on those abovementioned indexes. Abdominal aorta mean arterial pressure, heart rate, and arterial baroreceptor reflex function changes were compared in all rats. Results: MAP, HR, and BRS were slightly lower in the rats under anesthetic state than in waking state before treatment (P < 0.05); they did not show significant changes between anesthetic and waking state, however, after treatment (P > 0.05). -

United States Patent (19) (11) 4,310,524 Wiech Et Al
United States Patent (19) (11) 4,310,524 Wiech et al. 45 Jan. 12, 1982 (54) TCA COMPOSITION AND METHOD FOR McMillen et al., Fed. Proc., 38,592 (1979). RAPD ONSET ANTDEPRESSANT Sellinger et al., Fed. Proc., 38,592 (1979). THERAPY Pandey et al., Fed. Proc., 38,592 (1979). 75) Inventors: Norbert L. Wiech; Richard C. Ursillo, Primary Examiner-Stanley J. Friedman both of Cincinnati, Ohio Attorney, Agent, or Firm-Millen & White 73) Assignee: Richardson-Merrell, Inc., Wilton, Conn. (57 ABSTRACT A method is provided for treating depression in a pa (21) Appl. No.: 139,498 tient therefrom and requiring rapid symptomatic relief, (22 Filed: Apr. 11, 1980 which comprises administering to said patient concur 51) Int. Cl. .................... A61K 31/33; A61K 31/135 rently (a) an effective antidepressant amount of a tricy clic antidepressant or a pharmaceutically effective acid (52) ...... 424/244; 424/330 addition salt thereof, and (b) an amount of an a-adrener 58) Field of Search ................................ 424/244, 330 gic receptor blocking agent effective to achieve rapid (56) References Cited onset of the antidepressant action of (a), whereby the PUBLICATIONS onset of said antidepressant action is achieved within Chemical Abst., vol. 66-72828m, (1967), Kellett. from 1 to 7 days. Chemical Abst, vol. 68-94371a, (1968), Martelli et al. A pharmaceutical composition is also provided which is Chemical Abst., vol. 74-86.048j, (1971), Dixit et al. especially adapted for use with the foregoing method. Holmberg et al., Psychopharm., 2,93 (1961). Svensson, Symp. Med. Hoechst., 13, 245 (1978). 17 Claims, No Drawings 4,310,524 1. -

(12) United States Patent (10) Patent No.: US 8,980,319 B2 Park Et Al
US00898O319B2 (12) United States Patent (10) Patent No.: US 8,980,319 B2 Park et al. (45) Date of Patent: *Mar. 17, 2015 (54) METHODS OF PRODUCING STABILIZED A613 L/445 (2006.01) SOLID DOSAGE PHARMACEUTICAL A613 L/47 (2006.01) COMPOSITIONS CONTAINING A6II 45/06 (2006.01) MORPHINANS A63/67 (2006.01) (52) U.S. Cl. (71) Applicant: Mallinckrodt LLC, Hazelwood, MO CPC ............. A6 IK3I/485 (2013.01); A61 K9/1652 (US) (2013.01); A61 K9/2031 (2013.01); A61 K 9/2081 (2013.01); A61 K9/2086 (2013.01); (72) Inventors: Jae Han Park, Olivette, MO (US); A6IK9/2095 (2013.01); A61 K9/5042 Tiffani Eisenhauer, Columbia, IL (US); (2013.01); A61 K3I/4355 (2013.01); A61 K Spainty,S.Isna Gupta, F11llsborough, 31/4375A6 (2013.01); IK3I/445 gets (2013.01); it' A6 (2013.01); IK3I/47 Stephen Overholt, Middlesex, NJ (US) (2013.01); A61K 45/06 (2013.01); A61 K 9/2013 (2013.01); A61 K9/209 (2013.01); (73) Assignee: Mallinckrodt LLC, Hazelwood, MO A6 IK3I/167 (2013.01) (US) USPC ........... 424/472: 424/465; 424/468; 424/490; c - r - 514/282; 514/289 (*) Notice: Subject to any disclaimer, the term of this (58) Field of Classification Search patent is extended or adjusted under 35 N U.S.C. 154(b)b) by 0 daysyS. Seeone application file for complete search history. This patent is Subject to a terminal dis claimer. (56) References Cited (21) Appl. No.: 14/092.375 U.S. PATENT DOCUMENTS (22) Filed: Nov. 27, 2013 2008, 0026052 A1 ck 1/2008 Schoenhard ................. -

