Chronic Obstructive Pulmonary Disease (2018 Report)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trends in COPD (Chronic Bronchitis and Emphysema): Morbidity and Mortality
Trends in COPD (Chronic Bronchitis and Emphysema): Morbidity and Mortality Please note, this report is designed for double-sided printing American Lung Association Epidemiology and Statistics Unit Research and Health Education Division March 2013 Page intentionally left blank Table of Contents COPD Mortality, 1999-2009 COPD Prevalence, 1999-2011 COPD Hospital Discharges, 1999-2010 Glossary and References List of Tables Table 1: COPD – Number of Deaths by Ethnic Origin and Sex, 1999-2009 Figure 1: COPD – Number of Deaths by Sex, 1999-2009 Figure 2: COPD – Age-Adjusted Death Rates by Ethnic Origin and Sex, 2009 Table 2: COPD – Age-Adjusted Death Rate per 100,000 Population by Ethnic Origin and Sex, 1999- 2009 Figure 3: COPD – Deaths and Age-Adjusted Death Rate by Sex, 2009 Figure 4: COPD – Diagnosed Cases and Evidence of Impaired Lung Function Figure 5: Chronic Bronchitis – Prevalence Rates per 1,000, 2011 Table 3: Chronic Bronchitis – Number of Conditions and Prevalence Rate per 1,000 Population by Ethnic Origin, Sex and Age, 1999-2011 Figure 6: Emphysema – Prevalence Rates per 1,000, 2011 Table 4: Emphysema – Number of Conditions and Prevalence Rate per 1,000 Population by Ethnic Origin, Sex and Age, 1997-2011 Table 5: COPD – Adult Prevalence by Sex and State, 2011 Figure 8: COPD – Age-Adjusted Prevalence in Adults by State, 2011 Table 6: Characteristics Among Those Reporting a Diagnosis of COPD by State (%), 2011 Figure 9: COPD – First-Listed Hospital Discharge Rates per 10,000, 2010 Table 7: COPD – Number of First-Listed Hospital Discharges and Rate per 10,000 Population by Race, Sex and Age, 1999-2010 Figure 9: National Projected Annual Cost of COPD, 2010 Introduction Chronic obstructive pulmonary disease (COPD) is a term which refers to a large group of lung diseases characterized by obstruction of air flow that interferes with normal breathing. -
Chronic Obstructive Lung Disease &Bronchiectasis
PLEASE CHECK Editing file BEFORE! Chronic Obstructive lung Disease & Bronchiectasis ★ Objectives: 1. Definition of the two conditions 2. Clinical and radiological diagnosis 3. Differential diagnosis 4. General outline of management 5. Create a link to 341 clinical teaching ★ Resources Used in This lecture: Davidson, Guyton and Becker step 1 lecture notes Done by: Mohammad Alkharraz Contact us at: [email protected] Chronic Obstructive Pulmonary Diseases (COPD) COPD contains two diseases which are chronic bronchitis and emphysema ■ COPD is classified under obstructive pulmonary diseases along with other (no kidding!) diseases such as asthma and bronchiectasis ■ Chronic bronchitis and emphysema are grouped together under COPD because they are both mainly caused by smoking and they usually present together. ■ Brainless pathology textbooks (Robbins) try to confuse us students with “Pink Puffers” and “Blue Bloaters”. Forget about that as it is not clinically relevant1. Let us quickly point out some points (pathology) that are relevant to each disease (chronic bronchitis and emphysema) and then we will discuss the clinical presentation, management, etc. of COPD Chronic bronchitis It is mainly a clinical diagnosis patients cough up lots of sputum for a long period of time “3 months per year for at least 2 consecutive years2” ● Pathogenesis: Cigarette smoke causes hyperplasia of mucus glands which increase the secretion of mucus → mucus plugs cause obstruction of bronchioles→ COPD Emphysema It is mainly a pathological diagnosis. ● Pathogenesis: 1. Pollutants (smoking)→ increased inflammatory mediators in the lung that destroy the lung parenchyma (trypsin and elastase) 2. We have defense mechanisms to fight these inflammatory mediators (alpha1 antitrypsin) ○ However, the amount of inflammatory mediators exceeds our ability to counteract them 3. -

