An-Re-Patel Chest-2015-16 Annual Report.Pmd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
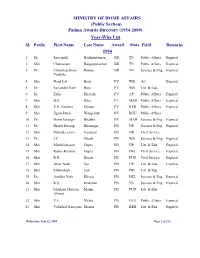
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -

Autar Singh Paintal (1925–2004)
Indian J Physiol Pharmacol 2005; 49 (2) : 247–250 OBITUARY Autar Singh Paintal (1925–2004) What can I say that can change your lives? Perhaps I should ask you to do something that is very difficult. And so I am going to ask you to try to achieve perfection in your chosen areas of activity. (A.S. Paintal at the Institute Convocation of Delhi University of Technology, 1993) Professor Autar S. Paintal - an internationally acclaimed scientist in the area of cardio-respiratory physiology - died on December 21, 2004. He was born on September 24, 1925 in Mogok, Myanmar, where his father Dr. Man Singh was a physician in the service of the British Medical Service and possessed a strong socialist outlook, while Autar’s mother Rajwans Kaur was a deeply religious lady. Autar’s own life thus came to be moulded by both these systems of belief. At the age of 14, he was sent to Lahore to finish his matriculation, ahead of the evacuation of the family from Burma. Here, besides studying hard and starting on his inexhaustible fund of limericks that he subsequently became famous for, he learnt to row the large country boats that plied on the river Raavi. He stayed on at the Forman Christian College to write the Intermediate Examination of the Panjab University and after that he joined his family in Lucknow where his father chose to settle down. Admission into Medical College in 1943 was an easy matter for him but he needed financial support. Fortunately for him, he still held the status of a ‘Burma Evacuee’ and the Burmese Government came to his support. -

FAMILY LAW of Muslims, Parsis and Christians of India (Mumbai University Academic Council Accepted ‘Administrative Law’ by Mr
FAMILY LAW of Muslims, Parsis and Christians of India (Mumbai University Academic Council accepted ‘Administrative Law’ by Mr. I.A. Saiyed as Reference – Book for LL.B. Degree Course on recommendations of Board of Studies in Law – See Circular No. UG/214 of 2011 of University of Mumbai.) By I.A. SAIYED Advocate, Notary and Law Professor Foreword by ISO 9001:2015 CERTIFIED © AUTHOR No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording and/or otherwise without the prior written permission of the author and the publisher. First Edition : 1991 Reprint : 2001 Second Revised Edition : 2004 Reprint : 2006, 2008 Third Revised Edition : 2010 Reprint : 2015, 2016, 2017 Fourth Revised Edition : 2019 Published by : Mrs. Meena Pandey for Himalaya Publishing House Pvt. Ltd., Ramdoot, Dr. Bhalerao Marg, Girgaon, Mumbai - 400 004 Phone: 022-23860170/23863863; Fax: 022-23877178 E-mail: [email protected]; Website: www.himpub.com Branch Offices : New Delhi : Pooja Apartments, 4-B, Murari Lal Street, Ansari Road, Darya Ganj, New Delhi - 110 002. Phone: 011-23270392, 23278631; Fax: 011-23256286 Nagpur : Kundanlal Chandak Industrial Estate, Ghat Road, Nagpur - 440 018. Phone: 0712-2738731, 3296733; Telefax: 0712-2721216 Bengaluru : Plot No. 91-33, 2nd Main Road, Seshadripuram, Behind Nataraja Theatre, Bengaluru - 560 020. Phone: 080-41138821; Mobile: 09379847017, 09379847005 Hyderabad : No. 3-4-184, Lingampally, Besides Raghavendra Swamy Matham, Kachiguda, Hyderabad - 500 027. Phone: 040-27560041, 27550139 Chennai : New No. 48/2, Old No. 28/2, Ground Floor, Sarangapani Street, T. Nagar, Chennai-600 012. -