EVALUATION of ACETYLCHOLINESTERASE INHIBITORY ACTIVITY and MODULATORY EFFECT on NICOTINIC ACETYLCHOLINE RECEPTORS of ALKALOIDS ISOLATED from Rhodolirium Andicola
UNIVERSIDAD DE LA FRONTERA Facultad de Ingeniería y Ciencias Doctorado en Ciencias de Recursos Naturales EVALUATION OF ACETYLCHOLINESTERASE INHIBITORY ACTIVITY AND MODULATORY EFFECT ON NICOTINIC ACETYLCHOLINE RECEPTORS OF ALKALOIDS ISOLATED FROM Rhodolirium andicola DOCTORAL THESIS IN FULFILLMENT OF THE REQUERIMENTS FOR THE DEGREE DOCTOR OF SCIENCES IN NATURAL RESOURCES FELIPE EDUARDO MORAGA NICOLÁS TEMUCO-CHILE 2018 Evaluation of acetylcholinesterase inhibitory activity and modulatory effect on nicotinic acetylcholine receptors of alkaloids isolated from Rhodolirium andicola Esta tesis fue realizada bajo la supervisión del director de Tesis Dra. ANA MUTIS TEJOS, y bajo la co-tutela del Dr. EMILIO HORMAZÁBAL URIBE, pertenecientes al Departamento de Ciencias Químicas y Recursos Naturales de la Universidad de La Frontera, y es presentada para su revisión por los miembros de la comisión examinadora. FELIPE EDUARDO MORAGA NICOLÁS Dr. Andrés Quiroz Director programa de Doctorado en Dra. Ana Mutis T. Ciencias de Recursos Naturales Dr. Emilio Hormazábal U. Dr. Patricio Iturriaga V. Dra. Mónica Rubilar Directora Académica de Postgrado Universidad de La Frontera Dr. Andrés Quiroz C. Dr. Alejandro Urzúa M. Dr. Leonardo Guzmán G. Dedico esta tesis a mi Madre por su apoyo amor y confianza Agradecimientos/Acknowledgments Este escrito no solo refleja los resultados de una investigación, sino también, interés y aprecio por los productos naturales. El desarrollo de este trabajo no habría sido posible sin el apoyo de todas aquellas personas, que directa o indirectamente, me han permitido llevar a cabo los objetivos propuestos en esta investigación. De este modo, las siguientes líneas expresan mis agradecimientos más sinceros a quienes colaboraron en hacer esto una realidad. -

The Search for the "Manchurian Candidate" the Cia and Mind Control
THE SEARCH FOR THE "MANCHURIAN CANDIDATE" THE CIA AND MIND CONTROL John Marks Allen Lane Allen Lane Penguin Books Ltd 17 Grosvenor Gardens London SW1 OBD First published in the U.S.A. by Times Books, a division of Quadrangle/The New York Times Book Co., Inc., and simultaneously in Canada by Fitzhenry & Whiteside Ltd, 1979 First published in Great Britain by Allen Lane 1979 Copyright <£> John Marks, 1979 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner ISBN 07139 12790 jj Printed in Great Britain by f Thomson Litho Ltd, East Kilbride, Scotland J For Barbara and Daniel AUTHOR'S NOTE This book has grown out of the 16,000 pages of documents that the CIA released to me under the Freedom of Information Act. Without these documents, the best investigative reporting in the world could not have produced a book, and the secrets of CIA mind-control work would have remained buried forever, as the men who knew them had always intended. From the documentary base, I was able to expand my knowledge through interviews and readings in the behavioral sciences. Neverthe- less, the final result is not the whole story of the CIA's attack on the mind. Only a few insiders could have written that, and they choose to remain silent. I have done the best I can to make the book as accurate as possible, but I have been hampered by the refusal of most of the principal characters to be interviewed and by the CIA's destruction in 1973 of many of the key docu- ments. -