Podiums France
PODIUMS FRANCE : ANNEE 1990 : VILLETANEUSE (93) CS Villetaneuse le 6/01 : Cyclo – cross seniors 1 et Pro : 2ème Thierry Casas, CM Aubervilliers. BOIS D’ARCY (78) le 7/01 : Cyclo – cross seniors toutes catégories : 2ème Albert Pioline, CM Aubervilliers. CAP D’AGDE (Hérault) le 14/01 : « Championnats de France Cyclo cross Amateurs » : Argent : Thierry Casas, CM Aubervilliers. NOINTEL (95) le 20/01 : Cyclo – cross seniors toutes catégories : 2ème Thierry Casas, CM Aubervilliers. ISSOU (78) le 21/01 : Cyclo – cross toutes catégories : 1er Thierry Casas, 3ème Albert Pioline, tous les 2 du CM Aubervilliers. MELUN (77) le 27/01 : Cyclo – cross seniors toutes catégories : 2ème Yves Auvroin, CM Aubervilliers. LE MEE (77) le 4/02 : Cyclo – cross seniors toutes catégories : 2ème Mieczyslaw Korycki, 3ème Thierry Casas, CM Aubervilliers. CHAMPAGNE SUR OISE (95) le 11/02 : Cyclo – cross seniors toutes catégories : 3ème Thierry Casas, CM Aubervilliers. TORCY (77) le 17/02 : Cyclo – cross seniors toutes catégories : 2ème Yves Auvroin, CM Aubervilliers. CIRCUIT DES PLAGES VENDEENNES du 18/02 au 1/03 : Route Nationale : 1er au général : Hervé Boussard, CM Aubervilliers et vainqueur de la 5ème étape. 1er PARIS – COULOMMIERS (77) le 11/03 : Féminines toutes catégories : 1ère Corinne Le Gal, CC La Courneuve. SAINT PATHUS (77) le 18/03 : Féminines toutes catégories : 3ème Corinne Le Gal, CC La Courneuve. VENEUX LES SABLONS (77) le 1/04 : Féminines toutes catégories : 2ème Corinne Le Gal, CC La Courneuve. GRAND PRIX DE BOULOGNE (92) le 8/04 : Route Nationale : 3ème Hervé Boussard, CM Aubervilliers. VILLENEUVE LA GARENNE (92) le 15/04 : Féminines toutes catégories : 1ère Corinne Le Gal, CC La Courneuve. -
General Vertical Files Anderson Reading Room Center for Southwest Research Zimmerman Library
“A” – biographical Abiquiu, NM GUIDE TO THE GENERAL VERTICAL FILES ANDERSON READING ROOM CENTER FOR SOUTHWEST RESEARCH ZIMMERMAN LIBRARY (See UNM Archives Vertical Files http://rmoa.unm.edu/docviewer.php?docId=nmuunmverticalfiles.xml) FOLDER HEADINGS “A” – biographical Alpha folders contain clippings about various misc. individuals, artists, writers, etc, whose names begin with “A.” Alpha folders exist for most letters of the alphabet. Abbey, Edward – author Abeita, Jim – artist – Navajo Abell, Bertha M. – first Anglo born near Albuquerque Abeyta / Abeita – biographical information of people with this surname Abeyta, Tony – painter - Navajo Abiquiu, NM – General – Catholic – Christ in the Desert Monastery – Dam and Reservoir Abo Pass - history. See also Salinas National Monument Abousleman – biographical information of people with this surname Afghanistan War – NM – See also Iraq War Abousleman – biographical information of people with this surname Abrams, Jonathan – art collector Abreu, Margaret Silva – author: Hispanic, folklore, foods Abruzzo, Ben – balloonist. See also Ballooning, Albuquerque Balloon Fiesta Acequias – ditches (canoas, ground wáter, surface wáter, puming, water rights (See also Land Grants; Rio Grande Valley; Water; and Santa Fe - Acequia Madre) Acequias – Albuquerque, map 2005-2006 – ditch system in city Acequias – Colorado (San Luis) Ackerman, Mae N. – Masonic leader Acoma Pueblo - Sky City. See also Indian gaming. See also Pueblos – General; and Onate, Juan de Acuff, Mark – newspaper editor – NM Independent and -