SRNO FOLIO NO NAME Shares As on March 31, 2017 1 0000019 K VISWANATHAN 20 2 0000231 BHARAT MULCHAND CHOKSEY 212 3 0000234 PRAN K
GOODYEAR INDIA LIMITED Registered Office: Mathura Road, Ballabgarh (Dist. Faridabad) - 121 004, Haryana, Corporate Office: 1st Floor, ABW Elegance Tower, Plot no. 8, Commercial Centre Jasola – 110 025, New Delhi, India CIN: L25111HR1961PLC008578 Email – [email protected],Website –www.goodyear.co.in Details of Shareholders and Equity Shares due for transfer to IEPF Suspense Account in respect of which Dividends have been unpaid/unclaimed since financial year ended December 31, 2008 Shares as on SRNO FOLIO_NO NAME March 31, 2017 1 0000019 K VISWANATHAN 20 2 0000231 BHARAT MULCHAND CHOKSEY 212 3 0000234 PRAN KRISHANA MUKHERJEE 20 4 0000258 ULLAL VARADARAJA NAYAK 64 5 0000271 SACHINDRA NATH BASU 578 6 0000490 RAJENDRA KISHORE BAIJAL 2 7 0000623 KUNDAN LAL KOHLI 318 8 0000702 JAGDISH PRASHAD PANNALAL AND CO PVT LTD 190 9 0000716 CLIVE STREET NOMINEES PVT LTD 176 10 0000750 MOTI LOKUMAL JHANGIANI 70 11 0000759 BANTVAL SIVA RAO 560 12 0000800 MOHINDRA NATH 145 13 0000829 MOHAN LAL LATH 36 14 0000916 AMAR KRISHNA PODDER 26 15 0001010 PRAPHULLA KUMAR SEN 286 16 0001059 SOHAN LAL BERRY 2 17 0001091 SITA BHAGAT 10 18 0001106 SATYA PAL 22 19 0001218 BABOO HAYATH SAHAB 140 20 0001260 JETHALAL GOKALDAS UDESHI 9 21 0001273 SURATH CHANDRA ROY 72 22 0001274 VIDYA PRAKASH SARNA 78 23 0001297 KISHORI LAL AGARWALA 56 24 0001319 NIHAL DEVI AHUJA 8 25 0001349 HIRA LAL ARORA 56 26 0001351 ROSHAN LAL ARORA 28 27 0001358 JANAK AWASTI 46 28 0001359 GULAMALI MOHMED BABVANI 18 29 0001369 NANAK CHAND RAI BAHADUR 144 30 0001454 SATHANALA BHULOKAMU -

Patron-In-Chief Honorary Fellows Founder Fellows
Patron-in-Chief 1. Dr. Rajendra Prasad 2. Dr. S. Radhakrishnan 3. Dr. Zakir Husain 4. Shri V.V. Giri 5. Shri Fakhruddin Ali Ahmed 6. Shri Giani Zail Singh Honorary Fellows 1. Shri Jawahar Lal Nehru 2. Dr. B.C. Roy 3. Major Genl. S.L. Bhatia 4. Col. R.N. Chopra 5. Dr. H.M. Lazarus 6. Dr. Jivaraj N. Mehta 7. Dr. A. Lakshamanswami Mudaliar 8. Dr. N.A. Purandare 9. Major Genl. S.S. Sokey 10. Dr. A.C. Ukil 11. Dr. Sushila Nayar 12. Smt. Indira Gandhi 13. Dr. V.T.H. Gunaratne 14. Dr. Dharmendra 15. Shri P.V. Narasimha Rao Founder Fellows 1. Dr. Madan Lal Aggarwal 2. Dr. B.K. Aikat 3. Dr. S.T. Achar 4. Dr. (Col.) Amir Chand 5. Dr. A.A. Ayer 6. Dr. Santokh Singh Anand 7. Dr. R.B. Arora 8. Dr. L.H. Athle 9. Dr. A.V. Baliga 10. Dr. Baldev Singh 11. Dr. Bankat Chandra 12. Dr. A.K. Basu 13. Dr. B.B. Bhatia 14. Dr. T.N. Banerjee 15. Dr. Bimal Chandra Bose 16. Dr. J.C. Banerjee 17. Dr. E.J. Borges 18. Dr. P.V. Cherian 19. Dr. R.N. Chaudhuri 20. Dr. G. Coelho 21. Dr. R.A.F. Cooper 22. Dr. (Lt.Genl.) D.N. Chakravarti 23. Dr. L.W. Chacko 24. Dr. M.K.K. Menon 25. Dr. Subodh Mitra 26. Dr. (Capt) P.B. Mukherjee 27. Dr. S.R. Mukherjee 28. Dr. B. Mukhopadhaya 29. Dr. M. Naidu 30. Dr. B. Narayana 31. Dr. C.G. -