Review Article Natural Product-Derived Treatments for Attention-Deficit/Hyperactivity Disorder: Safety, Efficacy, and Therapeutic Potential of Combination Therapy
Hindawi Publishing Corporation Neural Plasticity Volume 2016, Article ID 1320423, 18 pages http://dx.doi.org/10.1155/2016/1320423 Review Article Natural Product-Derived Treatments for Attention-Deficit/Hyperactivity Disorder: Safety, Efficacy, and Therapeutic Potential of Combination Therapy James Ahn,1 Hyung Seok Ahn,2 Jae Hoon Cheong,3 and Ike dela Peña1 1 Department of Pharmaceutical and Administrative Sciences, Loma Linda University, Loma Linda, CA 92350, USA 2School of Medicine, Chungnam National University, Daejeon 301-747, Republic of Korea 3Department of Pharmacy, Sahmyook University, Seoul 139-742, Republic of Korea Correspondence should be addressed to Ike dela Pena;˜ [email protected] Received 9 November 2015; Revised 30 December 2015; Accepted 10 January 2016 Academic Editor: Daniel Fung Copyright © 2016 James Ahn et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Typical treatment plans for attention-deficit/hyperactivity disorder (ADHD) utilize nonpharmacological (behavioral/psychosocial) and/or pharmacological interventions. Limited accessibility to behavioral therapies and concerns over adverse effects of pharmacological treatments prompted research for alternative ADHD therapies such as natural product-derived treatments and nutritional supplements. In this study, we reviewed the herbal preparations and nutritional supplements evaluated in clinical studies as potential ADHD treatments and discussed their performance with regard to safety and efficacy in clinical trials. We also discussed some evidence suggesting that adjunct treatment of these agents (with another botanical agent or pharmacological ADHD treatments) may be a promising approach to treat ADHD. -

Dicentrine Production from a Hairy Roots Culture of Stephania Suberosa
Dicentrine Production from a Hairy Roots Culture of Stephania suberosa Waraporn Putalun*, Gorawit Yusakul, and Denpong Patanasethanont Faculty of Pharmaceutical Sciences, Khon Kaen University, Khon Kaen, 40002, Thailand. Fax: +66-43-2 02-3 79. E-mail: [email protected] * Author for correspondence and reprint requests Z. Naturforsch. 64 c, 692 – 696 (2009); received June 8/July 2, 2009 A hairy roots culture of Stephania suberosa was established using Agrobacterium rhizo- genes ATCC15834. The production of dicentrine was found to be (8.92 ± 0.07) mg/g dry wt on day 35 of culture. Effects of sucrose content, tyrosine, and medium strength on growth and dicentrine production of S. suberosa were investigated. 6% (w/v) sucrose was an op- timum content for the growth and dicentrine accumulation in S. suberosa hairy roots. The utilization of a precursor from tyrosine feeding enhanced the dicentrine production. The medium with 1.0 mM of tyrosine had the highest effect on dicentrine accumulation in hairy roots at day 40 of culture [(14.73 ± 0.47) mg/g dry wt]. In addition, ¼ Murashige and Skoog medium was suitable for biomass and dicentrine production in hairy roots. This culture sys- tem has a potential to produce dicentrine from hairy roots of S. suberosa. Key words: Dicentrine, Hairy Roots, Stephania suberosa Introduction achieved in S. suberosa tuberous roots (Patra et al., 1986; Sriprang et al., 2006). Therefore, hairy Stephania suberosa Forman (Menispermaceae) roots cultures of S. suberosa are necessary for the is a medicinal plant which has been used in Thai production of biological compounds. It is known traditional medicine for the treatment of hyper- that many factors could affect the secondary me- tension. -