Team Dimension Data an Post Chain Reaction Orica
Team Dimension Data An Post Chain Reaction Orica BikeExchange Roger Hammond Kurt Bogaerts Matthew Wilson 1 Mark Cavendish GBR 71 Nicolas Vereecken BEL 141 Caleb Ewan AUS 2 Steve Cummings GBR 72 Japer Bovenhuis NED 142 Alex Edmondson AUS 3 Bernhard Eisel AUT 73 Emiel Wastyn BEL 143 Michael Hepburn AUS 4 Mark Renshaw AUS 74 Oliver Kent-Spark AUS 144 Luka Mezgec SLO 5 Jay Robert Thomson RSA 75 Jacob Scott GBR 145 Robert Power AUS 6 Johann Van Zyl RSA 76 Damien Shaw IRL 146 Amets Txurruka ESP Team Sky Cannondale Drapac Pro Cycling Wanty Group Gobert Kurt Arvesen Eric Van Lancker Steven De Neef 11 Elia Viviani ITA 81 Jack Bauer NZL 151 Mark McNally GBR 12 Ian Stannard GBR 82 Dylan Van Baarle NED 152 Enrico Gasparotto ITA 13 Wout Poels NED 83 Sebastian Langeveld NED 153 Marco Marcato ITA 14 Nicolas Roche IRL 84 Ryan Mullen IRL 154 Guillaume Martin FRA 15 Ben Swift GBR 85 Wouter Wippert NED 155 Xandro Meurisse BEL 16 Danny Van Poppel NED 86 Ruben Zepuntke GER 156 Bjorn Thurau GER Team WIGGINS Caja Rural - Seguros RGA Madison Genesis Simon Cope Jose Miguel Fernandez Mike Northey 21 Sir Bradley Wiggins GBR 91 Carlos Barbero ESP 161 Erick Rowsell GBR 22 Jonathan Dibben GBR 92 Miguel Ángel Benito ESP 162 Alexandre Blain FRA 23 Owain Doull GBR 93 Javier Francisco Aramendia ESP 163 Taylor Gunman NZL 24 Mark Christian GBR 94 Andre Domingos Goncalez POR 164 Matt Holmes GBR 25 Chris Latham GBR 95 Diego Rubio ESP 165 Matt Cronshaw GBR 26 Daniel Pearson GBR 96 Héctor Saez ESP 166 Tom Stewart GBR Etixx Quick-Step Great Britain Team Giant Alpecin Brian Holm -

Allergic Bronchopulmonary Aspergillosis As a Cause of Bronchial Asthma in Children
Egypt J Pediatr Allergy Immunol 2012;10(2):95-100. Original article Allergic bronchopulmonary aspergillosis as a cause of bronchial asthma in children Background: Allergic bronchopulmonary aspergillosis (ABPA) occurs in Dina Shokry, patients with asthma and cystic fibrosis. When aspergillus fumigatus spores Ashgan A. are inhaled they grow in bronchial mucous as hyphae. It occurs in non Alghobashy, immunocompromised patients and belongs to the hypersensitivity disorders Heba H. Gawish*, induced by Aspergillus. Objective: To diagnose cases of allergic bronchopulmonary aspergillosis among asthmatic children and define the Manal M. El-Gerby* association between the clinical and laboratory findings of aspergillus fumigatus (AF) and bronchial asthma. Methods: Eighty asthmatic children were recruited in this study and divided into 50 atopic and 30 non-atopic Departments of children. The following were done: skin prick test for aspergillus fumigatus Pediatrics and and other allergens, measurement of serum total IgE, specific serum Clinical Pathology*, aspergillus fumigatus antibody titer IgG and IgE (AF specific IgG and IgE) Faculty of Medicine, and absolute eosinophilic count. Results: ABPA occurred only in atopic Zagazig University, asthmatics, it was more prevalent with decreased forced expiratory volume Egypt. at the first second (FEV1). Prolonged duration of asthma and steroid dependency were associated with ABPA. AF specific IgE and IgG were higher in the atopic group, they were higher in Aspergillus fumigatus skin Correspondence: prick test positive children than negative ones .Wheal diameter of skin prick Dina Shokry, test had a significant relation to the level of AF IgE titer. Skin prick test Department of positive cases for aspergillus fumigatus was observed in 32% of atopic Pediatrics, Faculty of asthmatic children. -