Indian Council of Medical Research New Delhi © 2005 Indian Council of Medical Research
Annual Report 2003-2004 Indian Council of Medical Research New Delhi © 2005 Indian Council of Medical Research Prof. N.K. Ganguly: Director-General Dr. K. Satyanarayana: Chief (Publication & Information) Complied and Edited by Dr. Sudha Chauhan, DDG (SG) Published by the Division of Publication, Information and Communication on behalf of the Director-General, Indian Council of Medical Research New Delhi 110029 Layout Design & Production Control by ICMR Press Unit Printed at: S. Narayan & Sons, B-88, Okhla Indl. Area, Phase-II, New Delhi Tel: 26385873 he Indian Council of Medical Research has made significant strides in its mandate of ‘Research for TBetter Health’. The Council has lived up to country’s expectations on all major fronts of its activity: research and development of vaccines and drugs for infectious diseases like tuberculosis, malaria, filariasis, HIV/AIDS, research in the areas of modern biology like molecular biology, genomics, bioinformatics, fertility regulation, cancer and other non-communicable diseases, consultancy and human resource development, national and international collaborations and biomedical informatics and communication. During the period under report, the Memorandum for the Expenditure Finance Committee (EFC) of ICMR has been approved by the Government of India and Rs.870 Crores have been allocated for the 10th Plan. The research activities will now be pursued with greater vigour as more funding would be available. To optimize resource utilization, the Council is using the Combined Approach Matrix being used by Global Health Forum for Health Research for setting research priorities in various disciplines. The Council continued to play an important role in detecting new and emerging infections in India like the Chandipura virus encephalitis in Andhra Pradesh and Gujarat and outbreak of mysterious fever in Siliguri. -

Bright Sparks
I NDIAN response. This was known as the Paintal Index and was used by clinicians in the early days. He continued in his alma mater and later became a lecturer in the N Department of Physiology. A TIONAL Later he received a Rockefeller Scholarship to pursue PhD from the Medical A. S. Paintal School in Edinburgh. Here he conceptualised the discovery of J-receptors. At S that time it was difficult to dissect single nerve fibres without impairing their (1925 – 2004) CIENCE activity. He found an innovative method of dipping the whole nerve in liquid paraffin to embed the whole nerve and isolate the single fibres without impairing their activity. This gave a tremendous boost to research in this area. A CADEMY In 1953 he returned to India and joined the Defence Laboratory in Kanpur. After five years he moved to the All India Institute of Medical Sciences (AIIMS), Autar Singh Paintal was perhaps India’s best known physiologist. He was a New Delhi as a researcher in Physiology. Six years later he became the Director prodigious researcher with a very colourful and uncompromising personality. INSA of the V. P. Chest Hospital a post he held till 1990. Later even when he became Paintal was born on 24 September 1925 in Mogok, Burma where his father the Director General of the Indian Council of Medical Research (ICMR) he worked in the British Medical Service. He completed his Matriculation from PLA still continued his research at his modest two-room laboratory at the V.P. Chest Institute. Lahore at the age of fourteen and later joined the Forman Christian College TINUM JUBILEE for his Intermediate. -