Review Article Natural Compounds for the Management of Parkinson's
Hindawi BioMed Research International Volume 2018, Article ID 4067597, 12 pages https://doi.org/10.1155/2018/4067597 Review Article Natural Compounds for the Management of Parkinson’s Disease and Attention-Deficit/Hyperactivity Disorder Juan Carlos Corona Laboratory of Neurosciences, Hospital Infantil de Mexico´ Federico Gomez,´ Mexico Correspondence should be addressed to Juan Carlos Corona; [email protected] Received 28 June 2018; Revised 31 October 2018; Accepted 11 November 2018; Published 22 November 2018 Guest Editor: Francesco Facchiano Copyright © 2018 Juan Carlos Corona. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Parkinson’s disease (PD) is the second most common neurodegenerative disorder with an unknown aetiology. Te pathogenic mechanisms include oxidative stress, mitochondrial dysfunction, protein dysfunction, infammation, autophagy, apoptosis, and abnormal deposition of �-synuclein. Currently, the existing pharmacological treatments for PD cannot improve fundamentally the degenerative process of dopaminergic neurons and have numerous side efects. On the other hand, attention-defcit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder of childhood and is characterised by hyperactivity, impulsiv- ity, and inattention. Te aetiology of ADHD remains unknown, although it has been suggested that its pathophysiology involves abnormalities in several brain regions, disturbances of the catecholaminergic pathway, and oxidative stress. Psychostimulants and nonpsychostimulants are the drugs prescribed for the treatment of ADHD; however, they have been associated with increased risk of substance use and have several side efects. Today, there are very few tools available to prevent or to counteract the progression of such neurological disorders. -

Poisonous Properties of Bikukulla Cuculla- Ria (Dutchman's-Breeches) and B
POISONOUS PROPERTIES OF BIKUKULLA CUCULLA- RIA (DUTCHMAN'S-BREECHES) AND B. CANADENSIS (SQUIRREL-CORN)1 By O. F. BivACK, Chemical Biologist, W. W. EGGLESTON, Assistant Botanist, and J. W. K^LLY, Chemical Laboratorian, Office of Drug, Poisonous, and Oil Plant Investigations, Bureau of Plant Industry, United States Department of Agriculture, and H. C. TURNER, Assistant Animal Husbandman, Virginia Agricultural Experiment Station INTRODUCTION Since the time of the early settlements in the mountains of Virginia frequent fatal cases of poisoning have occurred among cattle grazing in the mountain pastures in early spring. It has long been believed that certain early spring plants popularly known as <<staggerweeds,, have been the cause of these fatalities, since these plants are among the first to appear in the pastures and are often eaten by cattle when other forage is not abundant. Suspicion has chiefly centered upon the plants com- monly called larkspur (Delphinium tricorne Michx.), dutchman's-breeches (Bikukulla cucullaria (L.) Millsp.)> squirrel-corn (B. canadensis (Goldie) Millsp.), and wild bleeding heart (B. eximia (Ker) Millsp.). In the literature relating to poisonous plants the toxic character of D. tricorne has long been recognized, but the American species of Bikukulla appear to have received comparatively little attention from chemists and prac- tically none from toxicologists. The probable poisonous character of species of Bikukulla was first brought to the attention of the Department of Agriculture in June, 1920, by Prof. H. S. Stahl, of the Virginia Polytechnic Institute. He sub- mitted specimens of "little staggerweed," later identified as Bikukulla cucullaria y with the statement that this plant was believed to be respon- sible for the recent death of a number of cattle in the mountain pastures of Bland County, Va.