Martian Crater Morphology
ANALYSIS OF THE DEPTH-DIAMETER RELATIONSHIP OF MARTIAN CRATERS A Capstone Experience Thesis Presented by Jared Howenstine Completion Date: May 2006 Approved By: Professor M. Darby Dyar, Astronomy Professor Christopher Condit, Geology Professor Judith Young, Astronomy Abstract Title: Analysis of the Depth-Diameter Relationship of Martian Craters Author: Jared Howenstine, Astronomy Approved By: Judith Young, Astronomy Approved By: M. Darby Dyar, Astronomy Approved By: Christopher Condit, Geology CE Type: Departmental Honors Project Using a gridded version of maritan topography with the computer program Gridview, this project studied the depth-diameter relationship of martian impact craters. The work encompasses 361 profiles of impacts with diameters larger than 15 kilometers and is a continuation of work that was started at the Lunar and Planetary Institute in Houston, Texas under the guidance of Dr. Walter S. Keifer. Using the most ‘pristine,’ or deepest craters in the data a depth-diameter relationship was determined: d = 0.610D 0.327 , where d is the depth of the crater and D is the diameter of the crater, both in kilometers. This relationship can then be used to estimate the theoretical depth of any impact radius, and therefore can be used to estimate the pristine shape of the crater. With a depth-diameter ratio for a particular crater, the measured depth can then be compared to this theoretical value and an estimate of the amount of material within the crater, or fill, can then be calculated. The data includes 140 named impact craters, 3 basins, and 218 other impacts. The named data encompasses all named impact structures of greater than 100 kilometers in diameter. -

Startnummer Naam 161 ADAM YATES 72 ALBERTO BETTIOL 91
Startnummer Naam 161 ADAM YATES 72 ALBERTO BETTIOL 91 ALEJANDRO VALVERDE 112 ALESSANDRO DE MARCHI 135 ALEXANDER KRISTOFF 146 ALEXEY LUTSENKO 38 ALEXIS VUILLERMOZ 13 AMUND GRØNDAHL JANSEN 172 ANDRÉ GREIPEL 2 ANDREY AMADOR 126 ANTHONY PEREZ 188 ANTHONY TURGIS 104 BAUKE MOLLEMA 173 BEN HERMANS 33 BENOIT COSNEFROY 47 BOB JUNGELS 211 BRYAN COQUARD 151 CALEB EWAN 98 CARLOS VERONA 207 CASPER PHILLIP PEDERSEN 203 CEES BOL 125 CHRISTOPHE LAPORTE 166 CHRISTOPHER JUUL JENSEN 87 CLÉMENT RUSSO 37 CLÉMENT VENTURINI 88 CONNOR SWIFT 212 CYRIL BARTHE 215 CYRIL GAUTIER 63 DAMIANO CARUSO 76 DANIEL FELIPE MARTINEZ 171 DANIEL MARTIN 26 DANIEL OSS 92 DARIO CATALDO 165 DARYL IMPEY 133 DAVID DE LA CRUZ 53 DAVID GAUDU 134 DAVIDE FORMOLO 85 DAYER QUINTANA 86 DIEGO ROSA 197 DOMENICO POZZOVIVO 46 DRIES DEVENYNS 8 DYLAN VAN BAARLE 192 EDVALD BOASSON HAGEN 108 EDWARD THEUNS 1 EGAN BERNAL 128 ELIA VIVIANI 22 EMANUEL BUCHMANN 94 ENRIC MAS 164 ESTEBAN CHAVES 185 FABIEN GRELLIER 132 FABIO ARU 23 FELIX GROSSSCHARTNER 156 FREDERIK FRISON 187 GEOFFREY SOUPE 12 GEORGE BENNETT 191 GIACOMO NIZZOLO 144 GORKA IZAGUIRRE INSAUSTI 111 GREG VAN AVERMAET 25 GREGOR MÜHLBERGER 121 GUILLAUME MARTIN 176 GUY NIV 148 HAROLD TEJADA 73 HUGH JOHN CARTHY 174 HUGO HOFSTETTER 143 HUGO HOULE 118 ILNUR ZAKARIN 93 IMANOL ERVITI 145 ION IZAGUIRRE INSAUSTI 162 JACK BAUER 114 JAN HIRT 138 JAN POLANC 153 JASPER DE BUYST 107 JASPER STUYVEN 214 JENS DEBUSSCHERE 75 JENS KEUKELEIRE 184 JÉRÔME COUSIN 124 JESUS HERRADA 155 JOHN DEGENKOLB 115 JONAS KOCH 4 JONATHAN CASTROVIEJO 206 JORIS NIEUWENHUIS 96 JOSÉ ROJAS -