Padma Vibhushan * * the Padma Vibhushan Is the Second-Highest Civilian Award of the Republic of India , Proceeded by Bharat Ratna and Followed by Padma Bhushan
TRY -- TRUE -- TRUST NUMBER ONE SITE FOR COMPETITIVE EXAM SELF LEARNING AT ANY TIME ANY WHERE * * Padma Vibhushan * * The Padma Vibhushan is the second-highest civilian award of the Republic of India , proceeded by Bharat Ratna and followed by Padma Bhushan . Instituted on 2 January 1954, the award is given for "exceptional and distinguished service", without distinction of race, occupation & position. Year Recipient Field State / Country Satyendra Nath Bose Literature & Education West Bengal Nandalal Bose Arts West Bengal Zakir Husain Public Affairs Andhra Pradesh 1954 Balasaheb Gangadhar Kher Public Affairs Maharashtra V. K. Krishna Menon Public Affairs Kerala Jigme Dorji Wangchuck Public Affairs Bhutan Dhondo Keshav Karve Literature & Education Maharashtra 1955 J. R. D. Tata Trade & Industry Maharashtra Fazal Ali Public Affairs Bihar 1956 Jankibai Bajaj Social Work Madhya Pradesh Chandulal Madhavlal Trivedi Public Affairs Madhya Pradesh Ghanshyam Das Birla Trade & Industry Rajashtan 1957 Sri Prakasa Public Affairs Andhra Pradesh M. C. Setalvad Public Affairs Maharashtra John Mathai Literature & Education Kerala 1959 Gaganvihari Lallubhai Mehta Social Work Maharashtra Radhabinod Pal Public Affairs West Bengal 1960 Naryana Raghvan Pillai Public Affairs Tamil Nadu H. V. R. Iyengar Civil Service Tamil Nadu 1962 Padmaja Naidu Public Affairs Andhra Pradesh Vijaya Lakshmi Pandit Civil Service Uttar Pradesh A. Lakshmanaswami Mudaliar Medicine Tamil Nadu 1963 Hari Vinayak Pataskar Public Affairs Maharashtra Suniti Kumar Chatterji Literature -

Newsaugust2005.Pdf
Editor Co-Editor Dr. P.N. Tiwari Dr. G. Govil Ex-Project Director, NRL, Ex-Senior Prof. & Dean (Physics) IARI, New Delhi Tata Instt. of Fundamental Research Block B-65, SFS Qrts., Homi Bhabha Road, Nebi Nagar, Sheikh Sarai, Phase - I, Mumbai-400 005 New Delhi - 110 017 Ph.: 022-26301816 Tel.: 011-26012615 E-mail: [email protected] Associate Editors Dr. P.S. Datta Dr. Indra Mani Project Director & Professor Senior Scientist Nuclear Research Laboratory Divn. of Agricultural Engineering IARI, New Delhi - 110012 IARI, New Delhi - 110012 Email: [email protected] Email: [email protected] Editorial Advisory Committee Dr. A.R. Verma (New Delhi) Dr. P.N. Srivastava (Gurgaon) Dr. P.M. Bhargava (Hyderabad) Dr. (Mrs.) Indira Nath (New Delhi) Dr. S.R. Valluri (Bangalore) Office Bearers of the Society (August 1, 2005 - July 31, 2008) President Vice President Secretary Dr. K.L. Chopra Dr. Vikram Kumar Dr. Nandula Raghuram (Ex-Director, IIT Kharagpur) Director, National School of Biotechnology, M-70, Kirti Nagar Physical Laboratory GGS Indraprastha University, New Delhi-110 015 K.S. Krishnan Marg, Kashmiri Gate, Delhi -110006 Ph: (011) 25154114 New Delhi-110012 Ph: (011) 26112065 Email: [email protected] Joint Secretary Treasurer Dr. Ashima Anand Dr. Indra Mani Principal Scientific Officer Senior Scientist DST Centrefor Visceral Divn. of Agricultural Enginering Mechanisms, V.P. Chest IARI, New Delhi-110 012 Institute, New Delhi-110 007 E-mail : [email protected] Ph: (011) 27667749 Email: [email protected] Main objectives of the 'Society for Scientific Values 1. To promote objectivity, integrity and ethical values in pursuit of scientific research, education and management, and 2. -