C 367 Jornal Oficial
Jornal Oficial C 367 da União Europeia 57.º ano Edição em língua portuguesa Comunicações e Informações 16 de outubro de 2014 Índice IV Informações INFORMAÇÕES DAS INSTITUIÇÕES, ÓRGÃOS E ORGANISMOS DA UNIÃO EUROPEIA Parlamento Europeu PERGUNTAS ESCRITAS E SUA RESPOSTA 2014/C 367/01 Perguntas escritas apresentadas por deputados ao Parlamento Europeu e respetiva resposta dada por uma instituição da União Europeia ......................................................................................................................... 1 (Ver nota ao leitor) PT Nota ao leitor A presente publicação contém perguntas escritas apresentadas por deputados ao Parlamento Europeu e a respetiva resposta dada por uma instituição da União Europeia. Para cada pergunta e resposta é apresentada, antes de uma eventual tradução, a versão na língua original. Por vezes, a resposta pode ser dada numa língua que não seja a da pergunta. Isto depende da língua de trabalho da comissão a quem é requerida a resposta. Estas perguntas e respostas são publicadas nos termos dos artigos 117.º e 118.º do Regimento do Parlamento Europeu. Todas as perguntas e respostas são acessíveis através do website do Parlamento Europeu (Europarl) na rubrica «Perguntas parlamentares»: http://www.europarl.europa.eu/plenary/pt/parliamentary-questions.html SIGNIFICADO DAS SIGLAS DOS GRUPOS POLÍTICOS PPE Grupo do Partido Popular Europeu (Democratas-Cristãos) S&D Grupo da Aliança Progressista dos Socialistas e Democratas no Parlamento Europeu ALDE Grupo da Aliança dos Democratas e Liberais pela -

224641234.Pdf
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Helsingin yliopiston digitaalinen arkisto ASTROBIOLOGY Volume 19, Number 3, 2019 Mary Ann Liebert, Inc. DOI: 10.1089/ast.2018.1870 A Low-Diversity Microbiota Inhabits Extreme Terrestrial Basaltic Terrains and Their Fumaroles: Implications for the Exploration of Mars Charles S. Cockell,1 Jesse P. Harrison,2,3 Adam H. Stevens,1 Samuel J. Payler,1 Scott S. Hughes,4 Shannon E. Kobs Nawotniak,4 Allyson L. Brady,5 R.C. Elphic,6 Christopher W. Haberle,7 Alexander Sehlke,6 Kara H. Beaton,8 Andrew F.J. Abercromby,9 Petra Schwendner,1 Jennifer Wadsworth,1 Hanna Landenmark,1 Rosie Cane,1 Andrew W. Dickinson,1 Natasha Nicholson,1 Liam Perera,1 and Darlene S.S. Lim6,10 Abstract A major objective in the exploration of Mars is to test the hypothesis that the planet hosted life. Even in the absence of life, the mapping of habitable and uninhabitable environments is an essential task in developing a complete understanding of the geological and aqueous history of Mars and, as a consequence, understanding what factors caused Earth to take a different trajectory of biological potential. We carried out the aseptic collection of samples and comparison of the bacterial and archaeal communities associated with basaltic fumaroles and rocks of varying weathering states in Hawai‘i to test four hypotheses concerning the diversity of life in these environments. Using high-throughput sequencing, we found that all these materials are inhabited by a low-diversity biota. Multivariate analyses of bacterial community data showed a clear separation between sites that have active fumaroles and other sites that comprised relict fumaroles, unaltered, and syn-emplacement basalts. -
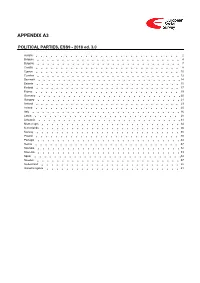
ESS9 Appendix A3 Political Parties Ed
APPENDIX A3 POLITICAL PARTIES, ESS9 - 2018 ed. 3.0 Austria 2 Belgium 4 Bulgaria 7 Croatia 8 Cyprus 10 Czechia 12 Denmark 14 Estonia 15 Finland 17 France 19 Germany 20 Hungary 21 Iceland 23 Ireland 25 Italy 26 Latvia 28 Lithuania 31 Montenegro 34 Netherlands 36 Norway 38 Poland 40 Portugal 44 Serbia 47 Slovakia 52 Slovenia 53 Spain 54 Sweden 57 Switzerland 58 United Kingdom 61 Version Notes, ESS9 Appendix A3 POLITICAL PARTIES ESS9 edition 3.0 (published 10.12.20): Changes from previous edition: Additional countries: Denmark, Iceland. ESS9 edition 2.0 (published 15.06.20): Changes from previous edition: Additional countries: Croatia, Latvia, Lithuania, Montenegro, Portugal, Slovakia, Spain, Sweden. Austria 1. Political parties Language used in data file: German Year of last election: 2017 Official party names, English 1. Sozialdemokratische Partei Österreichs (SPÖ) - Social Democratic Party of Austria - 26.9 % names/translation, and size in last 2. Österreichische Volkspartei (ÖVP) - Austrian People's Party - 31.5 % election: 3. Freiheitliche Partei Österreichs (FPÖ) - Freedom Party of Austria - 26.0 % 4. Liste Peter Pilz (PILZ) - PILZ - 4.4 % 5. Die Grünen – Die Grüne Alternative (Grüne) - The Greens – The Green Alternative - 3.8 % 6. Kommunistische Partei Österreichs (KPÖ) - Communist Party of Austria - 0.8 % 7. NEOS – Das Neue Österreich und Liberales Forum (NEOS) - NEOS – The New Austria and Liberal Forum - 5.3 % 8. G!LT - Verein zur Förderung der Offenen Demokratie (GILT) - My Vote Counts! - 1.0 % Description of political parties listed 1. The Social Democratic Party (Sozialdemokratische Partei Österreichs, or SPÖ) is a social above democratic/center-left political party that was founded in 1888 as the Social Democratic Worker's Party (Sozialdemokratische Arbeiterpartei, or SDAP), when Victor Adler managed to unite the various opposing factions. -

March 21–25, 2016
FORTY-SEVENTH LUNAR AND PLANETARY SCIENCE CONFERENCE PROGRAM OF TECHNICAL SESSIONS MARCH 21–25, 2016 The Woodlands Waterway Marriott Hotel and Convention Center The Woodlands, Texas INSTITUTIONAL SUPPORT Universities Space Research Association Lunar and Planetary Institute National Aeronautics and Space Administration CONFERENCE CO-CHAIRS Stephen Mackwell, Lunar and Planetary Institute Eileen Stansbery, NASA Johnson Space Center PROGRAM COMMITTEE CHAIRS David Draper, NASA Johnson Space Center Walter Kiefer, Lunar and Planetary Institute PROGRAM COMMITTEE P. Doug Archer, NASA Johnson Space Center Nicolas LeCorvec, Lunar and Planetary Institute Katherine Bermingham, University of Maryland Yo Matsubara, Smithsonian Institute Janice Bishop, SETI and NASA Ames Research Center Francis McCubbin, NASA Johnson Space Center Jeremy Boyce, University of California, Los Angeles Andrew Needham, Carnegie Institution of Washington Lisa Danielson, NASA Johnson Space Center Lan-Anh Nguyen, NASA Johnson Space Center Deepak Dhingra, University of Idaho Paul Niles, NASA Johnson Space Center Stephen Elardo, Carnegie Institution of Washington Dorothy Oehler, NASA Johnson Space Center Marc Fries, NASA Johnson Space Center D. Alex Patthoff, Jet Propulsion Laboratory Cyrena Goodrich, Lunar and Planetary Institute Elizabeth Rampe, Aerodyne Industries, Jacobs JETS at John Gruener, NASA Johnson Space Center NASA Johnson Space Center Justin Hagerty, U.S. Geological Survey Carol Raymond, Jet Propulsion Laboratory Lindsay Hays, Jet Propulsion Laboratory Paul Schenk,