General Kofi A. Annan the United Nations United Nations Plaza
MASSACHUSETTS INSTITUTE OF TECHNOLOGY DEPARTMENT OF PHYSICS CAMBRIDGE, MASSACHUSETTS O2 1 39 October 10, 1997 HENRY W. KENDALL ROOM 2.4-51 4 (617) 253-7584 JULIUS A. STRATTON PROFESSOR OF PHYSICS Secretary- General Kofi A. Annan The United Nations United Nations Plaza . ..\ U New York City NY Dear Mr. Secretary-General: I have received your letter of October 1 , which you sent to me and my fellow Nobel laureates, inquiring whetHeTrwould, from time to time, provide advice and ideas so as to aid your organization in becoming more effective and responsive in its global tasks. I am grateful to be asked to support you and the United Nations for the contributions you can make to resolving the problems that now face the world are great ones. I would be pleased to help in whatever ways that I can. ~~ I have been involved in many of the issues that you deal with for many years, both as Chairman of the Union of Concerne., Scientists and, more recently, as an advisor to the World Bank. On several occasions I have participated in or initiated activities that brought together numbers of Nobel laureates to lend their voices in support of important international changes. -* . I include several examples of such activities: copies of documents, stemming from the . r work, that set out our views. I initiated the World Bank and the Union of Concerned Scientists' examples but responded to President Clinton's Round Table initiative. Again, my appreciation for your request;' I look forward to opportunities to contribute usefully. Sincerely yours ; Henry; W. -

Indian Contribution in Medical Science – Modern Medicine (Part 2)
Journal of The West Bengal University of Health Sciences January 2021 Vol 1 Issue 3 EDITORIAL Indian Contribution in Medical Science – Modern Medicine (Part 2) Manidip Pal Continued from previous issue. Chronology Arthur Saravanamuthu Thambiah has been maintained according to the birth (1924-2011) is fondly called as Father of year of the legends. Dermatology practice in India.45 His renowned papers included the first Asian case of Lipoid Hattangadi Shashidhar Bhat (1921-2010) Proteinosis (1963) and the first world report is considered as doyen of Urology in India.41 of Cystic changes in the bones of Darier’s He was a visionary, teacher and surgeon disease (1969). He was recipient of Dr. B.C. extraordinary. In India he was first surgeon Roy National Award under the category of to exploit bladder flaps, intestine, Teflon and Eminent Medical Teacher in 1978.46 penile prosthesis in reconstructive urology.42 He took on the mantle of starting urology Darab Kersasp Dastur (1924-2000) and department at CMC, Vellore, nurturing it Autar Singh Paintal (1925-2004) are named and made it grow. HOD of Surgery from as Founder of Indian neuroscience. Darab other institutions came to CMC to get trained Kersasp Dastur, had pivotal work on brain under him in Urology so as to set up their tumours and muscle disease. His research urology department in their institutes.41 work had contributed to the development of neuro-tuberculosis, neuro-oncology, Har Gobind Khorana (1922-2011) developmental disorders of the nervous won the Nobel Prize in Physiology or system and pathology of protein calorie Medicine (1968) alongwith Robert W. -
Bright Sparks Introduction.P65
BRIGHT SPARKS INSPIRING INDIAN SCIENTISTS FROM THE PAST by Arvind Gupta illustrated by Karen Haydock CONTENTS A. Cursetjee ........................................... 1 Nain Singh Rawat ................................. 6 J. C. Bose ............................................ 10 P. C. Ray ............................................... 14 Ruchi Ram Sahni ................................ 18 D. N. Wadia ......................................... 22 S. Ramanujan ...................................... 26 C. V. Raman ........................................ 30 S. K. Mitra ........................................... 35 Birbal Sahni ......................................... 39 J. B. S. Haldane ................................... 44 P. C. Mahalanobis ............................... 49 M. N. Saha ........................................... 53 S. N. Bose ............................................ 57 S. S. Bhatnagar .................................... 61 Yellapragada SubbaRow .................... 65 Salim Ali .............................................. 69 K. S. Krishnan .................................... 74 V. N. Shirodkar ................................... 78 T. R. Seshadri ...................................... 82 P. Maheshwari ..................................... 86 Irawati Karve ...................................... 90 B. P. Pal ................................................ 94 D. D. Kosambi ................................... 98 Homi Bhabha ................................... 103 Subrahmanian Chandrasekhar........ 107 Vikram Sarabhai